Laparoscopic surgery for pancreatic diseases
The pancreas is an organ whose disease is most often invisible to a person in the initial stage, so the patient learns about it after an attack of acute pain. Therefore, for timely and effective treatment, it is necessary to immediately contact a specialist for high-quality diagnostics. One of the most effective methods for diagnosing and treating the pancreas is laparoscopy.
Benefits of laparoscopy
Laparoscopy is a relatively new method of performing surgical and diagnostic procedures. With its help, the process of differential examination of the abdominal organs is simplified, especially for complications associated with the pancreas. Laparoscopy simplifies cholangiography using contrast, radiography, biopsy and color photography of internal organs. The method makes it possible to find the cause of the disease, which is especially helpful in emergency cases. Thus, we can highlight the advantages of laparoscopy:
- no scar remains on the anterior wall of the abdomen;
- diagnostic results are more accurate;
- the procedure is painless;
- small blood loss;
- the number of possible complications is much less;
- the postoperative period in the hospital is reduced;
- The rehabilitation period after surgery is shorter.
Such operations extremely rarely require blood transfusions, unlike ordinary ones, when this is almost always a necessity.
You can move your abdominal muscles within 24 hours after surgery; the patient is discharged after about 4 days, since the risk of complications is extremely low.
Contraindications for laparoscopy
Laparoscopy for pancreatitis is not performed in the following cases:
- Insufficient technical equipment, inability to create maximum access to the affected part of the organ and overview of the operated area.
- Adhesive joints in the upper abdomen, omentum.
- Obesity.
- Blood clotting disorder.
- The possibility of cleansing the abdominal cavity in another, less invasive way.
For pancreatic cancer, if there is no access to the affected areas of the organ, laparotomy is considered a more effective method - a conventional operation with an incision in the abdominal cavity.
It should also be noted that, unlike many other types of cancer, it is recommended not to perform a puncture in pancreatic oncology, since due to the peculiarities of its location there is a high risk of bleeding, injury to neighboring organs, and the formation of a fistula. For this reason, surgeons try to create optimal access to the organ and remove tumor formation.
Before deciding to perform laparoscopy, you should make sure that other, less invasive methods cannot solve the problem.
Possible complications after the procedure include:
- Injuries to blood vessels and intestines.
- Hypothermia from dry gases that are injected to bloat the abdomen.
- Burns from electrodes.
- Development of infections.
In laparoscopy, it is very important to find a professional, experienced doctor, since the success of the manipulation depends half on this.
As a therapeutic method, laparoscopy is used for pathologies such as chronic pancreatitis. Using it reveals:
- cyst;
- stone;
- neoplasm (cancer in the initial stage of different localization).
Detection of a tumor or cyst requires oncological vigilance during resection.
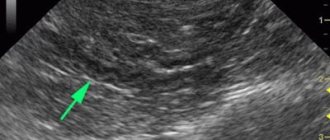
During laparoscopy of acute pancreatitis, it is necessary to remove part of the gland from the retroperitoneal space into the abdominal cavity. Diagnosis is carried out by indirect signs, since the gland itself, due to its topographic location behind the peritoneum, is not accessible to direct examination.
Laparoscopy can only be refused if the patient has:
- obesity;
- pathology of the blood coagulation system;
- manifestations of mental disorders.
The above is taken into account during planned laparoscopy. In urgent cases, the procedure should be performed in all necessary situations, with the exception of:
- clinical death;
- agony;
- conscious refusal of the patient to undergo manipulation.
Indications
Laparoscopy as a surgical method is prescribed for:
- formation of pancreatic necrosis in the presence of acute pancreatitis;
- the need to examine deformities of the pancreas due to pancreatitis;
- the presence of cysts and various types of neoplasms as a consequence of chronic pancreatitis.
Laparoscopy as a research method is used for:
- jaundice, which progresses when you need to find out its origin;
- hepatomegaly, the genesis of which is unknown;
- ascites, the origin of which cannot be diagnosed in any other way (liver cirrhosis or cancer cells are often found in parallel);
- exclude the presence of cancer cells in the gallbladder;
- definition of urinary tract diseases.
