Classification of polyps
During the research process, an extensive classification of rectal polyps was created. First of all, it is worth noting that all benign tumors of the rectum are divided into two main types: epithelial, which are the most dangerous and common, and rare neoplasms, the prevalence of which does not exceed 3.5%.
Rectal polyps are divided according to the following criteria: multiplicity, size, geological structure. Multiplicity criteria distinguish such groups of polyps as single, diffuse multiple (group and scattered). Based on their histological structure, it is possible to distinguish such types of polyps as glandular, hyperplastic, villous and glandular-villous. As for the size of polyps, their malignancy directly depends on it.
Glandular polyps are most prone to malignant degeneration. That is why, if a patient is found to have this type of polyp, he is diagnosed with a precancerous condition. Quite often, villous polyps that have a round or elongated shape and a velvety pink-red surface develop into cancer. It is worth noting that most polyps go through several successive stages of development: small neoplasms increase in size over time, after which they can even degenerate into malignant tumors.
One of the most dangerous types of polyposis is diffuse, which is also called familial. It is characterized by the growth of a large number of polyps in the rectum and other organs. Statistical data from scientists confirm that the risk of malignant degeneration of diffuse polyps reaches 80-100%. That is why it is extremely important to diagnose this type of polyps as early as possible in order to prevent their growth and transformation into malignant cancer.
Polyp removal
Initially, medicine had only one option for conservative therapy to combat such benign lesions. We are talking about celandine juice. But as soon as researchers realized that this approach had no practical benefit, they stopped using it altogether.
Today, treatment involves exclusively surgical removal, as well as a fairly long postoperative period. It is aimed at healing and preventing the recurrence of the growth. In private medical centers and public hospitals, the following methods are used to implement the plan:
- polyectomy, which relies on the use of a proctoscope and colonoscope;
- transanal excision;
- resection of a certain piece of intestine;
- transanal resection, which involves the formation of an anorectal anastomosis;
- endomicrosurgery.
The first version is the most popular. The operation itself involves first inserting an operating device into the rectum, and then a loop is thrown over the appendage through it. Later, the loop is heated by connecting to an electric current, which allows the polyp to come out without problems.
Rehabilitation and the manipulation itself last much longer for those who have become victims of polyposis. It all depends not only on the diameter and specific location of the growths. The results of histological testing will have to be taken into account.
If visualization showed that the polyps are scattered individually, but do not exceed 0.5 cm in size, then you will simply have to undergo regular examinations at least once every six months. But as soon as the benign formation becomes more than 0.5 cm, you can move on to an active strategy. It covers polypoethmoidotomy under the control of endoscopic equipment.
This step is explained by the risk of malignancy, which means transformation into a malignant tumor. To neutralize “nests”, the same methods described above are used, with an eye to the affected area.
If the doctor preferred sigmoidoscopy with subsequent removal of the lesion, then the former site of polyp growth must be cauterized. This will protect the intestines from infection by pathogenic microorganisms.
Very rarely, doctors use the tactic of direct incision of the intestine, when endoscopic equipment acts as an assistant. The collected pathological material is then sent to a clinical laboratory.
Etiology and pathogenesis of polyps
The exact causes of benign tumors have not yet been established. This is difficult to do, since the formation of polyps often occurs asymptomatically. In addition, polyps are found mainly in those patients who complain of symptoms such as discomfort, pain and discharge in the anus, and intestinal dysfunction. Making a diagnosis is complicated by the fact that these symptoms are similar to the manifestations of diseases such as colitis, hemorrhoids, rectal cancer, paraproctitis.
Research into the incidence of rectal polyps is still ongoing by scientists. Today, the increase in the incidence of pathology among the population is associated with factors such as environmental problems and a decrease in physical activity. In addition, great importance in the formation of polyps is given to the process of changing nutrition. Namely, the diet of the population of most economically developed countries is dominated by high-calorie foods, which contain a large percentage of animal fats. Such a diet is dangerous because chyme, which contains too little fiber, enters the rectum, which ultimately leads to a decrease in intestinal motility. Also, a large volume of bile acids regularly enter the intestines, which then, during the digestion process, turn into dangerous substances that can have a carcinogenic effect on the mucous membrane. Some studies pay much attention to the gender principle of the formation of intestinal polyps. Namely, they are most often diagnosed in men.
Types and Types of Anal Polyps
Clinicians distinguish two main classifications of polypous formations: according to the nature of their occurrence and structural features (histology results).
