Benign formations are one of the most common findings during endoscopic examination of the large intestine. Such findings include a polyp of the sigmoid colon. Large formations in this area give pronounced symptoms, which become the reason for visiting a doctor.
Treatment of benign growths is carried out only surgically. In the sigmoid colon, they are removed endoscopically using a sigmoidoscope or colonoscope. Conservative therapy is used as a method of support - pain relief, stimulation of intestinal motility, prevention of infectious complications.
What is a sigmoid colon polyp
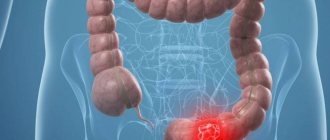
The sigmoid colon (doctors simply call it sigmoid) is part of the colon and directly passes into the rectum. Its peculiarity is that it is bent in two places (therefore it resembles the Latin letter S); accordingly, narrowings are formed in these places.
A polyp of the sigmoid colon is a benign formation that is located within its boundaries and originates from the tissues lining the intestines. Like growths of other parts of the intestine, sigma polyps give nonspecific symptoms - constipation, watery diarrhea, abdominal pain and blood in the stool.
Benign tumors of the sigmoid region should be treated immediately, since this area accounts for the majority of malignant tumors.
In addition, when a polyp is localized in the area of the sigmoidal angle, there is a risk of developing intestinal obstruction - a serious complication that requires emergency hospitalization.
Symptoms
At the initial stage of development of the pathological process, signs may be completely absent, which leads to delayed diagnosis and the development of associated complications.
Polyps of the sigmoid colon are characterized by the following symptoms:
- pain when sitting for a long time;
- blood and mucus in stool;
- pain during defecation;
- false urge to defecate;
- unstable stool - prolonged bouts of diarrhea can be alternated with equally prolonged constipation;
- increased gas formation;
- nausea, vomiting;
- heartburn, especially after eating fatty or heavy foods;
- weakness;
- especially large polyps can “fall out” from the anus.
It should be noted that pronounced symptoms are observed only in cases where the neoplasm reaches two centimeters or more.
In more complex cases, intestinal obstruction, muscle weakness, and elevated body temperature may be present.
Types and types of polyps
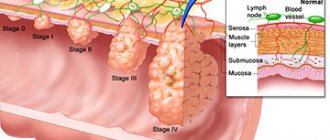
For classification, division according to histological principle is used. All polyps of the sigmoid colon can be divided into 3 types:
- epithelial (potentially malignant) – adenomatous formations and their subtypes;
- non-epithelial (with very low oncogenic potential) - hyperplastic, inflammatory, hamartomatous;
- submucosal non-epithelial (rare, have low oncogenic potential) – lipomas, leiomyomas.
4 types of formations make up the bulk of findings during endoscopy:
- tubular;
- tubular-villous;
- villous;
- hyperplastic.
The first three belong to the group of adenomatous (glandular) polyps, which are formed from the intestinal epithelium with an altered structure (which creates the preconditions for cancerous degeneration). In appearance, they resemble mushroom-shaped growths and have a pale tint, which makes them different from normal mucous membrane.
Villous tumors have a high rate of malignancy into adenocarcinoma - from 35 to 90%. More often they are found in the form of flat, hyperemic growths. They also secrete large amounts of fluid into the lumen of the organ, which causes watery diarrhea.
A hyperplastic polyp is an enlarged epithelial gland without a disrupted structure. Outwardly it looks like an unchanged protrusion of the mucous membrane. The chance of malignant degeneration is low - less than 1%. The malignant variant is serrated carcinoma, which is an extremely aggressive tumor. Therefore, formations larger than 1 cm are also removed.
A polyp that forms during prolonged inflammation of the mucous membrane is called inflammatory and is not considered oncogenic. But a large number of them can interfere with the passage of stool and cause bleeding.
When the mucosa heals, granulation polyps may appear, which also do not have oncogenic potential. But periodic monitoring and surgery are necessary if any symptoms appear.
Kinds
Depending on a number of features in medicine, there are different types of polyps that affect the mucous membrane of the sigmoid colon.
Some of them do not reach large sizes and manifest a number of symptoms in rare cases. But other types of formations can develop into cancer.
Hyperplastic
They are considered the most common, as they are found in most patients.
Hyperplastic type formations are usually no more than five millimeters and are light in color. In appearance they resemble flat plaques.
Against the background of the dark-colored mucosa, the formations are clearly visible. Over time, they manifest themselves with many symptoms, but despite this, in rare cases they degenerate into cancer. Pathology requires specialist supervision.
Adenomatous
They are the most dangerous type of sigmoid colon polyps, as they are prone to transformation into a malignant course.
They are considered a precancerous condition and require immediate treatment. Depending on the stage of development, formations can reach 1-5 cm.
This species is divided into several types, including villous, tubular and villous-tubular.