Laparoscopic diagnosis allows you to check at what stage pancreatitis is and its severity.
Pancreatic resection for malignant tumors
Cystadenomas (benign tumors of the pancreas) are amenable to such resection most often; the procedure is effective for a neuroendocrine tumor located in the same organ. Malignant tumors must not be removed in this way. However, if you follow the rules for working with cancer cells, laparoscopic resection can be considered one of the safest and most reliable methods.
The big disadvantage of such a resection is that there are few people who have undergone the procedure, so the method is considered experimental and requires confirmation and further study.
Laparoscopy often reveals malignant tumors that were considered harmless tumors before the procedure. If such a situation occurs, the following facts are taken into account:
- what concomitant diseases does the patient have?
- are there tumor cells in the resection margin;
- is it possible to carry out effective treatment;
- Is it necessary to do another resection, but according to the rules of oncological procedures?
If a patient needs such a resection of the pancreas for pancreatitis, it is necessary to prepare for it, namely:
- conduct an external visual inspection;
- conduct laboratory biochemical diagnostics to determine whether there is a possibility that the tumor is hormonally active;
- do a CT scan with slices of 0.3-0.4 cm;
- perform endoscopic ultrasound and biopsy if there is a suspicion that the neoplasm is malignant;
- sometimes it is necessary to do retrograde cholangiopancreatography.
Biochemical analysis is carried out selectively. Diagnostic parameters are determined depending on the symptoms. If biochemical data are equivocal, a challenge test or site-specific studies may be performed.
Laparoscopic distal pancreatectomy
The indications for the procedure are the same as for any other operation. But distal pancreatectomy is not used to treat malignant neoplasms. This method is suitable for removing pseudocysts and tumors in the gland or its tail. The use of this method is prohibited for:
- malignant pancreatic tumors;
- physicians who are not skilled in open surgery or the complex procedures that use such methodology.
In what cases is it prescribed?
Laparoscopy of the pancreas is performed for:
- Necrosis of pancreatic tissue, accompanied by the development of infections and abscess.
- Enzymatic peritonitis.
- Multiple organ failure, which has developed and persists for three days after conservative therapy, as this is a clear symptom of the death of gland tissue and the retroperitoneal zone.
- CT or MRI revealed 50 percent death of gland tissue.
- Spread of necrosis to the retroperitoneal region.
- Cyst formation.
- Overgrowth of the gland with scar tissue to restore the outflow of digestive enzymes during long-term chronic pancreatitis.
- The formation of stones that block the bile, pancreatic duct and duodenal lumen.
- Tumor formations.
- Periampullary cancer.
- Ascites of the head of the pancreas.
Before deciding on the choice of laparoscopy as a method of treatment or surgical intervention, it is necessary to evaluate the possibility and effectiveness of its implementation in a particular case, and make sure that there are no contraindications.
In order to find out that laparoscopy is possible and not dangerous in a particular case, the patient must undergo some studies. Appointed:
- Clinical, biochemical blood test, blood clotting test.
- Toxicological analysis of urine and blood.
- Ultrasound of the abdominal and retroperitoneal space.
- In special cases - CT scan and tests for tumor markers.
- It is necessary to undergo fluorography, cardiogram, and be tested for HIV and hepatitis.
If the operation is urgent, blood, urine, and coagulation tests are performed, and the blood type and rhesus are determined. If the decision is positive, laparoscopic surgery is prescribed.
Direct preparation for surgery involves fasting for eight hours before the procedure. If the operation is scheduled for the morning, it is not recommended to eat after 18.00 in the evening of the previous day, so that the body has time to digest all the food. The absence of food in the esophagus reduces the risk of developing an abdominal infection and vomiting during the administration of anesthesia.
On the day of the procedure, an hour before the procedure, the patient, if necessary, is also given a cleansing enema or given medications to cleanse the intestines.
Before the procedure, the patient must remove jewelry, lenses, and dentures.
Immediately before the operation, the patient is given drugs that make it easier to enter anesthesia, prevent the development of fear, reduce the secretion of glands and the risk of allergic reactions. Anesthesia is usually administered intravenously and through the respiratory tract.