By type of occurrence
The following groups of polypous neoplasms are distinguished according to the nature of their occurrence::
- Inflammatory or infectious - the polyp is based on past inflammation;
- Neoplastic - with excessive growth of intestinal mucous tissue;
- Hyperplastic - type 3 polyp is the result of the proliferation of abnormal mucosal epithelial cells.
It is important ! The most difficult prognostically are neoplastic and hyperplastic growths of the mucous membrane, since the process of their occurrence can be influenced by many hereditary or autoimmune factors.
According to morphological structure
Thanks to the possibility of performing a biopsy, doctors can evaluate not only the structural features of the polyposis lesion, but also compare the risks of possible malignancy of the tumor. There are several types of tumors.
Fibrous
Fibrous polyps are formed from connective tissue and epithelial cells. Another name for them is false. Fibrous polyps are the least likely to develop into cancer. This is their main difference from other types of pathological proliferation of mucous membranes.
The main cause of fibrous growths is chronic inflammation of the tissues of the rectum and complications of diseases in this localization:
- haemorrhoids,
- fistulas,
- cryptite,
- paraproctitis.
These polyps are shaped like a mushroom or a pear and usually have a thick stalk or a wide base. Malignancy is possible only in the case of constant trauma or cases of rectal cancer in close relatives.
Adenomatous
The adenomatous polyp is based on a variety of tissues, mainly glandular epithelium. This feature is responsible for the second name of adenomatous polyp - glandular growth or adenoma. Along with glandular cells, the body of the polyp may also contain atypical components.
Adenomatous growths are often multiple and are formed due to uncontrolled cell division and proliferation. Fast-growing colonies of small tumors spread throughout the entire length of the rectum, which leads to discomfort and unpleasant symptoms.
Attention ! Adenomatous or glandular polyps are most prone to malignancy. The incidence of malignancy reaches 65% of all clinical cases. Treatment is usually long-term and has a long rehabilitation period.
Hyperplastic growth
Hyperplastic growths of the mucous membranes are a type of polyposis with rapid spread of growths along the lining of the rectal canal. There is no specific reason for its occurrence.
Pathology often becomes a secondary complication:
- dysbacteriosis,
- duodenitis,
- peptic ulcer and gastritis,
- infectious lesions of the gastrointestinal tract.
The base of the polyp is always edematous and hyperemic. The body of the polyp contains plasma cells, a lymphocytic component, erosions, and cystic cavities.
If for the stomach hyperplastic growths of the mucous membrane are organotypic, then in the case of the rectum, they are at least atypical. The formation of hyperplastic polyps is based on a violation of cell functionality, slowing down or stopping the processes of secretion and production of secretions.
Hyperplastic polyps are formed even in young children due to spontaneous intrauterine mutations.
The structure of the polyp is complex and has the following features:
- wide base;
- whitish shade of the base;
- size less than 5-6 cm;
- spherical shape of the polyp body;
- smooth glossy surface.
Note ! Hyperplastic polyps have a minimal risk of malignancy, just like fibrous neoplasms. Risks of malignancy occur in only 2% of all clinical cases.
Villous polyp
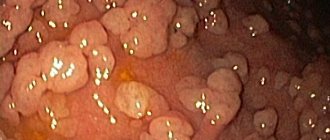
Villous neoplasms are round in shape, have a velvety surface, and a wide base. Villous ones are the most dangerous in terms of malignant degeneration of cells. There are known cases of malignancy of only one polyp villi less than 1 mm.
At the early stage there are two main development paths:
- Along the intestinal mucosa;
- Inside the lumen of the organ.
The nature and features of growth may vary depending on:
- progressive course of pathology,
- prescribed therapy,
- taking medications.
The volume of the neoplasm varies and can reach 10 cm.
Among the symptoms, especially:
- Copious anal discharge (wetting underwear);
- Painful and frequent urge to defecate;
- Atypical discharge in stool (mucus, blood, pus);
- Feeling of pressure in the rectum.
Fibrous polyps are the least likely to develop into cancer.
Pain and other unpleasant symptoms completely depend on the sensitivity of the patient, his age, and anamnestic features. If the polyps are located close to the anus, they may fall out of it or be pinched by the sphincters.