In the initial stages of formation they are asymptomatic. But over time, patients experience intestinal obstruction due to the large size of the formation.
In addition, villous polyps are often injured and accompanied by bleeding.
Diffuse
The main cause of occurrence is heredity. The formations are always multiple and are also observed in children and adults.
On this topic
- Digestive system
Differences between sigmoidoscopy and colonoscopy
- Natalya Gennadievna Butsyk
- December 9, 2021
A distinctive feature is rapid development and expansion. In certain cases, the presence of several hundred and even thousands of small neoplasms is observed.
Treatment depends on the type of polyps formed on the surface of the mucous membrane of the sigmoid colon.
Causes
There is no single etiological factor that would explain the appearance of single benign formations in the intestine.
The reasons for the formation of polyps in the sigmoid colon are associated with lifestyle, diet, and bad habits.
The main risk factors are:
- Inflammatory bowel diseases - infectious colitis, ulcerative colitis, Crohn's disease.
- Heredity - close relatives have a higher chance of developing polyps, especially with familial polyposis.
- Age – after 50 years, the risk of benign and malignant intestinal formations increases.
- Sedentary lifestyle – due to a sedentary lifestyle and physical inactivity, blood stagnation in the pelvis and local hemodynamic disturbances occur.
- Smoking and alcohol.
- Eating a lot of red meat, processed foods, and low fiber in the diet.
- Excess weight and often associated type 2 diabetes.
- Chronic stress and neurotic conditions.
- Anomalies of intestinal development - dolichosigma (elongated sigmoid colon).
A separate group are hereditary polyposis, the cause of which lies in genetic abnormalities. They are inherited, and their treatment often requires surgery in childhood - from periodic polypectomy to total removal of the large intestine.
Causes of the disease
Intestinal neoplasms are overgrown areas of the intestinal mucosa. They can be millimeter or centimeter in size. Colon tumors that continue to grow continuously for many years can develop into malignant tumors.
One or more polyps (polyposis) can form in the human body. Benign adenomas usually grow very slowly. If the tumors increase in size fairly quickly, the risk of developing colorectal carcinoma increases dramatically.
Various reasons are responsible for the development of polyps, including heredity. Poor nutrition is considered today to be the main cause of the formation of retcosigmoid formations, especially in industrialized countries. Too much animal fat in the diet (meat, sausages), lack of fiber, obesity, nicotine and alcohol contribute to the development of polyps of varying severity. If intestinal polyps are due to hereditary characteristics, the cause may be Gardner's syndrome, Cowden's syndrome or Pütz-Jeghers syndrome.
Adenomatous polyposis of the sigmoid and other parts of the colon is a hereditary disease that is caused by the malfunction of certain genes. Colon growths caused by Gardner's syndrome almost always cause colon cancer. Colorectal polyps and large brown spots on the limbs and mouth are signs of Pates-Jeghers syndrome. It is worth noting that with Cowden syndrome, other organs are affected, in addition to the intestines.
Symptoms
Symptoms of the presence of benign formations in the intestinal lumen are not specific and can only guide the doctor towards a particular pathology.
A polyp of the sigmoid colon can manifest itself with the following symptoms:
- Blood in stool. When the polyp is localized in the sigma, blood will be visible in the form of longitudinal stripes in the formed stool or present in the form of streaks. Less common is the discharge of unchanged blood (occurs with diarrhea); black feces are not typical for formations of the sigmoid region. Profuse bleeding occurs when a polyp is torn off.
- Changing the stool. Polyps of the sigmorectal angle are characterized by the appearance of constipation (due to the natural narrowing of the lumen in this place). Large villous tumors secrete mucus and fluid, causing diarrhea.
- Pain. Large formations can interfere with the movement of stool, causing discomfort. Pain often occurs due to spasm of smooth muscles, much less often due to ulceration of the polyp and its inflammation.
- Partial intestinal obstruction. Bloating, severe pain, nausea, scanty diarrhea - these symptoms periodically occur when a polyp blocks the intestinal lumen. This is typical for very large growths or long stalked polyps that extend into the rectum.
- General symptoms. The release of blood from a polyp in small quantities can occur for years and go unnoticed. Chronic bleeding is accompanied by loss of iron, which leads to the formation of iron deficiency anemia. Symptoms include general weakness, fatigue, hair loss, deformed nails, lip seals, and distorted taste. Symptoms of anemia are not specific, but should prompt the doctor to think about a possible cause of chronic blood loss.
In children, polyps can cause intussusception, which is accompanied by acute pain, vomiting, bleeding in the feces and the development of intestinal obstruction. Immediate hospitalization and surgical intervention are required.
There is a disease, there are no symptoms
Colon polyps are often asymptomatic, but can cause rectal bleeding, mucous discharge with feces, constipation or diarrhea, discomfort in the intestinal area, and rarely pain (without clear localization).