Progress of the operation
The operation is carried out according to the following algorithm:
- Injection of carbon dioxide into the abdominal area to create free space, which will ensure visualization of the operated area and free movement of instruments. The gas is collected using a needle that is inserted through a hole created in the navel.
- Hollow tubes are inserted through small incisions in the abdomen to provide a path for surgical instruments used during the operation. As a rule, three tubes are inserted: one for the laparoscope (it is inserted into the previously made umbilical incision), the other two are for introducing additional instruments.
- A laparoscope is inserted, on which a light guide and a video camera are attached.
- The abdominal cavity is examined for the presence of existing lesions, the degree of their growth, the presence of adhesions and inflammatory foci.
- The planned therapeutic actions (decompression, drainage, debridement) or removal of tissue, tumors, adhesions or stones are carried out.
- Material is collected for histological and biological examination.
- Purulent contents (if any) are removed.
- The abdominal cavity is examined to ensure that all emergency procedures have been completed.
- Surgical instruments are removed.
- Gas is removed.
- The incisions made (usually there are only three) are closed with sutures.
If the sutures are cosmetic, they will dissolve on their own; if they are ordinary, they are removed 10 days after the procedure.
Rehabilitation
| Factor | Recommendations |
| Diet | On the first day after surgery, it is recommended to refrain from eating and drink only a small amount of still alkaline water. The next day, depending on the patient’s condition and the severity of the operation, artificial nutrition with special mixtures can be used or a transition to gentle nutrition can be made according to the fifth dietary table. |
| Caring for seams | After removing the threads for two weeks, it is recommended to treat the seams with brilliant green/iodine to prevent infection, and periodically change the dressings. As a rule, you can swim on the third day after the stitches are removed. A month after the operation, for better healing of scars in the absence of signs of inflammation, they can be treated with special ointments. |
| Loads | Two to three weeks after surgery suggest limiting physical activity. |
| Sex life | If the dynamics of recovery are positive, sexual activity can begin two weeks after the operation. |
Following these points is very important for a speedy recovery and prevention of postoperative complications.
Loading…
The indications for the procedure are the same as for any other operation. But distal pancreatectomy is not used to treat malignant neoplasms. This method is suitable for removing pseudocysts and tumors in the gland or its tail. The use of this method is prohibited for:
- malignant pancreatic tumors;
- physicians who are not skilled in open surgery or the complex procedures that use such methodology.
Today, 3 options for the procedure have been developed:
- the spleen is removed at the same time;
- do not violate the integrity of the spleen and its vessels;
- crossing the vessels, but without touching the spleen.
They try to preserve the spleen because it plays an important role in the fight against capsular pathogenic microorganisms. This has a beneficial effect on the functioning of the body and life expectancy. This information has not been fully confirmed, so many surgeons remove the organ, especially since it is difficult to preserve the vessels during laparoscopy.
Preparation:
- give anesthesia;
- endotracheal intubation is performed;
- a Foley catheter is placed;
- the patient's position depends on the location of the tumor;
- compression stockings are put on the legs;
- making the abdominal cavity sterile.
Procedure:
- the abdominal cavity is examined using a video laparoscope;
- thanks to dissection they get to the pancreas;
- Laparoscopic ultrasound is used to accurately detect tumors and large vessels in the pancreas;
- looking for a relatively thin place in the gland;
- vessels are mobilized with a stapler, except for those that fit tightly;
- a part of the organ is resected and taken from the abdomen;
- place a drainage tube;
- drainage is removed.
This method protects the abdominal cavity from infections from the outside. The likelihood of developing hernias and pain syndrome is reduced to zero. After the operation, the patient must strictly adhere to the prescribed diet for a year. After this time, the patient completely recovers. Then he must undergo a control ultrasound every six months.
