Reactive changes in the pancreas develop as a result of diseases associated with the stomach, intestines, liver and other parts of the digestive system. The sign indicates changes in most physiological manifestations in the body, therefore, when it appears, you need to immediately contact a doctor and undergo a full examination.
reactive changes in the pancreas
Causes
What are reactive changes in the pancreas? Reactive changes in an organ are not considered a separate pathology and cannot go away without permission. These disorders are a reaction of the organ to various types of diseases associated with the organs of the stomach and intestines, as well as to adverse effects experienced by the body.
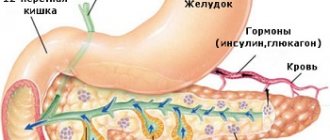
The pancreas is the second largest in the abdominal area after the liver, and ensures the production of 2 important phenomena.
- Production of insulin required for glucose absorption.
- The production of digestive juice, without it there will be no normal digestion.
The juice enters the duodenum through the ducts. The position of these ducts is important for the functioning of the pancreas. Since all organs of the gastric and intestinal tract are transmitted through ductal channels, various diseases of any of them immediately affect the activity of the organ, leading to reactive disorders.
Enzymes produced by the organ begin to be active only when they enter the intestinal area. If the juice from the duodenum is thrown into the pancreatic canals, these elements begin to function early, as a result of which the gland tissues are absorbed. This leads to the formation of reactive changes in the pancreatic parenchyma, which leads to the formation of provoking causes.
The reasons for the development of reactive manifestations are considered:
- infectious diseases - reactive changes occur against the background of pneumonia, viral infections, colds;
- the presence of inflammation in the stomach and intestines - the organ enlarges due to gastritis, ulcers, damage to the esophagus;
- peritoneal injury;
- liver and gallbladder diseases;
- irrational eating - inflammation appears as a result of drinking alcohol, soda, consuming fast foods;
- taking medications – the formation of reactive manifestations is observed if long-term treatment with antibiotics, drugs that eliminate inflammation and fungus, and diuretics;
- birth defects;
- problems after vaccination;
- poisoning of the body;
- presence of chronic diseases;
- complications after abdominal surgery;
- patient's age. According to statistics, women aged 40-50 years experience pancreatic diseases more often than men.
taking medications for reactive symptoms
What are reactive changes?
In response to exposure to irritants of various origins, responses begin to occur in the pancreas with the destruction of cellular structures.
Secondary changes in the pancreas most often occur against the background of cholelithiasis. Violation of the outflow of juice and bile leads to the reverse reflux of active enzymes, and self-digestion of the organ occurs.
Mechanical, toxic and chemical effects lead to an imbalance in the intra- and extracellular environment, the release of biologically active substances occurs, and severe inflammation develops. All these processes are reversible and will have a favorable outcome if measures are immediately taken to eliminate the root cause.
Symptoms of reactive changes in the pancreas
Both in an adult and in a child, the development of pathology can occur in a chronic manner, the symptoms of which may not appear for a long period of time. However, if diffuse changes in the pancreas of a reactive nature are at the stage of exacerbation, then the pathology is accompanied by a painful manifestation in the abdomen.
In the acute form, nausea, vomiting, pain, swelling, which are accompanied by allergies, may occur.
The intensity of the development of signs of the disease depends on how severely the pancreas is affected.
When the initial stage of reactive lesions is observed, the following symptoms appear:
- unbearable pain in the ribs, abdominal area, flatulence, which intensifies after eating and vomiting;
- increased formation of gases;
- nausea;
- esophagitis;
- diarrhea;
- atavism;
- vomiting with the release of bile and mucus.
increased gas production
Features of the signs of the pancreas in children:
- A painful phenomenon in the abdomen, stomach. They subside when the child sits down, slightly tilting the body forward.
- Vomiting with undigested pieces of food. After the vomiting process it doesn’t get any easier.
- An increase in body temperature may occur.
- Frequent diarrhea. The stool is watery in texture and has a foul, pungent aroma. With long-standing reactive changes, the stool is unstable, diarrhea is replaced by constipation.
- Dryness of the oral mucosa, there is a milky coating during the examination.
- Appetite is impaired. Eating irregularly and in small quantities, refusing foods that you previously liked.
- Constant belching, increased gas formation, bloating.
- Decreased tone, increased fatigue.
