Thanks to modern medical research (fibroscopy), proliferation of the integumentary pituitary epithelium of the stomach can be detected with great accuracy, because if treatment is started in advance, it has a favorable outcome. Proliferation is the pathological growth of cells. It can be benign or malignant. A biopsy is performed to confirm the diagnosis. There are other modern methods for detecting the disease at any stage. Focal hyperplasia of the gastric mucosa is more common. Although this disease has many varieties.
Origins of the problem
With gastric hyperplasia, cells divide and multiply in increased numbers. Moreover, in the advanced stage of the disease, changes begin in the cells themselves. They turn malignant. What causes cells to multiply so rapidly? There may be several reasons:
- hormonal imbalances in the body;
- advanced chronic inflammation in the digestive organ - gastritis, polyps, ulcers;
- stomach infections that have not been completely cured;
- impaired nervous regulation of the digestive organ;
- regular exposure of the stomach to all kinds of carcinogens (including from smoking and alcohol);
- a hereditary component that promotes the proliferation of epithelial cells.
If you suspect hyperplasia, you should immediately consult a doctor. And if an illness is detected, treatment must begin immediately.
Proliferation of the gastric epithelium against the background of polyps
A gastric polyp is a benign tumor that develops from the pitted epithelium. What is gastric proliferation with a polyp? This is the development of atrophic or hyperplastic changes against the background of an inflammatory process. Cytological biopsies taken from the polyp reveal many accumulations of pitted epithelium. In adenomatous polyps, proliferation of the gastric epithelium is also manifested by the presence of glandular-like cellular structures. If we compare the cell structure of a polyp with a cytogram of gastritis, then young and immature forms with light, large nuclei are more predominant. In addition, in this case, single mitotic figures are often found. With a polyp, lymphoid and glandular elements may be found in small quantities. Proliferation of the gastric epithelium in granulation polyps is characterized by the appearance of abundant inflammatory infiltrates with a high content of neutrophils.
What should you be wary of?
The insidiousness of the disease lies in the fact that hyperplasia is asymptomatic for a long time, so a person does not worry.
As a result, when a chronic advanced form of proliferation of the integumentary epithelium of the stomach has developed, treatment begins with a delay. The thin layer of epithelium that lines the walls of the stomach begins to grow rapidly. How not to be late and seek treatment on time:
- any recurring indigestion, stomach pain, heartburn, belching should be a reason to consult a doctor;
- You should regularly undergo a preventive examination and medical examination, during which a stool test for occult blood is performed;
- If someone in your family suffered from chronic gastritis, peptic ulcer, or hyperplasia of the integumentary pitted epithelium of the stomach, you should also undergo a mandatory preventive examination by a gastroenterologist with appropriate examination.
Here are the signs that begin to worry when epithelial growth is already in force:
- cramping and very noticeable pain in the abdominal area due to involuntary contractions;
- symptoms of anemia may appear;
- it is possible that indigestion may occur during or after a meal;
- Pain in the digestive organ also occurs at night on an empty stomach.
To think that this is ordinary, simple gastritis and that everything will go away on its own is naive. Self-medication is strictly forbidden! You need to go to the doctor immediately.
Your IP address is blocked.
The study of diseases of the gastrointestinal tract, in particular the stomach and duodenum, is the basis of a narrow branch of medicine - gastroenterology. There are many causes of stomach diseases: poor diet, stress, violation of work and rest schedules, exposure to harmful substances, activity of Helicobacter pylori bacteria, etc.
The stomach is an important organ responsible for the general condition of the body; all systems suffer due to gastric conditions. Therefore, it is important to know the causes of stomach diseases and its main diseases. If we consider stomach diseases from the perspective of oncology, the harbingers of this pathology can be gastric ulcers, acute and chronic gastritis, duodenogastric reflux, polyps, and gastric erosion, which are often encountered in the daily practice of gastroenterologists.
During monitoring of inpatient and outpatient patients, this group of gastrointestinal diseases occupies a leading position among disorders that, in combination with various environmental factors, as well as individual characteristics, most often lead to carcinogenic activity.