Other operations on the pancreas
Pancreas surgery is performed using different methods. Registration in a high-quality online casino Frankcasino. Link to the Frank Casino website https://www.casinozru.com/casino/frank-casino.html Remember about the tournaments. See reviews from gambling addicts or get free bonuses and play on your mobile phone at Frank Casino. First, the surgeon makes small incisions in the abdomen and inserts a laparoscope. This way he can examine the organs and determine whether the tumor has metastasized. The type of surgical intervention depends on where the tumor is located: in the head - Whipple surgery, in the tail - distal pancreatectomy, in the body - total pancreatectomy:
- During a Whipple operation, the doctor removes the head of the organ, part of the stomach, small intestine and bile duct; their integrity will be restored over time.
- Using laparoscopy, diagnostics are carried out, during which they look for the location of cancer metastases. This is the last research method that gives final results about the extent of tumor spread. Thanks to the fact that today's laparoscopes have improved optical fibers, biopsy devices and other instruments, the capabilities of laparoscopy have increased. This diagnostic method helps to more accurately determine the tactics of future treatment of the pancreas for pancreatitis.
- Surgery for pseudocyst. Method used: transgastric access. The pancreas is accessed through the stomach using an endoscope and laparoscope. Drainage is carried out.
- Laparoscopic enucleation. Used for benign neoplasms. The method requires minimal resection. Applies to superficial tumors up to 20 mm. In order to determine how much fabric needs to be cut, a special sensor is used. The anterior fascia is opened and the tumor is removed.
- Pancreaticoduodenectomy. The method is experimental and its benefits have not been proven.
source
Methods of laparoscopy for pancreatitis: indications and technology
Laparoscopy for pancreatitis has been used to a limited extent, but is currently used for many surgical pathologies, including diseases of the digestive system.
The term itself means the essence of this method: “laparo” is translated from ancient Greek as belly, “scopy” is an examination that is performed using a special apparatus with an eyepiece - a laparoscope. It is inserted into the abdominal cavity through a small (1.0-1.5 cm) incision in its anterior muscle wall. In addition to the laparoscope itself, a manipulator is inserted through a similar second hole - an instrument with which the surgeon performs some operations.
How the procedure is performed
The patient takes a position on the operating table depending on the type of intervention. For example, pancreatic resection requires the patient to lie on his right side.
Laparoscopy is an operation on the pancreas, which is performed using a special surgical instrument, a cannula. It is inserted into the abdominal cavity through a small incision in the abdomen just below the navel. Then:
- The peritoneal space is filled with carbon dioxide.
- Additional incisions are made on the anterior abdominal wall to use additional instruments and a video camera.
- The progress of the operation is monitored on the screen.
After removing the tumor and completing the excision of the dead areas, the incision is sutured. The instruments are first removed and drainage is installed to ensure the outflow of fluid from the organ and prevent tissue swelling.
If the purpose of the operation was diagnosis, after receiving the results of the biopsy, a decision is made on further treatment tactics. Laparoscopy for pancreatitis lasts on average up to three hours.
What is pancreatic laparoscopy?
Laparoscopy is a minimally invasive surgical diagnostic and treatment procedure. This is an informative way of primary diagnosis of complex pathologies that have not been accurately diagnosed by other, more accessible methods. In certain situations it is used as a minimally invasive therapeutic procedure.
The method is characterized by low trauma and high selectivity.
Laparoscopy of the pancreas: subtleties of surgery for pancreatitis
Laparoscopy of the pancreas is a minimally invasive diagnostic and treatment procedure. Until recently, it had very limited use, but today doctors prescribe this procedure for many surgical diseases of the insulin-producing structure.
The essence of laparoscopic surgical technique is working through small punctures using manipulators
Refusal of traditional laparotomy in favor of laparoscopic techniques has reduced the number of postoperative complications and shortened the recovery period.
Benefits of diagnostic and therapeutic laparoscopy
Since all surgical operations on the abdominal organs are extremely traumatic, risky and entail many negative consequences, laparoscopy has significantly facilitated this process. It has significant advantages over classical laparotomy, when access to the abdominal cavity is made through a midline incision of the anterior abdominal wall from the epigastrium to the symphysis:
- high accuracy of visualization of all spaces and organs;
- more accurate diagnosis;
- reduction of trauma to the abdominal wall (incision length is usually 25–30 cm, in some cases longer);
- reducing trauma to the abdominal organs - when making a cut for a better view, the organs are displaced and thereby disrupt their anatomical location and injure them;
- significant reduction in rehabilitation time and shorter hospital stay;
- no scar after the procedure.
