Causes
There are a number of main factors of accessory pancreatitis of the pancreatic duct that influence its development.
Despite disagreements on the part of specialists dealing with the issue, one thing is certain - the accessory gland is laid in utero. Several main factors contribute to this process. Genetic diseases play a significant role in the development of an aberrant pancreas. Malfunctions occur in the genetic apparatus of cells. The failure is mostly observed at the gene level. The factor of a woman’s behavior in her position plays a huge role. Has a great impact:
- smoking tobacco products during pregnancy. The same applies to the use of narcotic drugs during this period;
- the risk is present when exposed to physical factors. This implies an increase in body temperature and possible exposure to radiation;
- with increased neuropsychological stress and exposure to stressful situations, this phenomenon is also observed.
Doctors often emphasize to pregnant women that they should not take certain medications. This can be explained by the risk of pathological processes and malfunctions in the genetic apparatus
Important. The development of the disease is provoked by an infectious disease suffered by the mother during pregnancy.
This may be rubella, the main manifestations of which are red rashes. The place of their localization is the front part, the body.
The disease is provoked by syphilis, which is sexually transmitted. With viral diseases, for example, with herpes, a similar reaction of the body is observed.
Another provoking disease is listeriosis. The disease affects the lymphatic tissue, liver, and other organs.
Symptoms of the disease
Clinical manifestations of the presence of an aberrant pancreas depend on its size and location. If it is located in the area of the stomach walls, then the symptoms are very similar to the manifestations of gastritis, and if it is located in the area of the duodenum, then in this case the manifestations may indicate the development of an ulcer. In addition, signs may appear indicating pancreatitis, cholecystitis or appendicitis. These signs do not force the patient to see a doctor, and the pathology may not be detected for a long time.
Treatment
If an aberrant pancreas is detected, treatment may not be carried out in the absence of symptoms, if it does not bother the patient and does not harm a nearby organ. But it requires a mandatory detailed examination and constant monitoring to prevent tissue malignancy. When an anomaly is detected, studies are needed to exclude the development of a malignant formation. If everything is normal, then the operation is postponed, and the patient undergoes regular examinations: ultrasound (every year) and other procedures.
If an ectopic organ is accompanied by a pathological process, surgical intervention is prescribed, the method of which is determined by a specialist depending on the location of the anomaly. For a superficial location (in the wall of the gastric antrum, in the duodenum), endoscopic electroexcision is used, which consists of cutting off the polyp with soft or hard diathermic loops.
In some cases, abdominal surgery may be prescribed, accompanied by opening the peritoneal wall and layer-by-layer resection of a certain part of the stomach. Less traumatic is endoscopic minilaparotomy, which involves creating an anastomosis between the abnormal formation and the anatomical gland. If there are cysts (often large) in the organ, they are fenestrated.
Possible complications
If you ignore and do not observe the “accessory” gland, it can lead to gastric and intestinal bleeding, pancreatitis (if it is inflamed), intestinal obstruction of various stages, stenosis of the gastrointestinal tract and even the development of a malignant tumor.
As for preventive measures, only one thing can be said: if it does not interfere with a full life and does not threaten health, then in any case constant monitoring is required. In addition, a special diet, taking medications that help absorb and digest food, and giving up bad habits are recommended.
Prevention of complications from the accessory gland
If there is an accessory gland, then its further development must be monitored regularly. To prevent it from causing a lot of complications, prevention is necessary:
- Stick to a diet: add more easily digestible protein and fiber-enriched foods to your diet. A minimum of fat and nothing that would increase appetite.
- Take medications that help the digestion process, for example, Creon in the form of mini-microspheres. Capsules are easily mixed in the stomach with food and penetrate into the intestines. This is necessary in the absence of the production of its own enzymes.
- Quitting smoking and alcohol.
If you follow the recommendations and are constantly monitored by a doctor, the additional gland will not cause any inconvenience. In any case, constant monitoring by a specialist is necessary in order to promptly identify complications and take the necessary measures.
Treatment
Doctors identify only one method of treatment - the use of surgery. It is worth noting that the type of surgery performed depends on various clinical signs. The location of the abnormal formation and the presence or absence of any symptoms also matter. Thanks to the use of this treatment method, it is possible to confirm or refute the possibility of a malignant formation.