It is often difficult to diagnose reactive disorders, since the symptoms are similar to other diseases - colitis, gastric and duodenal ulcers, hepatitis. Therefore, it is important to immediately consult a doctor if such manifestations occur.
Clinical signs
Changes in the pancreas of a reactive nature arise as a consequence of pathologies of the gastrointestinal tract or liver. What exactly provoked the pathology determines what signs will appear first. In the event that a violation of the integrity of the parenchyma is associated with diseases of the biliary tract and liver, the changes will be diffuse in nature. In this case, the first alarming symptoms will be expressed in acute painful sensations localized in the upper abdomen, nausea and constant diarrhea.
If reactive changes in the pancreas are associated with gastrointestinal diseases, most often a duodenal ulcer, then in addition to nausea and pain in the epigastric region, a person will constantly be accompanied by bloating, flatulence and sour belching. But all these symptoms are also characteristic of other pathologies of the gastrointestinal tract, so only an experienced specialist can make a correct diagnosis after conducting special diagnostic studies.
In the same case, if a sick person ignores the first alarming symptoms, does not consult a doctor in a timely manner and does not begin treatment, the disease will progress very quickly. This will be expressed in the following symptoms:
- painful sensations in the stomach area become very intense and take on a long-term character;
- pain reduction is possible only when the patient takes a sitting position with a slight tilt of the torso forward or lies on his side, pressing his knees to his stomach;
- vomiting becomes profuse and constant, and the expelled masses of food mixed with gastric juice do not bring any relief to the patient;
- stool instability appears, that is, previously present diarrhea begins to alternate with constipation;
- low-grade fever (37–38 °C) constantly persists;
- the oral mucosa is dry, and the tongue is covered with a yellowish or white dense coating;
- gas formation in the abdominal cavity increases, which is expressed in bloating, belching and flatulence;
- a person with reactive changes in the pancreas almost completely loses his appetite.
But these pathological manifestations are not always present. In some cases, reactive pathological changes occurring in the gland can occur with very minimal symptoms or without them at all. In these cases, the pathology becomes an incidental finding during diagnostic studies carried out to identify another disease.
Diagnostics
Recognition of pathologies of the esophagus and gland is complex, which includes the determination of dysfunctions of the organ and its structure. By examining all organs, this will allow us to identify the main cause of the reactive changes in the organ.
Diagnosis of reactive disorders is carried out using ultrasound; it involves examining all organs of the gastric and intestinal tract that could have an impact on the formation of pathology. A healthy organ has no affected areas or changes in size. Diffuse damage that spreads evenly throughout the tissues of the organ is also absent.
- In the presence of uniform damage to the parenchyma and an overestimated size of the gland, an acute course of reactive disorders is characteristic.
- If a chronic form of reactive pancreatitis develops, a decrease in the echogenicity and density of pancreatic tissue occurs, and the size of the pancreas remains unchanged.
- A smooth increase in echogenicity with normal organ sizes indicates lipomatosis, when tissue fragments are replaced by adipose tissue.
- If there is no change in the size of the organ, or if it decreases, the parenchyma thickens, and the density and echogenicity also increase, then this indicates a fibrotic condition.
Ultrasound of the pancreas
In addition to ultrasound, the following methods are included in the diagnosis of reactive disorders:
- A general blood test helps to detect an increased ESR and leukocyte volume in case of inflammatory phenomena;
- A urine test is performed to determine the content of enzymes that are excreted unchanged by the kidneys;
- to refute or the presence of inflammation in the organ, a urine test is prescribed;
- a biochemical blood test helps to identify enzyme levels;
- endoscopy of the duodenum to study the position of the mucosa in the area of the duct inflow;
- The coprogram is used to identify the amount of undigested protein and fat particles in the stool.
After carrying out all the procedures, the gastroenterologist carefully studies the results of diagnosing pancreatic changes and prescribes therapy for the underlying disease that provoked the reactive state of the pancreas. By eliminating the main factor, it will be possible to stabilize the organ.
Reactive pancreatitis
When the first signs of reactive pancreatitis appear, a series of clinical and biochemical tests are performed: a general blood and urine test, a coagulogram, the level of pancreatic enzymes in the blood and urine, blood elastase, total protein and calcium. There is usually an increase in amylase and trypsin inhibitor levels in the blood and urine with normal levels of lipase and trypsin. It is possible to increase the level of blood elastase in the first few days of the disease.