Advantages and disadvantages of the technique
The advantages of laparoscopy are as follows:
- Painless procedure;
- More accurate diagnosis;
- Shorter rehabilitation period for the patient after the operation;
- No scars on the anterior abdominal wall.
Due to the fact that during laparoscopy small incisions are made, the devices themselves are small in diameter and are equipped with lenses that allow obtaining high-quality images, it has many advantages over conventional surgery, which involves a large incision in the abdominal cavity.
These advantages include:
- less trauma to the abdominal wall and internal organs;
- better visualization of the operated area;
- short period of hospital stay;
- rehabilitation is faster and less painful;
- after the procedure, small, neat scars remain, which heal much faster than traces of large incisions;
- less trauma reduces the risk of developing postoperative complications.
At the same time, this method also has some disadvantages:
- due to the use of optics, the perception of the depth of insertion of the laparoscope is distorted - professionalism is needed to calculate the required depth and correctly insert the device;
- the device is not as flexible and resourceful as the doctor’s hands, such clumsiness reduces the range of the procedure;
- it is difficult to calculate the force of pressure of instruments on tissue, since there is no tactile sensation, this again requires experience and professionalism;
- it is not possible to calculate some organ characteristics (for example, tumor density);
- during the procedure, the doctor sees only the specific operated area and cannot examine the abdominal area as a whole (for this reason, the presence of tumor formations in the space that is located outside the visualized area can be missed).
Laparoscopy is a relatively new method of performing surgical and diagnostic procedures. With its help, the process of differential examination of the abdominal organs is simplified, especially for complications associated with the pancreas. Laparoscopy simplifies cholangiography using contrast, radiography, biopsy and color photography of internal organs.
- no scar remains on the anterior wall of the abdomen;
- diagnostic results are more accurate;
- the procedure is painless;
- small blood loss;
- the number of possible complications is much less;
- the postoperative period in the hospital is reduced;
- The rehabilitation period after surgery is shorter.
Such operations extremely rarely require blood transfusions, unlike ordinary ones, when this is almost always a necessity.
Since all surgical operations on the abdominal organs are extremely traumatic, risky and entail many negative consequences, laparoscopy has significantly facilitated this process. It has significant advantages over classical laparotomy, when access to the abdominal cavity is made through a midline incision of the anterior abdominal wall from the epigastrium to the symphysis:
- high accuracy of visualization of all spaces and organs;
- more accurate diagnosis;
- reduction of trauma to the abdominal wall (incision length is usually 25–30 cm, in some cases longer);
- reducing trauma to the abdominal organs - when making a cut for a better view, the organs are displaced and thereby disrupt their anatomical location and injure them;
- significant reduction in rehabilitation time and shorter hospital stay;
- no scar after the procedure.
Indications and contraindications for surgery
As a therapeutic method, laparoscopy is used for pathologies such as chronic pancreatitis. Using it reveals:
- cyst;
- stone;
- neoplasm (cancer in the initial stage of different localization).
Carrying out laparoscopy for pancreatic necrosis comes down to identifying and excision of dying organ tissue.
Detection of a tumor or cyst requires oncological vigilance during resection.
During laparoscopy of acute pancreatitis, it is necessary to remove part of the gland from the retroperitoneal space into the abdominal cavity. Diagnosis is carried out by indirect signs, since the gland itself, due to its topographic location behind the peritoneum, is not accessible to direct examination.
Indications and contraindications
Minimally invasive intervention on pancreatic tissue is indicated for the following diseases:
- benign tumors;
- malignant tumors in the initial stages of formation;
- cysts in chronic forms of pancreatitis;
- pancreatic necrosis.
Laparoscopy for pancreatic necrosis is performed to remove areas that have died. Tumors and cysts are resected in compliance with the principles of oncological radicality. Acute forms of pancreatitis sometimes require removal of part of the gland into the abdominal cavity. This prevents contact of healthy tissue with the inflamed organ and pancreatic juice, which can lead to destruction of a section of the peritoneum, intestines or large blood vessel.