Symptoms of rectal polyps
In almost all cases, the formation of benign formations of the colon and rectum occurs without symptoms. However, if the polyp reaches a size of 2-3 centimeters, the patient may experience the following symptoms of rectal polyps:
- Bleeding from the rectum. Rectal bleeding is the main symptom of many proctological pathologies, in particular anal fissure, rectal cancer, hemorrhoids, and ulcerative colitis. Of course, immediately after the appearance of such bleeding, you should contact a proctologist to find out their causes.
- Constipation. Constipation is caused by intestinal obstruction caused by polyps. An increase in the size of polyps leads to impaired intestinal motility.
- Abdominal pain. This symptom is the least common and occurs in the case of an inflammatory process in polyps.
Symptoms
The symptoms of rectal polyposis are not specific, which makes its diagnosis very difficult. There may be no symptoms for a long time, especially when the growth is single and small in size. Manifestations of symptoms begin when large affected areas or large-diameter neoplasms are observed. It is not uncommon for a patient to accidentally discover a polyp during a routine examination or during examination for another pathology.
Common symptoms of a polyp in the rectum:
- aching systematic pain in the lower abdomen, in women is often mistaken for hormonal changes and gynecological pathologies;
- constant constipation and chronic diarrhea, alternation is possible, but constipation is more common as a consequence of intestinal obstruction;
- increased gas formation along with constipation;
- hemorrhoids and anal fissures;
- bleeding from the anus is the most common reason for patients to visit a doctor; copious mucus may be released;
- itching, burning in the anus, sensation of a foreign body;
- discomfort during the act of defecation, a feeling of incompleteness of the process after visiting the toilet;
- the presence of blood and mucus in the stool;
- elevated body temperature as an indicator of the inflammatory process in the body.
In children, diagnosis is difficult, since all the signs described above do not directly indicate the pathology of polyposis and appear to be a consequence of many diseases. The most dangerous symptom is heavy rectal bleeding, which can lead the patient to anemia.
Diagnosis of rectal polyps
Quite often, cancer occurs against the background of inflammation of polyps. However, it is worth noting that polyps grow slowly. That is why it is extremely important to diagnose their formation at an early stage. Of course, detecting a polyp at an early stage can increase the favorable prognosis of its treatment by 90%. The most effective diagnostic methods for detecting polyps include the following:
- Digital rectal examination. Using this technique, you can examine a large area of the rectum and identify neoplasms. This method is also used to diagnose rectal fistulas, hemorrhoids, and anal fissures.
- Sigmoidoscopy. One of the most effective methods of examining the rectum, which allows you to accurately and in detail assess the condition of the patient’s rectal walls. Since most polyps are often located in the sigmoid and rectum, using a proctoscope it will be quite easy to identify them.
- Irrigoscopy. This technique involves the introduction of a barium suspension into the rectum. After administering the drug, an x-ray is taken, which will reveal polyps larger than one centimeter in size.
- Colonoscopy. To carry out this diagnostic procedure, the patient should undergo a course of enemas. The technique allows you to very accurately identify even small polyps - less than one centimeter in size.
- Biopsy. This is one of the most important methods that allows you to accurately determine whether there is cancer in a given case. The technique is based on taking a suspicious area for histological examination. A biopsy can be performed during a colonoscopy or sigmoidoscopy.
- Fecal occult blood test. This technique involves examining stool for the presence of blood. However, it is worth remembering that in some cases polyps may not bleed, so this analysis may be ineffective.
- CT scan. Helps detect rectal polyps even of very small size.
Clinical picture
Depending on the structure of the epithelial formation, the clinical picture of polyposis can vary greatly. Let's look at the existing options one by one.
It is better to go to the hospital immediately
The first option involves the formation of a so-called adenoma - a benign tumor of the glandular epithelium. Most often, it is during the formation of this type that blood is released into the stool.
In appearance and structure, adenomas are thick, pink in color, the same as the intestinal mucosa.
It is this form that most often becomes a malignant formation. The size of the polyp-adenoma is approximately 2-3 centimeters. The connection to the intestine is made through a stalk:
- thin;
- or fat.
The second type of formations that grow during polyposis is villous in nature. It is also formed from epithelium, like other species. Often it is the villous polyp that causes rectal bleeding, since its body is penetrated by vascular branches. In addition, it is the formations that have a villous appearance that are most prone to the development of necrotic processes, which result in the formation of ulcerative tissue.
The size of the villous formation is usually impressive, the lower limit of the size is around three centimeters; as a rule, they grow much larger, causing constant constipation in the patient.