It should be borne in mind that a dangerous symptom - frequent rectal bleeding - may indicate a high risk of the polyp degenerating into a cancerous tumor. In this case, bleeding, as a rule, is chronic.
But these symptoms are not specific, that is, characteristic only of this disease. Diagnostics is of decisive importance.
Diagnostics
If a polyp is suspected in the sigmoid colon, the following studies are performed:
- Endoscopy. If a single growth is detected in the sigmoid region, all parts of the large intestine are checked to exclude other formations and anomalies (for example, diverticula). To do this, use a colonoscope or a shorter sigmoidoscope.
- Biopsy with histological examination. During a colonoscopy, a biopsy of a section of polyp tissue is performed, or the entire formation is sent for histological examination. Histological examination makes it possible to detect cancer cells at an early stage and decide on further surgery and chemotherapy.
- Radiation methods (CT, MRI). Sometimes polyps are discovered by chance, when the patient has completely different symptoms and the diagnosis of another disease requires the use of radiation methods. In routine practice, irrigoscopy (filling the intestine with a contrast agent and examination using an X-ray machine) can be used, but it is increasingly being replaced by endoscopic methods.
Due to its anatomical features, visualization of the sigmoid colon is possible only with the help of flexible endoscopes; other methods (digital examination, sigmoidoscopy) are not informative.
Important!
If a single polyp is detected, the entire large intestine must be examined.
How are intestinal polyps removed?
In most cases, the polyp can be removed during a colonoscopy with biopsy. The doctor inserts biopsy scissors or a special wire loop into the intestine and excises the tumor. Small polyps up to 5 mm in size can be removed entirely. Large ones are removed in pieces.
If there is a suspicion of malignant transformation, resection of the mucous membrane around the polyp is performed. All removed tissue is sent to the laboratory for histological and cytological examination.
If the polyp cannot be removed, the doctor must take a piece of tissue for a biopsy. Moreover, this must be done correctly, otherwise the laboratory will obtain a false negative result. The diagnosis will not be made in time, and time is a very important factor in the fight against cancer. The prognosis greatly depends on how early treatment is started.
Find out the exact cost of removing intestinal polyps
Surgical removal of a polyp in the sigmoid colon
In most cases, polyps in the sigmoid colon are removed endoscopically. Access to the surgical field depends on the size of the formation, the nature of the base (pedunculated, flat) and its location.
Table 1. Types of surgical approaches for the treatment of sigmoid colon polyps
| Type of access | Indications |
| Endoscopic | Includes methods of polyp removal using a cold loop, electrical excision and photodestruction (laser). This is the method of choice for polypectomy of small adenomatous and hyperplastic formations on the stalk. The least traumatic method, minimal likelihood of complications |
| Laparoscopic | Access is through punctures in the abdominal cavity. Large formations, such as villous polyps, are removed in this way. The rehabilitation period takes 2-4 days |
| Laparotomy | Opening the abdominal cavity. It is used rarely, mainly to remove large glandular flat polyps along with part of the intestine. Adenocarcinomas and other malignant tumors are removed laparotomically along with the affected organ and a local group of lymph nodes. Requires long-term rehabilitation in a hospital setting |
Removal of malignant formations includes more complex operations - dissection of the submucosal layer, partial resection of an organ or removal of part of the intestine. Also, the detection of cancer cells is the basis for prescribing additional examinations - CT/MRI with contrast, PET tomography, determination of tumor markers, immunohistochemistry. After the examination, the need for chemotherapy and radiation therapy is decided.
Conservative therapy includes the following groups of drugs:
- Antispasmodics (No-Shpa) are used to eliminate spastic pain. Narcotic analgesics (Tramadol, Morphine) are used after laparoscopic and laparotomy operations.
- Antibiotics (Alfa-Normix, Nifuroxazide) to prevent infectious complications. Systemic antibiotics (Ceftriaxone, Levofloxacin) are used for abdominal operations.
- Laxatives (Duphalac) for intestinal atony and constipation. For the same purpose, enemas are prescribed in the hospital.
- Carminatives (Espumizan) to reduce gas formation in the intestines.
- Vitamins (Milgamma) to accelerate tissue regeneration processes.
- Hemostatics (Ditsinon) for bleeding. Blood loss of up to 150 ml is considered physiological; in other cases, it is necessary to look for the cause and use hemostatic drugs.
Important!
Anticoagulants (Warfarin, Apixaban, Dabigatran) and NSAIDs are discontinued 3-4 days before surgery. The use of other medications must be agreed with your doctor.
Diet
Bowel preparation begins two days before endoscopic resection of the polyp. The following foods are excluded from the diet:
- vegetables and fruits in any form, mushrooms;
- cereals and whole grain products;
- dough, baked goods, flour products, bread;
- alcohol, canned food, spices.