For diagnostic purposes, surgery is prescribed if the patient is diagnosed with ascites of unknown etiology, jaundice, or enlarged liver. In this case, through the camera of the laparoscope, the surgeon performs a visual examination of the abdominal organs and, if necessary, separates tissue microparticles for cytological examination.
Laparoscopy is refused if the patient suffers from obesity, pathology of the blood coagulation system, or mental disorders. However, these contraindications are relevant only for planned interventions. Emergency laparoscopy can be performed in almost all cases. The exception is clinical death, agonal state, conscious refusal of an adequate patient from medical care.
Laparoscopy for diagnostic purposes
Diagnostic laparoscopy is performed infrequently: for example, if an ultrasound scan fails to detect an area of necrosis or tumor.
Indications for the use of laparoscopy for diagnostic purposes:
- jaundice as a sign of hepatitis or obstruction of the common bile duct by a tumor or stone - it must be differentiated as an acute sign or accompanying inflammation of a chronic nature (calculous cholecystitis);
- peritonitis to clarify the etiology;
- determination of the scale and nature of damage to the pancreas (pancreas);
- establishing the form of confirmed pancreatic necrosis.
Diagnostic methods for prescribing laparoscopy
Diagnostic laparoscopy is performed infrequently: for example, if an ultrasound scan fails to detect an area of necrosis or tumor.
Indications for the use of laparoscopy for diagnostic purposes:
- jaundice as a sign of hepatitis or obstruction of the common bile duct by a tumor or stone - it must be differentiated as an acute sign or accompanying inflammation of a chronic nature (calculous cholecystitis);
- peritonitis to clarify the etiology;
- determination of the scale and nature of damage to the pancreas (pancreas);
- establishing the form of confirmed pancreatic necrosis.
Before prescribing therapeutic laparoscopy, it is necessary to carry out a number of examinations, despite the fact that the method itself is not considered dangerous, and no complications are observed after it. Mandatory diagnostic methods for deciding whether to prescribe laparoscopy include:
- clinical and biochemical blood tests;
- coagulogram - a comprehensive analysis of blood clotting indicators;
- toxicological analysis of blood and urine (if poisoning with alcohol, toxic substances, drugs is suspected);
- Ultrasound of the abdominal organs and retroperitoneal space;
- CT;
- if necessary, tests for tumor markers.
All preliminary studies are needed to assess possible risks:
- bleeding;
- perforation of neighboring organs.
Before laparoscopic surgery, the following types of laboratory and instrumental research methods are required:
- General blood analysis;
- Blood biochemistry;
- CT scan;
- Magnetic resonance imaging;
- Angiography;
- Biopsy.
Having received the results, the attending physician makes a decision on the advisability of laparoscopy. They will draw up a detailed plan for the procedure and what needs to be done immediately before the operation:
- Visual diagnostics, which is necessary to accurately determine the anatomical structure of the pancreas.
- Biochemical blood test to determine whether the tumor is dependent on hormones.
- Computed tomography of the organ, designed to select the optimal location for access to the pancreas during surgery.
- Ultrasound diagnostics combined with biopsy.
- Taking tests for tumor markers.
After performing a certain set of these diagnostic procedures, the doctor makes a decision on the need to perform laparoscopic surgery and draws up a plan for further preparing the patient for the procedure.
Diagnostic laparoscopy is performed in rare cases. For example, if it is impossible to determine the location of the tumor process or the area of necrosis using ultrasound.
Laparoscopy as a treatment method
With the help of therapeutic laparoscopy you can:
- remove purulent contents from the abdominal cavity in case of peritonitis of pancreatogenic etiology;
- open and clean the zones of destruction around the pancreas and in the tissues of the organ itself.
Indications for therapeutic laparoscopy:
- acute pancreatitis;
- pancreatic necrosis, subject to infection with the development of an abscess;
- peritonitis developed under the influence of enzymes (abacterial);
- the presence of multiple organ failure after intensive conservative therapy for 3 days (this indicates extensive necrosis of pancreatic tissue and retroperitoneal tissue);
- more than 50% of pancreatic tissue necrosis detected during examination on CT angiography;
- spread of pancreatic necrosis into the retroperitoneal space, diagnosed by other methods, which can lead to death.