The development of reactive pancreatitis is indicated by an exacerbation of chronic pathology of the digestive tract in the anamnesis, and the presence of other etiological factors in the patient. During the physical examination, attention is drawn to tachycardia, arterial hypotension, pallor of the skin and mucous membranes. Palpation of the abdomen is painful in the upper parts, a positive Mayo-Robson sign is determined (pain in the left costovertebral angle). The abdomen is usually distended but soft, and symptoms of peritoneal irritation are negative.
Ultrasound of the abdominal organs, especially targeted examination of the pancreas and biliary tract, is the safest and most informative method for diagnosing reactive pancreatitis. This method allows you to identify stones in the common bile duct, swelling and enlargement of the pancreas. To clarify the diagnosis and more detailed visualization of the pathological focus, it may be necessary to conduct a survey radiography of the abdominal organs, computed tomography (the gold standard for diagnosing pancreatitis) and MSCT of the abdominal organs. Endoscopic RP and choledochoscopy for reactive pancreatitis should be carried out only according to strict indications (proven obstruction of the common bile duct with a stone); Magnetic resonance imaging of the pancreas and biliary tract can successfully replace these studies, which will allow us to visualize stones, determine their size and location.
Angiography of the celiac trunk in reactive pancreatitis indicates increased vascularization of pancreatic tissue. Esophagogastroduodenoscopy in the acute period of reactive pancreatitis is indicated for all patients, as it allows not only to diagnose concomitant pathology, but also, if necessary, to carry out endoscopic restoration of the patency of the duodenal papilla. Laparoscopy is required only in cases of severe reactive pancreatitis and diagnostic difficulties.
Treatment
Detected reactive disorders in tissues require complex treatment. When treatment of the main disease is started in time, the iron returns to its normal position, therefore there is no need to prescribe excessive medication so as not to overload the digestive system.
If the case is serious, the victim is treated in a clinic, where he is constantly monitored by a doctor. During therapy it is required to adhere to bed rest and dietary nutrition.
The main therapeutic measures for a reactive pancreas include:
- abstinence from alcohol;
- following the dietary table;
- avoiding physical activity until complete remission occurs.
dietary food
Treatment with medications is prescribed taking into account the main disease that caused the reactive disorders. It is possible to use symptomatic therapy if abnormalities are detected in the analysis, the presence of complaints and signs that indicate changes in the functioning of the pancreas.
Often, in these situations medications are prescribed:
- Painkillers – in mild cases, non-steroidal drugs that relieve inflammation will help, but in severe cases, narcotic analgesics are indicated.
- Antispasmodics – Platyfillin, No-spa.
- Drugs that eliminate bloating - Espumisan.
- Enzyme medications – Mezim, Pancreatin.
Diet cannot be excluded in the complex treatment of disorders. If you do not follow this rule, then all treatment will be in vain. Therefore, nutrition for pancreatitis goes like this:
- refusal of foods that can provoke irritation of the pancreas - these are smoked meats, pickles, spicy and fatty dishes;
- cooking food exclusively by steaming, frying is prohibited;
- limit carbohydrate intake, this will reduce the burden of activity;
- fractional diet 5-6 per day;
- To facilitate the digestion of food, foods should be chewed well and consumed only warm.
The permitted products include:
- stale bread;
- soups with vegetables;
- cooked meat;
- fermented milk products;
- vegetables;
- fruits.
vegetable soup
It is necessary to follow these recommendations during the period of remission, since the pancreas immediately responds to changes in the diet, resulting in aggravation of pancreatitis.
Treatment of reactive changes in the gland
The treatment regimen for pathology strictly depends on the severity and cause of its occurrence. To normalize the condition, you will need to adhere to the following principles:
- follow a diet;
- be regularly monitored in hospital;
- take medication.
Treatment differs for adults and children. It is necessary to take into account the characteristics of the body. It is necessary to assess the person's condition. Sometimes it is necessary to be hospitalized in a hospital.
If the cause of the modification of the gland is chronic pancreatitis, then the doctor will create a diet and prescribe food enzymes to relieve the load on the pancreas. If a provoking disease of any other organ is identified, drug therapy will be formulated.
Note! Treatment may include taking antibiotics, antivirals, and restorative drugs.