Preparation is also carried out using cleansing preparations (Fortrans) and enemas according to special schemes, which are prescribed individually. Compliance with the rules of preparation for polypectomy is the most important prevention of complications.
Compliance with a slag-free diet after removal of a sigmoid colon polyp is prescribed for a period of 7 to 30 days, depending on the extent of the operation and the speed of rehabilitation of the patient. The list of prohibited foods remains the same as before preparing for the intervention. On the first day after surgery, it is recommended to consume fermented milk products without sugar (kefir, yogurt) and weak broths 5-6 times a day.
In the first days of the recovery period, boiled lean meat, sticky soups, and steamed omelettes can be introduced into the diet. On days 7-8, the menu is supplemented with mashed potatoes and white bread crumbs. From day 14 you can eat boiled porridge. It is better to eat meals in small portions to avoid high load on the intestines.
The disease can be prevented
A special focus of the work of the coloproctologist at ON CLINIC is preventive research. For this purpose, a colonoscopy is performed.
After 40-50 years, an examination by a coloproctologist is necessary once a year, a colonoscopy – once every three years. But you should approach this issue more individually.
It is necessary to undergo regular examinations at an earlier age:
- if the patient’s family had cases of polyps or colon cancer;
- if the patient was previously diagnosed with chronic intestinal disease;
- with eating disorders, sedentary lifestyle, frequent constipation;
- when discomfort in the intestinal area, pain and other unpleasant symptoms occur.
The basis for the prevention of colon cancer is the early detection of asymptomatic polyps and timely surgical treatment.
Any detected polyp requires, first of all, a thorough examination and subsequently immediate surgical intervention to avoid life-threatening complications.
Surgical treatment is carried out using endoscopic equipment, with the help of which the stalk of the polyp is captured and compressed. This is followed by a mandatory histological examination of the taken material.
Why is the formation of polyps in the sigmoid colon dangerous?
Polyp of the sigmoid colon threatens with the following complications:
- Oncology. Malignant degeneration of the polyp carries a mortal threat and requires removal of the entire sigmoid colon and chemotherapy. With metastasis (which can be asymptomatic), the five-year survival rate does not exceed 30%.
- Intestinal obstruction. A large polyp can partially or completely block the intestinal lumen, which in turn is dangerous due to obstruction and peritonitis. If surgical care is not provided in a timely manner, death occurs.
- Bleeding. Severance of a polyp can lead to massive bleeding, a drop in blood pressure and hemorrhagic shock.
The operation also carries certain risks. Consequences after removal of a polyp in the sigmoid colon:
- perforation of the organ wall and development of peritonitis;
- postoperative bleeding;
- infectious complications (wound inflammation);
- relapse of the polyp after 1-2 years.
Postoperative risks are more justified than possible cancerous degeneration of the polyp, therefore, in most cases, surgical intervention is indicated.
Treatment
There is only one adequate treatment for sigmoid colon polyps - surgical removal. Drug therapy rarely brings positive results; it is usually used simultaneously with surgery and during the postoperative recovery stage.
Drug therapy
Drug therapy can be prescribed if surgery is impossible for various reasons, for small polyps without a tendency to malignant tumor cells. Usually, manipulations with the administration of drugs through a sigmoidoscope are prescribed. The difference between rectosigmoidoscopy and colonoscopy is right here.
Douching, enemas and systemic use of antitumor drugs will not bring the desired effect due to the peculiarities of the location of the sigmoid colon and its distance from the anus.
There are no traditional methods of treatment. Any recipes that prove high therapeutic results are not clinically proven.
Prognosis and prevention
Further prognosis for life depends on an accurate diagnosis:
- A pedunculated hyperplastic polyp in the sigmoid colon rarely recurs; after removal, rehabilitation is quick. The size rarely exceeds 1-2 cm, but doctors recommend removing all formations larger than 0.5 cm.
- Adenomatous polyp of the sigmoid colon, even if small in size, is prone to malignancy into adenocarcinoma, which is difficult to treat and often requires radical intervention. The risk of recurrence of glandular formations is up to 30% per year.
- Hamartomatous, inflammatory polyps do not have oncogenic potential, but can recur. Only observation is required.
It must be remembered that adenomatous polyps are considered a precancerous condition. This is a signal that something in the body is not working correctly and you need to think about your lifestyle. To reduce the risk of new formations it is necessary:
- treat chronic diseases;
- add sports or fitness activities to your weekly schedule;
- review nutrition;
- identify and eliminate sources of constant stress;
- stop drinking alcohol and tobacco.
In adults, the risk of polyps and sigmoid colon cancer is directly proportional to age. The best prevention is screening (endoscopy), especially after 50 years. It is important to undergo periodic medical examinations even in the absence of symptoms.