Any precancerous disease develops in stages with an increase and deepening of negative changes occurring in the stomach. At some stages, any process is completely reversible, that is, the disease is curable. As the destruction deepens, the possibility of reversibility decreases, persistent chronicity of the process occurs, and the disease becomes incurable.
The transition to precancer or cancer is facilitated by the deepest stages, when the disease develops inside cells. Gastritis is one of the most common gastrointestinal diseases of an inflammatory or inflammatory-dystrophic nature that affects the gastric mucosa [4].
Gastritis is classified according to several indicators - by type, localization of the inflammatory process, etiological factor, endoscopic picture, morphological changes in the gastric mucosa.
All these indicators are very important for diagnosing and choosing a method of treating the disease. Atrophic gastritis, a long-term form of chronic disease in which destructive changes occur in the gastric mucosa, deserves special attention.
As a result of the pathological process, its area and the number of functioning cells decrease sharply. Many experts believe [5-7] that this subtype of chronic gastritis is a precancerous condition, and as a result, the threat of developing a malignant process is very high.
With atrophic gastritis, the mechanism of degeneration of normal stomach cells is triggered; the main and accessory cells involved in the production of pepsinogen and hydrochloric acid, the main components of gastric juice, cease to function optimally. Instead, the additional cells of the stomach begin to produce mucopolysaccharides - mucus - in a larger volume. As a result, the acidity of gastric juice sharply decreases.
The fact that cells change their specialization and cease to perform their main function indicates that the body has a malfunction in the system of hormonal, immune, enzyme and other regulators of physiological processes. Gastric ulcer is one of the main causes of morbidity and mortality among more than seven million gastrointestinal pathologies diagnosed annually [8].
Diagnosis of gastric and duodenal ulcers involves the presence of symptoms such as weight loss, oversaturation, epigastric pain, a feeling of fullness, bloating, and nausea. Unfortunately, the presence of these symptoms also fits into the clinical picture of gastroesophageal reflux disease, dyspepsia and gastritis, and therefore diagnosing gastric ulcer is difficult. The asymptomatic course of this pathology often does not allow diagnosis in the early stages of the disease; the disease remains undetected until clinical manifestations, namely bleeding of the gastrointestinal tract [9].
The gastric mucosa is lined by a single layer of epithelial cells, which is supported by thin elements of loose connective tissue covered by a thin layer of smooth muscle fibers. In many people, the gastric epithelium, in addition to its own acidic and enzymatic secretions of the stomach, is exposed to Helicobacter pylori.
The small gram-negative bacilli Helicobacter pylori are uniquely adapted to colonize the human stomach [10]. The presence of these microaerophilic microorganisms leads to the emergence of a number of subclinical and clinical indicators, which depend on the properties of the infecting strain, the host and the environment [11].
A number of patients with gastric ulcers or developing gastric lymphoma who have previously been treated with non-steroidal anti-inflammatory drugs are indicated for eradication therapy. But we cannot ignore the fact that this therapy may worsen gastroesophageal reflux disease and increase the risk of developing esophageal cancer [12]. Gastric polyps are abnormally growing masses of cells that form on the lining of the stomach.
The presence of this pathology is rare, and most often the disease is asymptomatic [13]. Large polyps cause bleeding, anemia, abdominal pain, or rarely cause obstruction due to their location. Only certain types of polyps can have carcinogenic activity and increase the risk of developing cancer in the future, and depending on this, a further treatment strategy is selected, which may include surgical removal of the polyp, monitoring of its changes, and conservative treatment [14].
Assessment of the morphological structure of cells is possible using cytological examination, which is widely used in clinical practice as an extremely sensitive, accurate, effective method for diagnosing malignant tumors and a number of non-tumor lesions of all organs of the digestive tube in patients with symptoms of gastrointestinal diseases, as well as for screening in groups of high risk for developing cancer of these organs [15].
Microscopically, malignant cells line the gastric glands and crypts and are epithelial cells that break through the basement membrane and invade the submucosa and muscle layer.