Polyps vary in structure and appearance
The third type of polyp is called hyperplastic. The diameter of such formations can reach a maximum value of 5 millimeters. The growth of such formations is most often not accompanied by any symptoms, in addition, they themselves also rarely cause serious harm. After all, their soft structure and short stature not only do not interfere with the natural process of bowel movements, but also do not affect the additional formation of any secretion, the opening of bleeding and do not cause many other negative consequences.
The fourth type appears to be a mixture of two structures:
- glandular;
- villous.
Their structure is combined, due to which it is quite rare (according to statistics, only 20% of patients are “awarded” with a mixed structure of polyposis). Symptoms during the germination of the formation of the desired form are very scant; blood spots in the stool are also almost impossible to detect, unless, perhaps, only with the help of studies conducted in the laboratory.
Video - About the most important things. Polyps in the intestines
Differential diagnosis
Polyps in the rectum can be easily confused with other pelvic pathologies. That is why it is also necessary to carry out differential diagnosis in order to make a more accurate diagnosis. Namely, it will be necessary to distinguish polyps from the following diseases:
- Crohn's disease, in which the inflammatory process is located in the upper part of the large intestine;
- actinomycosis, most often located in the cecum;
- non-epithelial tumors, which include fibroids (tumors of the muscle layer) and angiomas (vascular tumors);
- lipoma, which is predominantly localized in the submucosal layer of the colon.
Dangerous consequences of polyposis
What is the danger of having polyps inside the rectum? These neoplasms pose a very tangible threat to human health and future life. Many people do not understand this, since the formations are considered initially benign. However, despite this fact, they cause a number of extremely negative consequences.
First of all, we are talking about the degeneration of a polyp into a cancerous tumor. In this case, the most dangerous growths will be classified as adenomas. This type of polyp is diagnosed most often. Their villous form, crowned with many finger-like processes, is especially susceptible to malignancy.
The more extensive an adenoma grows, the more likely it is that it will become a cancerous tumor. As for the attachment relative to the intestinal walls, if it stands on a thick stalk, this is also a bad sign.
Removal of a polyp by burning the pedicle with a diathermic loop
When a polyp forms, intestinal obstruction may develop. In other words, there will simply be no room left for the stool to pass through, hence stagnation will occur. Feces will remain in the intestines, as a result, toxins will be absorbed into its walls and released into the body. This will not only lead to poisoning, allergies and dehydration, but also in especially advanced cases will justify the development of necrotic processes (death of the intestines). As a result, feces will enter the peritoneum, peritonitis will develop and the patient will die.
Enterocolitis, which takes on an acute form, can also form against the background of irritation by polyps of the intestinal wall. As a result of its occurrence, the rectum and other parts of the intestines will be covered with ulcers. Symptomatically this will manifest itself as follows:
- the person will feel severe pain in the peritoneum;
- his body temperature will rise;
- Blood may be found in the stool.
If surgical intervention is not performed in time under such circumstances, the person will die due to:
- perforation of the intestinal walls;
- infection spreading through the blood.
Infectious processes inside the rectum, caused by the growth of a polyp, can penetrate from it directly to the fatty layers of the body, forming pouches filled with pus. This causes not only very sensitive pain, but also an increase in body temperature. As a result, the disease becomes chronic. A person loses the ability to work, constant fatigue and lethargy appear.
The formation of polyps can lead to problems associated with bowel movements , such as:
- diarrhea;
- constipation
Despite the fact that the disorders seem to be completely different, with polyposis they alternate with each other, causing serious discomfort. With adenomas, it is diarrhea that most often opens, since the polyp is isolated a lot:
- salt;
- water.
As a result, such an essential chemical element as potassium is washed out, and its deficiency in the body develops, which provokes a disruption in the functioning of organs that constantly need this element.
When the stool is particularly fluid, a person loses the ability to control the flow of stool and also retain gases.
Polyps cause pain inside the intestines
The results of constipation and stagnation caused by polyposis can be fecal stones formed in the intestines. Fecal masses harden and turn to stone, forming compactions, which ultimately disrupt the work associated with the digestion of food entering the body. In addition, often oncological processes often begin to develop in places where fecal stones come into contact with the intestines.
Under the influence of polyps, the walls of the rectum can crack. This happens because when stool is released, the polyps block the passage, and the intestines have to stretch. The walls crack and there is acute pain that cannot be ignored. Because of this, a person tries to restrain acts of defecation, which in turn leads to the formation of constipation and fecal stones.