Surgery is postponed if the abnormal formation does not bother the patient in any way. In this case, they regularly monitor their health. For this, the patient is shown ultrasound and additional diagnostic methods.
In all other cases, diagnosis is needed, then surgery.
Today, the use of abdominal operations is practiced. In this case, the observation is controlled by a doctor, and the patient remains in the hospital for a long period of time. The following methods of surgical intervention are distinguished:
- An autopsy is performed in the abdominal wall. This is an abdominal operation.
- Endoscopic minilaparotomy is less damaging to a person.
- Another method is to use endoscopic, low-traumatic surgery. It is carried out with special equipment - an electrocoagulator.
A special feature of the second method is that the doctor makes a minimal incision in the abdominal wall. An option with a more extensive dissection is also possible. The operation is carried out using video surveillance. Thus, the surgical area can be sufficiently examined and the operation of surgical instruments can be monitored.
The authors have introduced an innovative way to treat the abnormal formation. Using basic diagnostic techniques, the doctor clarifies the boundaries of the surgical field. Next, an electrocoagulator is passed into the canal through the gland duct. Then the formation is destroyed layer by layer.
At the end of the procedure, nitric oxide is applied to the affected area. Its use promotes rapid healing of wounds and restoration of damaged areas. As a result, a postoperative scar is formed and the risk of future complications is minimized. The procedure is carried out under the supervision of a doctor, medical personnel and under the supervision of an endoscope.
The use of medications reduces the production of hydrochloric acid. This complex is used in the diagnosis of pancreatitis, chronic gastritis, and ulcers.
How to diagnose the disease?
Pathology can be detected using different methods, it all depends on its location. If the aberrant lobule of the pancreas is located on the wall of the duodenum, in the large intestine or stomach, then in this case it will not be difficult to identify it. In most cases, it is detected during a screening test. The age of patients who are most often diagnosed with the disease is 40-70 years.
An anomaly can be detected using several methods:
Endoscopic. In this case, the gland is a large island of glandular tissue, often resembling a polyp, which is located on a broad base. Often there may be a depression at the top of such an island, which is an endoscopic sign of an aberrant gland. If a superficial biopsy is taken during this study, it will be difficult to obtain accurate data.
Diagnostics
In asymptomatic cases, anomalies are discovered by chance. If a developmental defect is suspected, a complex of laboratory and instrumental examination methods is performed. A general and biochemical blood test determines the level of enzymes, and stool analysis is indicated for the same purpose. Elevated blood glucose levels indicate a deficiency of the endocrine function of the pancreas. All developmental anomalies of the pancreas require radiological and endoscopic confirmation. Double-contrast radiography allows visualization of the duodenum and suspects an annular pancreas if intestinal stenosis occurs without changes in the structure of the mucous membrane.
Magnetic resonance cholangiopancreatography is used to diagnose the condition of the ducts. The method is highly informative and non-invasive. Abdominal ultrasound allows one to judge the position of the pancreas and neighboring organs, as well as identify congenital cysts and suspect areas of ectopic spleen tissue. Esophagogastroduodenoscopy is performed to assess the condition of the mucous membrane of the duodenum and duodenal papilla, as well as to obtain material for a biopsy. In addition, it is necessary to exclude the presence of aberrant glands in the intestinal wall, so endoscopic examination of the upper gastrointestinal tract is complemented by colonoscopy.
Location of the aberrant gland
The aberrant pancreas can be located in the stomach and other organs:
- esophagus;
- duodenum;
- the walls of the gallbladder;
- liver;
- spleen;
- small intestine;
- mesentery of the small intestine, in the fold or mucous membrane of the abdominal cavity.
Treatment of chronic inflammation
If the diagnosis of pancreatitis has revealed a chronic form of the disease, then patients can be prescribed various medications: enzyme preparations based on pancreatin (Mezim, Festal, Creon), antibiotics (Abaktal, Amoxiclav, Sumamed) etc. In some cases (for example, with a formed pseudocyst), minimally invasive (percutaneous) drainage or surgical intervention is required.