But according to the published results of recent studies, it is believed that:
- in acute pancreatitis (AP) and pancreatic necrosis (PN), laparoscopy is contraindicated - this is due to the peculiarities of its implementation and complications aggravating the course of AP and PN;
- PN can be diagnosed using modern non-invasive methods: ultrasound of the abdominal organs and the retroperitoneal space;
- the result of therapeutic laparoscopy (LL) is not higher than the effect obtained from radiation or surgical treatment;
- the possibility of sanitation of the abdominal cavity with peritonitis or retroperitoneal phlegmon is successfully solved without LL.
Preoperative preparation for the operation
The day before the procedure, dinner is not recommended; a cleansing enema is performed in the morning.
The procedure is painless because anesthesia is performed before it is performed. Preliminary drug preparation is carried out before anesthesia by injection of a narcotic analgesic. The patient is taken to the operating room on a gurney.
After tracheal intubation, endotracheal anesthesia is administered. To prevent thrombophlebitis, intermittent compression sensors are attached to the legs. The skin of the abdomen is treated with alcohol and iodine, after covering the area around the intended intervention with sterile linen.
How is the operation performed?
The essence of laparoscopy is surgical intervention using manipulators through small punctures.
The technique of the procedure is simple: to insert a probe and other instruments, 3–4 small incisions (0.5–1.0 cm) are made in the anterior abdominal wall. To create a working space, a pneumoperitarium is created - the abdomen is filled with carbon dioxide. The following are the necessary steps:
- removal of necrotic areas of the pancreas;
- abdominization.
Then the laparoscope and auxiliary devices are removed, sutures are applied to the incision sites, and they are covered with an aseptic dressing.
To prevent postoperative infection, the patient is given the maximum dose of antibiotic in the operating room.
If during laparoscopic intervention it turns out that it is impossible to eliminate the pathology using this method without interrupting the operation, an open laparotomy is performed.
Progress of the operation
Despite the absence of a wide incision, laparotomy is a rather painful intervention. Therefore, before it begins, the patient is put under anesthesia. An endotracheal option is used to suppress the activity of the central nervous system, which requires intubation of the patient. The anesthetic-air mixture is supplied directly into the respiratory tract through the endotracheal tube.
After the patient has fallen asleep, the surgeon makes several (3-4) incisions 0.5-1.5 cm long, through which instruments are inserted into the abdominal cavity. To provide working space, the patient is given pneumoperitoneum (the abdomen is inflated with carbon dioxide). Next, the manipulator is carried to the affected area and the necessary actions are performed (abdominization of the pancreas, resection).
After completion of the work, the laparoscope and auxiliary units are removed, sutures are placed on the incisions, after which the damaged skin is covered with an aseptic bandage. To prevent infectious complications, a loading dose of an antibiotic can be administered to the patient directly in the operating room.
On a note! Sometimes during the intervention it turns out that it is impossible to eliminate the pathology laparoscopically. In such cases, without interrupting the operation, proceed to open laparotomy.
More about abdomization
Abdominalization of the pancreas is an operation aimed at removing the organ into the abdominal cavity. Normally, the gland is located in the retroperitoneal space, separated from the stomach, intestines and liver by the parietal layer of the peritoneum.
The operation is performed for severe forms of acute pancreatitis. The fact is that as a result of massive necrosis of the pancreas, decay products and aggressive enzymes easily enter the retroperitoneal tissue and intestinal mesentery - diffuse peritonitis develops, and the patient’s condition worsens significantly. The risk of death increases.
The intervention is performed by incising the abdomen along the midline. First, the doctor injects an anesthetic into the tissue surrounding the gland, and then dissects the peritoneum. The organ is bloodlessly removed into the abdominal cavity, wrapped in an omentum, after which drainage is installed between them to drain the “ichor” and administer antibiotics.
Abdominization is carried out only in cases where there is a high probability of restoration of the gland and allows to significantly limit the inflammatory process.