Individual cells lose their differentiation in relation to neighboring cells and are represented by numerous mitotic figures [16]. To prevent the development of cancer, early detection of such conditions, as well as their high-quality examination, is important.
The introduction and maximum use of modern endoscopic technology has significantly expanded the possibilities of cytological diagnosis of the gastrointestinal tract and, moreover, has opened up prospects for the use of the method, since cytological material is suitable for carrying out immunomorphological, molecular biological and genetic studies of invaluable differential diagnostic value [17, 18].
Conduct a comparative analysis and identify characteristic morphological cytological signs in various pre-tumor diseases of the stomach. The results of endoscopic and cytological diagnostics in patients with pre-tumor diseases of the stomach over the past three years were assessed. The material for the cytological study was tissue taken from the gastric mucosa from patients with gastric and duodenal ulcers and gastric polyps.
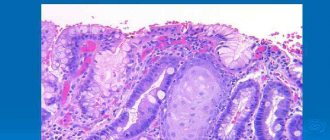
Impressions were made from the collected tissues. To evaluate the preparations, we used the method of light microscopy with Romanovsky-Giemsa staining [19]. The materials were captured using digital technology. All cytological findings were confirmed histologically. Cytological examination of stomach tissues of patients with uncomplicated atrophic gastritis shows no distinctive features. Smears contain cohesive aggregates of glandular epithelial cells and varying amounts of mixed inflammatory elements [20].
Dysplastic patterns include small to large aggregates with somewhat irregular or jagged edges. The constituent glandular cells contain nuclei that are larger than normal, often elongated or cigar-shaped, and include one or more nucleoli. Their chromatin is fine-grained and dark-colored. Nuclear contours range from smooth to slightly irregular. Cytoplasmic mucin is reduced or absent, and nuclear to cytoplasmic ratios increase [21].
Depending on the stage of the ongoing process, there are characteristic features: the presence of wide areas alternating with fields of gray-white recesses of various shapes of the thinned gastric mucosa indicates moderate atrophy.
Severe atrophy is characterized by a dry, thinned mucous membrane, almost no folds, the tissue is vulnerable, the vessels are translucent, have a grayish color with a cyanotic tint. Inside the aggregates, the anomalous cores appear crowded, molded, and overlapped. The tissues of the gastric mucosa are thinned, as a result of which they acquire a light gray color, the folds decrease in size, and the vascular pattern is pronounced.
Thickened convoluted folds with accumulations of mucus between them, swelling and hyperemia of the mucous membrane are signs of hypertrophic gastritis. Based on these features, it is necessary to distinguish gland dysplasia from benign repair. It may be difficult to distinguish between dysplasia and well-differentiated adenocarcinoma.
The only distinguishing characteristic is the presence of individually dispersed and intact abnormal glandular cells. By identifying this feature, adenocarcinoma is diagnosed. With erosive gastritis on the walls of the stomach, erosions are detected in the form of focal inflammation. There may be several such foci, the degree of their development depends on how strongly the disease develops.
The endoscopic picture of hemorrhagic gastritis is polymorphic, as it depends on the morphological basis that caused the bleeding, the time of examination and the degree of anemia of the patient. Erosions up to 0.3 cm in diameter are covered with hemorrhagic plaque, bordered by a rim of hyperemic mucous membrane. Intramucosal hemorrhages are visible as islands [22].
When studying cytological preparations for gastritis, signs of proliferation of the integumentary pitted epithelium were revealed. Certain groups of cells have signs of atypia in the form of a sharp enlargement of the size of cells and nuclei, irregular placement and congestion of nuclei are noted (Fig.
In cases of intestinal metaplasia, tall cylindrical, prismatic or goblet-shaped cells were found in the imprint smears (Fig. Cells of the integumentary pit epithelium with signs of intestinal metaplasia of the small intestinal type. Nuclei of large and medium sizes are observed, their location in the cells is eccentric, and they are intensely colored.