The constant loss of blood, which polyps provoke in one way or another, is another very unpleasant threat to human health. Anemia causes weakness in a person, and loss of strength is constantly felt.
Treatment of rectal polyps
Conservative treatment of rectal polyps does not give a positive result, so only surgery is chosen for this purpose. Namely, rectal polyps are often removed using an endoscope or surgical methods. If the polyps are located too low, they are removed transanally. If you are interested in how a small rectal polyp is removed, please note that this is done primarily during an endoscopic procedure using electrical excision. To do this, the stalk of the polyp is captured with a loop electrode and then clamped. If it is necessary to remove large polyps, they are first divided into parts.
The doctor should take into account that surgical intervention can often be complicated by perforation of the intestinal wall and even bleeding. Sometimes cancer cells are discovered during a diagnostic test. In this case, a decision is usually made to resect the entire cancer-affected area of the intestine. If diffuse polyposis is detected in a patient, then total resection of the large intestine is used to eliminate it. Upon completion of the operation, it is necessary to connect the end of the ileum to the anus.
Treatment of polyps in children and adults
Treatment for polyps in the rectum is possible without surgery at an early stage, but you need to start as soon as possible. Medicines are rarely prescribed, only for multiple polyps that cover the gastrointestinal mucosa or to reduce their size.
The main treatment option is surgery. Although, if there are significant contraindications in older people, doctors often resort to wait-and-see tactics and only in case of complications take urgent measures to perform surgery.
With polyposis in children, the main goal is to eliminate the pathological neoplasm and prevent the development of repeated rectal bleeding, which interferes with the normal development and growth of the child’s body.
Even multiple small rectal polyps in a child (unlike adults) are not subject to malignancy, so the disease develops slowly and is successfully treated.
For polyps in the rectum, the doctor selects treatment tactics taking into account the degree of spread of the pathological process and the location of the tumor. For children, transanal removal of polyps or Farabeuf hooks is applicable when the polyps are located up to 6 cm from the posterior opening.
Other modern techniques also have quite effective results:
- polypectomy followed by electrocoagulation of the polyp stalk;
- bowel resection.
Single, scattered polyps on a short stalk are successfully removed by polypectomy with the introduction of a special colonoscope instrument. For polyps with a wide base, intestinal resection is performed, removing the affected area and performing an anastomosis.
To obtain the best results, doctors often combine techniques. Relapses in the postoperative period in children are extremely rare.
Prognosis for rectal polyps
With timely detection and removal of polyps, a complete recovery of the patient is quite likely. However, in some cases it is not possible to prevent a recurrence of the disease. Such relapses often occur several years after the removal of polyps. To prevent the return of the pathological process, a colonoscopy is performed a year after the operation. In addition, it is advisable for the patient to undergo endoscopic examination every couple of years. It is worth noting that the size and number of tumors play a large role in the development of cancer. Therefore, large multiple polyps are most susceptible to malignancy. The most dangerous type of rectal polyps is considered diffuse, which most often degenerates into cancer.
Causes of polyps growing inside the intestines
According to ongoing medical research, the reasons that influence the appearance of epithelial sprouts in the intestines combine many different factors.
As a result of a scientific examination of the problem, it was found that polyps cannot form inside a healthy intestinal mucosa, since the existing environment in it is not friendly for them. Therefore, if you find that polyps have sprouted inside your intestines, know that pathological processes in the organ began some time before their occurrence. In other words, despite the fact that polyposis is a separate disease, it itself is a symptom of some other pathology of the intestinal lining.
Benign polyposis can turn into cancer
There is also a list of so-called risk factors that contribute to the formation of polyposis. Let's look at it below.
An aggravating factor that adds to the likelihood of polyposis is heredity. According to studies, there is a certain genetic predisposition that causes the occurrence of polyposis in blood relatives. If at least one person in your family suffered from the germination of polyps in the intestines, his descendants are already at risk. Most likely, these neoplasms will also be detected in them.
In addition, not only descendants, but also other relatives are at risk. This is due to the fact that the sick family member most likely also inherited a predisposition to polyposis from some ancestor. This means that the disease can also manifest itself in:
- brothers and sisters;
- nephews;
- other relatives.
According to studies, blood relatives with a predisposition to polyposis suffer from this pathology approximately 10 times more often than the general population.