Nutrition plays an important role. If the disease worsens on the 1st or 2nd day, patients are prohibited from eating anything. You can only drink liquid (1-1.5 liters per day): weak tea, alkaline mineral water without carbon, rosehip decoction (1-2 glasses). On the 2-3rd day you are allowed to eat. Slimy soups, liquid pureed milk koshes, vegetable purees, and fruit juice jelly are allowed.
During periods of remission, you should adhere to the following tips:
- Steam, puree or bake food in the oven. Eliminate pure fats from the diet and limit table salt to 6 g per day.
- Eat small meals 5-6 times a day. The recommended temperature for hot dishes is no higher than 57-62 degrees, cold food - no less than 15-17 degrees.
- Exclude from the diet sour, spicy, spicy and canned foods, peas and beans, mushrooms, carbonated and alcoholic drinks, kvass, sour fruit juices, and baked goods. Cream and sour cream are allowed in small quantities in dishes.
What is the reason for the development of an aberrant gland?
Scientists have not yet figured out why the accessory pancreatic duct is formed in the human body. Only one thing can be said with certainty - this anomaly occurs in utero, and the following factors have a direct impact on the appearance of such a developmental defect in the unborn child:
- Negative effects of the environment on the pregnant woman’s body (radioactive or ultraviolet radiation, constant high temperature).
- Genetic diseases (violation of the correct set of genes in the cells of a developing organism).
- Bad habits of the mother during pregnancy (alcohol abuse, smoking, drug use).
- Prolonged stress, frequent depression.
- Various infectious diseases that the expectant mother suffered during pregnancy (herpes, rubella, syphilis, listeriosis, etc.).
- The use of certain medications during this period that are undesirable for pregnant women.
Mechanism of formation and causes
According to doctors, the reasons for the appearance of such an unusual organ are congenital anomalies . The mechanisms of formation are not fully understood. Provoking factors that influence the appearance of a congenital defect in the fetus are considered:
- genetic mutations;
- radiation exposure;
- taking certain medications during pregnancy;
- stress;
- bad ecology;
- drug use, smoking, alcohol;
- viral diseases: rubella, measles, herpes, toxoplasmosis;
- listeriosis bacterium.
Methods of treating acute pancreatitis
If symptoms indicating the development of AP occur, the sick person should receive first aid:
- prohibit eating and drinking for several days;
- apply a heating pad with cold water or an ice pack to the epigastric area;
- give antispasmodics (thanks to the use of “No-shpa” or “Papaverine”, the production of enzymes will decrease).
After providing first aid, you must immediately call a doctor. The person must be hospitalized in a hospital. The hospital immediately performs an ultrasound diagnosis of acute pancreatitis. After an accurate diagnosis has been established, analgesics (Baralgin, Analgin) are prescribed to suppress pain.
Solutions of amino acids and glucose are also used in treatment. They replenish the plastic and energy needs of the human body. Antibiotics are also prescribed. These drugs are necessary for the treatment and prevention of purulent complications.
A few days after the start of treatment, a thin probe is installed in the small intestine. It is necessary for the use of enteral nutrition techniques. When intestinal function is restored, the patient is allowed to eat naturally. The diet should consist of cereals, boiled vegetables, and compotes.
Conservative treatment is successful in 87% of cases. The remaining 13% of sick people require surgery. It is carried out when the diagnosis of pancreatitis reveals serious complications. The goals of surgical treatment are as follows:
- Reducing endotoxicosis. For this purpose, drainage and decompression of the bile ducts, drainage and sanitation of the abdominal cavity are prescribed. During the operation, enzymes, toxins and other biologically active substances are removed from the body.
- Treatment of infectious and necrotic complications of pancreatic necrosis (abscesses, fistulas, cysts, peritonitis). To achieve this goal, specialists perform opening and drainage of post-necrotic, purulent cavities, resection and sequestrectomy of the pancreas.
Symptoms
The severity of clinical symptoms with an aberrant pancreas depends on its location and size. Manifestations of this anomaly occur with the development of complications. With this course, the patient develops signs of gastritis, peptic ulcer, pancreatitis, cholecystitis or appendicitis. In other cases, the accessory pancreas does not manifest itself in any way and is detected by chance during examinations for other diseases or during preventive examinations.