The cytoplasm is characterized by basophilic coloring, almost transparent at the nucleus and apical part, wide in the apical part and narrow, more elongated in the basal part. In the tissues under study there are accumulations of lymphoid elements, as well as plasma cells and segmented neutrophils.
The endoscopic picture of a healing ulcer is characterized by reduced hyperemia of the mucous membrane, the absence of necrotic tissue and purulent masses. The microscopic structure of the mucous membrane depends on the period of development of the ulcer. In cytological smears, desquamated epithelial cells, leukocytes and erythrocytes, fibroblasts, histiocytes, plasma cells and lymphocytes were determined. Directly along the edge of a chronic ulcer, the gastric mucosa undergoes significant thickening due to intensive proliferation of the pit epithelium.
All the cellular elements mentioned above can be found in cytological preparations. In the material obtained from the edges of a chronic ulcer, polymorphic cells of the integumentary epithelium of varying degrees of maturity were usually found. The predominance of immature large cells with large nuclei and basophilic cytoplasm may indicate intense proliferation of the epithelium.
During the period of exacerbation of the ulcer, degeneratively changed epithelial cells without clear boundaries with enlarged nuclei are found in large numbers. The chromatin pattern in them is sparse, in the form of coarse fibers.
In these preparations, segmented leukocytes predominated and elements of granulation tissue were found in significant quantities. During the period of ulcer scarring, very polymorphic cells of the histiocytic type appear in smears, which can be difficult to distinguish from atypical epithelial cells [25].
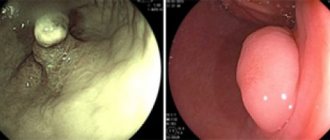
During the endoscopic examination of polyps, the number, shape, size, surface, color, consistency, inflammatory processes and localization of tumors were assessed.
Cytological preparations were characterized by a large number of layers and accumulations of integumentary pitted epithelium. With adenomatous polyps, glandular structures are also found. Compared with cytological descriptions of gastritis, in these diseases there was an advantage of immature cells, the nuclei were light, enlarged, and the chromatin pattern was delicately reticulated. Gland epithelial cells and lymphoid elements are detected in small quantities.
In cases of granulation polyps with abundant inflammatory infiltrates in their stroma, significant numbers of neutrophilic leukocytes can be included in cytological preparations.
The studies revealed changes in the composition and morphology of the cells of the gastric mucosa, which are observed with gastritis, polyposis and ulcers, but are not strictly specific. To establish a diagnosis, it is necessary to use additional research methods, since it is not possible to diagnose these processes based on cytological data alone. Diseases of the stomach and duodenum occupy a major place in gastroenterology. The stomach is an important organ responsible for the general condition of the body, so it is important to know the causes of its diseases and diagnostic methods.
Diseases can be caused by poor nutrition, stress, violation of work and rest schedules, exposure to harmful substances, the activity of Helicobacter pylori bacteria, etc. Timely diagnosis of lesions of the digestive organs helps prevent the development of negative changes in cells, which, under appropriate conditions, can lead to the development of a chronic process, precancerous condition and cancer. A comparative analysis of the endoscopic diagnosis and cytological picture of precancerous diseases of the stomach, such as gastritis, polyp and ulcer, shows that changes in the cells of the integumentary pit epithelium are not strictly specific for each disease: in some observations only slight polymorphism of epithelial cells is noted, in others they clearly predominate immature, young elements with some signs of atypia.
To establish a diagnosis, it is necessary to use other additional research methods, for example, histological, immunomorphological, molecular biological, genetic, since it is not possible to diagnose these processes on the basis of cytological data alone.
In different variations
Gastric hyperplasia has different manifestations. The types of this disease differ in that they affect different parts of the stomach. Thus, we distinguish:
- focal hyperplasia;
- follicular hyperplasia;
- lymphoid hyperplasia;
- hyperplasia of the integumentary pitted epithelium of the stomach;
- glandular hyperplasia;
- polypoid;
- antral;
- foveolar.