In addition, during the antenatal period of human development (when he is in the womb), when the formation of the rectum occurs, a predisposition to the disease is already embedded in the person. After birth and as an adult, under the influence of many factors, a person is more likely to develop disorders that determine the set of genes in him.
Polyposis is often inherited from parents
The second factor that influences the formation of almost any pathology of the intestines and gastrointestinal tract, as well as many other organs, is also inherent in polyposis. These are nutrition-related disorders that lead to poor bowel function and persistent constipation. We are talking primarily about:
- an unbalanced diet in which animal fats predominate;
- lack of a meal schedule;
- the presence of a large amount of food waste on the menu.
It is very important that intestinal peristalsis works perfectly so that polyps cannot grow on its mucous membranes. To do this, you need to follow some rules when creating a diet. Let's see in the table below which products are harmful and which will only be beneficial.
Table 1. Effect on intestinal motility
| Positive | Negative |
Foods rich in fiber have a positive effect on peristalsis and intestinal function in general, for example:
| Food waste, as well as foods that are difficult for the body to digest, containing large quantities of harmful fats and other substances that negatively affect health, have a negative impact on peristalsis and the functioning of the gastrointestinal tract:
|
Nutrition culture is a very serious issue from the point of view of today's medicine, since “you are what we eat.” In other words, a properly formulated diet sometimes turns out to be more effective and healthier than vitamins and medications. Sometimes normalizing the diet can stop the development of a disease in its infancy, which in itself says a lot.
Of course, the table contains far from complete lists of products that can have a positive or negative effect. We have presented only those of them that, despite their obvious usefulness, are almost absent in the diet of an ordinary Russian or resident of another country, or, despite the obvious harm, are, on the contrary, present in abundance.
The lack of fiber in the menu has an extremely negative effect on the process of polyp formation, since it is this substance that helps feces form and leave the body smoothly. But processed and refined foods slow it down very much; baked goods made from wheat flour, sugar, smoked and salty foods are especially harmful. The inclusion of this food waste in the menu creates a favorable environment for the development of polyps inside the intestines, as well as the appearance of other pathologies of the gastrointestinal tract.
The third factor that puts a person at risk is diseases of any part of the intestine that are chronic. Most often preceded by polyposis:
- colitis;
- ulcerative colitis;
- proctosigmoiditis.
In addition to chronic diseases, the growth of polyps is also provoked by acute intestinal infections. Most often, the colon is affected first, creating a favorable environment for the formation of polyps.
The following infectious diseases are especially dangerous (and beneficial for polyps):
- rotavirus infection;
- dysentery;
- salmonellosis and the like.
Even if it is possible to cure the pathological process quite quickly, after it the mucous membrane is still weakened for some time, and polyps can germinate. They arise as a result of a lack of oxygen inside the intestinal epithelium.
The lifestyle of a potential patient, usually accompanied by a low degree of mobility due to office work, for example, can also influence the formation of polyposis. In addition, if physical inactivity is combined with the unsatisfactory ecology of the region where a person lives, the likelihood of their occurrence becomes even higher.
The fact is that low mobility implies slow movement of blood inside the small pelvis, the so-called stagnation, which provokes disturbances in the outflow of lymph and venous blood, which ultimately leads to swelling and constipation.
Polyps can be detected using many different methods.
Prevention of rectal polyps
Unfortunately, there is currently no specific prevention of polyps. However, several preventive measures can be identified that can reduce the likelihood of tumors occurring in the rectum. These primarily include an active lifestyle, a healthy and balanced diet, timely diagnosis and treatment of diseases of the digestive tract. Of course, the earlier the pathology is diagnosed, the lower the likelihood of rectal cancer.
Let's sum it up
When a polyp appears inside the rectum, the prognosis for a complete recovery without consequences is very favorable. Relapses occur after some time in 30% of patients, however, their occurrence can be influenced by maintaining proper nutrition and leading a healthy lifestyle.
Polyposis is not a death sentence; in the early stages, the prognosis for its treatment is completely favorable
The time after which the polyp re-grows is approximately one year. It is after 12 months that patients who have undergone surgery come for a repeat colonoscopy. If the results are favorable, then the next time for examination should be in 36 months.
Listen carefully to your own feelings and do not delay in seeing a doctor if you find signs of polyposis. Remember, you have the power to prevent the development of the disease and its attendant consequences.