If the aberrant gland is located in the gastroduodenal zone and is capable of producing pancreatic juice, then the patient experiences the following symptoms:
- pain (from minor to severe, as with a peptic ulcer);
- abdominal cramps;
- indigestion;
- belching sour or bitter;
- nausea and vomiting;
- weight loss;
- formation of erosions on the mucous membrane of the stomach or duodenum.
Subsequently, the disease can lead to the development of gastrointestinal bleeding, perforation, penetration or malignancy of the ulcer.
If the aberrant gland compresses the extrahepatic bile ducts, the patient develops obstructive jaundice. When the accessory gland is localized in the small intestine, its complicated course can lead to the development of intestinal obstruction. If the aberrant pancreas is located in Meckel's diverticulum, then the patient experiences manifestations of acute appendicitis.
In some cases, the accessory pancreas occurs under the masks of the following diseases:
- gastritis;
- polyposis of the stomach or intestines;
- pancreatitis (or cholecystopancreatitis).
Malignancy of the aberrant pancreas is rare. Typically, adenocarcinomas located in the submucosal layer can develop in its place. Later, the tumor spreads to the mucous membrane and ulcerates. At this stage of the cancer process, it is difficult to distinguish it from ordinary adenocarcinoma.
What is pathology
An aberrant pancreas is an abnormality in the development of an accessory organ to a specific normal organ. Its tissues are identical to the tissues of the organ to which it is adjacent. It occurs near a certain organ of the human body (gastric wall, antral region of the gastrointestinal tract, duodenum, small intestine, mesentery) and does not have vascular and anatomical continuity with it. Its structure is the same as that of a normal one; it has its own aberrant pancreatic duct, which opens into the intestinal lumen.
Types of histology
There are three types of aberrant glands:
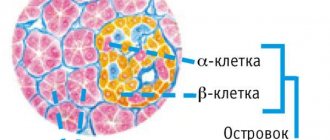
- type I: with typical lobular tissue, duct and islets, similar to cells of a normal organ;
- type II: with tissue including acini, ducts, excluding islets;
- type III: characterized by the presence of excretory ducts only.
We recommend finding out why you may feel sick in the morning.
Read: how psychosomatics explains the occurrence of pancreatitis.
Causes
Even modern medicine cannot name the exact reasons for the occurrence of an abnormal formation. Its formation occurs in utero, so it is a congenital pathology. There are suggestions that genetic factors, bad habits and severe stress during pregnancy, and infectious diseases of a pregnant woman such as rubella, listeriosis, syphilis, measles, and herpes can contribute to the development. There is also a risk of occurrence if, while carrying a child, radiation exposure was carried out and drugs were taken that are contraindicated during this period.
Symptoms
The clinical picture is completely determined by the location of the pathology. So, if the wall of the stomach is affected, the symptoms are similar to those of gastritis; if an anomaly develops in the duodenum, the symptoms resemble an ulcer. But often the aberrant pancreas, including the antrum of the stomach, does not show any symptoms.
As a rule, the patient complains in the event of the development of certain complications: inflammatory processes, bleeding, intestinal obstruction, including constipation, necrosis, perforation of the stomach walls. In one of these cases, abdominal pain, difficulties with digestion, vomiting after eating, release of bile during vomiting, weight loss, and stenosis of the duodenum may be observed.
Reasons for appearance
The exact root causes are still unknown to medicine. Possibly occurs during fetal development. Most gastroenterologists are inclined to believe that organ growth is a congenital pathology.
One of the provocateurs is genetic predisposition
Possible provoking factors include:
- chronic herpes;
- hereditary predisposition;
- measles;
- presence of bad habits;
- syphilis;
- tumors in the gland or stomach;
- prolonged exposure to stress during pregnancy;
- listeriosis;
- rubella
It is important to know! A connection has been established between radiation exposure during pregnancy and pathology.
Sometimes an additional pancreas causes complications. These include:
- stenosis of the gastric pylorus, or intestine;
- degeneration of an organ into a cancerous tumor;
- development of acute pancreatitis;
- opening of bleeding (stomach, intestines);
- development of intestinal obstruction.
Complications may occur if the organ is located next to the small intestine. Against the background of the simultaneous development of the inflammatory process, the risk of developing dyspeptic disorders is high.