The exact causes of the disease have not yet been established. There are only provoking factors. But sometimes hyperplasia occurs when the mucosa is healthy.
Treatment methods for gastric hyperplasia
After the doctor examines the test results and photographs taken during instrumental studies, he determines the direction of combating the pathology.
Small non-glandular formations do not require urgent medical attention. If there is no risk of progression or threat of malignancy, then only constant monitoring by a specialist is required.
Therapy is often also used with:
- antibiotics;
- enveloping drugs;
- proton pump inhibitors;
- substances that reduce stomach acidity;
- gastroprotectors;
- steroidal anti-inflammatory drugs;
- enzymes;
- sedatives.
If conservative treatment is not effective, the doctor decides on surgical intervention. If the disease progresses too rapidly, especially with the rapid growth of the integumentary pitted epithelium, complete removal of the tumors is required.
Starts from the hearth
The focus of hyperplasia in the stomach is a polyp in its early development, which has a benign course and is located in one specific place, the focus. Hence the name.
This disease is determined by the endoscopic method and using special dyes. The lesion is immediately colored. It can be large, small, multiple or single. It is usually formed as a result of erosion of the gastric mucosa.
Erosion of the mucous membrane, as a rule, provokes quite noticeable pain. Therefore, those suffering from this disease may experience cramping pain. They recur periodically, often arising as a reaction to provoking foods.
In addition, another sign of the presence of focal hyperplasia is developing anemia. Its symptoms may appear from time to time. And this is also a reason to contact a gastroenterologist.
In the treatment of focal hyperplasia, medications are used, as well as dietary nutrition that completely excludes fats. Medicines are selected depending on the root cause of the disease. In most cases these are hormonal drugs.
Foveal, lymphoid, glandular hyperplasia
During an endoscopic examination, an asymptomatically developing disease, foveolar hyperplasia of the stomach, can be discovered completely by accident. The foveal form of the disease is the uncontrolled proliferation of cells in the mucous membrane or tissues of the digestive organ. It leads to curvature and thickening of the folds of the mucous membranes of the stomach, lengthening its sections. The disease does not form either a malignant or benign tumor. But it is the initial stage to the development of hyperplastic polyps.
Lymphoid hyperplasia leads to inflammation of the lymph nodes.
Glandular hyperplasia leads to the formation of growths in place of the internal glands.
Polyp-like hyperplasia occurs with the formation of polyps, which can affect not only the digestive organ, but also the intestines.
What is proliferation?
The cells and tissues of the glandular epithelium of the stomach are systematically renewed, so proliferation does not stop. It is necessary to control the level of immunity, eliminate existing tissue defects, regenerate and restore their normal functioning.
On this topic
- Digestive system
Differences between sigmoidoscopy and colonoscopy
- Natalya Gennadievna Butsyk
- December 9, 2021
At the initial stages, cellular growth is regenerative, but over time, with active development, the mucous membrane ceases to recover. The surface of the epithelial glands is covered with nonspecific cells that have an elongated shape and dark color. In the normal state, such structural elements are located only in the glandular necks.
If the process of cell differentiation is disrupted, this leads to the occurrence of extensive atypical growths. The condition is considered very dangerous, as it leads to the development of cancer - carcinoma.
Follicular problem
Follicular hyperplasia of the stomach is also disguised as other diseases in the early stages. But this type of disease is insidious in that it can unnoticeably develop into a malignant form. It should be noted that follicular gastritis is quite rare - one in a hundred. What it is is when white blood cells accumulated at the site of mucosal damage transform into follicles.
The cells grow gradually without causing problems. And only when there are a lot of these cells does the patient experience painful and unpleasant sensations. The following symptoms should alert you:
- seemingly causeless increase in body temperature;
- weakness in the body;
- occasional pain in the digestive organ.
When a person has another disease, for example, gastritis, the patient will feel symptoms characteristic of it. The presence of follicles can only be determined if you go to the clinic about disturbing problems.
Important! If follicular hyperplasia begins to bother you with frequent, severe pain, there is a possibility that the disease has turned into a malignant form.