The pancreatic ducts are a system of powerful collectors, which are formed by the ducts of the original system, flowing into the main excretory canal. At the same time, they are formed from channels with a smaller diameter. Due to them, enzymes of pancreatic juice are promoted, which is secreted with the help of secretory cells of the acini into the passage of the small intestine, where the organ channel opens. The enzymes formed in the pancreatic gland pass into the duodenum through the main outlet in the area of the duodenal papilla of Vater due to the sphincter of Oddi.
Anatomy
This is an oblong organ, about 20 cm long. It occupies part of the retroperitoneal space, the lumbar spine is located behind, and the stomach is in front. Structural parts:
- Head. Close contact with the horseshoe-shaped depression formed by the bends of the duodenum allows the pancreatic ducts to open into this section of the intestine and provide the digestion process with the necessary enzymes.
- Body. It has three sides and resembles a prism. At the border with the head there is a notch for the mesenteric vessels.
- Tail. Directed to the spleen.
The duct of Wirsung runs along the axis of the organ. The organ is located in a connective tissue capsule. The anterior surface of the gland is covered with peritoneum.
Pancreatic ducts: how many channels in the pancreas and what pathologies they have
The pancreatic ducts perform an important function in the digestion process: they connect the organ with the intestines, due to which the process of food digestion proceeds physiologically.
There are not many duct pathologies, but they all cause serious discomfort. Let's look at how these ducts are structured and what symptoms indicate their damage.
The structure of the pancreatic ducts
Ducts are necessary for this organ so that pancreatic secretions can enter the lumen of the duodenum and begin to actively participate in the digestion process.
The hepatic ducts passing through the pancreas join to form the common bile duct. The pancreatic duct unites with the bile duct: they flow together into the duodenum. This happens most often, but there are other structural options:
- In half of all cases this variant is detected. The pancreatic duct and common bile duct unite before entering the duodenum to form an ampulla.
- The formations are connected to each other, but a common ampoule is not formed between them. In percentage terms, this type occupies 33%.
- The common bile duct and the pancreatic duct enter the intestine separately from each other: they do not unite with each other; the duodenum has two papillae (major and small).
- The common bile duct and pancreatic duct connect with each other long before they flow into the duodenum. This option accounts for 8% of cases.
Some people have an accessory pancreatic duct. Its presence is not a pathology. Therefore, the question of how many channels there are in a person’s pancreas can only be answered after additional examination.
What is the duct of Wirsung?
The main pancreatic duct of the pancreas is called the Wirsung duct. It lies in the thickness of the organ, running from the very tail to the head. It is obtained as a result of the fusion of smaller, lobular ducts. The Wirsung duct follows all the anatomical curves of the organ, this is especially important in the area of the head of the gland.
It can be clearly visualized using ultrasound. The normal length is from 16 to 23 cm, the diameter of the lumen varies depending on the location. In the tail it will be smaller, and in the head area there is an expansion of the Wirsung pancreatic duct: it increases 3-4 times.
The shape can be arched, S-shaped or knee-shaped.
At the end there is the sphincter of Oddi: the pancreatic duct itself opens into the duodenum, where the secretion then enters.
Main pathologies
The condition of the pancreatic and bile ducts is affected by any disease of the gastrointestinal tract. Pathology can be:
- congenital - most often these are developmental anomalies, characterized by a violation of the structure, shape, aplasia, etc.;
- acquired – problems arise throughout life.
The main pathologies that are found in the pancreatic ducts are stenosis, dilatation of the pancreatic duct, obstruction and obstruction, as well as inflammation.
Blockage of the lumen can be caused by various pancreatic cysts, tumor formations, scars, adhesions, pancreatitis and many other diseases.
Causes and symptoms
Ducts are affected in humans for various reasons. Among them are predisposing factors:
- poor nutrition;
- advanced infections of the digestive system, endocrine disorders;
- excessive alcohol consumption;
- severe and prolonged stress;
- autoimmune infections;
- metabolic disorders (diabetes mellitus).
Clinical manifestations of diseases can be extremely varied. The problem may not manifest itself in any way, but sometimes there is a sharp deterioration in the condition. Symptoms may also increase gradually as the disease progresses. Signs of disturbance in the ducts may be as follows:
- Discomfort in the right hypochondrium, which can last from several hours to a week or even a month.
- Pain of a girdling nature, involving the upper abdomen.
- Change in skin color: the skin and mucous membranes begin to turn yellow due to a violation of the outflow of bile.
- Change in stool color: it becomes light due to stercobilin deficiency.
- Itching of the skin - most often appears with jaundice.
- Darkening of urine due to impaired bilirubin metabolism.
- General signs of the inflammatory process: increased fatigue, weakness, fever.
All these symptoms indicate that there are problems in the digestive system that under no circumstances should be neglected. This can lead to serious consequences and complications.
Diagnostics
A gastroenterologist deals with pathologies of the pancreas and its ducts. It is this specialist who should be contacted for pain in the upper abdomen, stool disturbances and other characteristic symptoms listed above.
The doctor conducts an examination, after which, to clarify the diagnosis, he necessarily prescribes additional examinations:
- general blood test to detect signs of inflammation;
- Analysis of urine;
- coprogram;
- biochemical blood test (the level of bilirubin, alkaline phosphatase, enzymes: amylase, lipase, the amount of transaminases is especially important);
- ultrasound examination (is the main diagnostic method, in which not only the pancreatic duct is visualized, but also nearby structures);
- MRI and CT (show an accurate picture of the condition of the abdominal organs and surrounding tissues, you can see if the pancreatic duct is dilated, evaluate its course and tortuosity);
- biopsy under ultrasound control of suspicious areas of the gland.
On an ultrasound or MRI, along with the pancreas, you also need to look at the liver, gallbladder and its ducts, stomach and duodenum. This is necessary for differential diagnosis. For example, with mild inflammation, the pancreatic duct will not be differentiated during examination.
Treatment
Treatment of the pathology depends on its severity and the general condition of the body. In the acute phase of the inflammatory process, NSAIDs are prescribed, in more severe cases - antibacterial agents, and detoxification therapy is carried out in the hospital.
As a rule, doctors try to treat diseases using conservative methods; if necessary, they limit themselves to minimally invasive techniques.
Types of duct interventions:
- Choledocholithotomy is a surgical operation in which the common bile duct is partially excised. This is carried out with the aim of ridding the patient of gallstone disease.
- Installation of a stent in the duct: a metal structure is placed in its lumen, which eliminates the narrowing of the duct and its obstruction.
- Drainage of the bile ducts. A catheter is inserted into the lumen, the entire procedure is carried out under endoscopic control.
Source: https://zhkt.life/podzheludochnaya/zabolevaniya/anatomiya-protokov-podzheludochnoy-zhelezy-i-ih-patologii/
Function of external (exocrine) secretion
The parenchyma of the organ forms pancreatic juice, which has an alkaline reaction in order to neutralize the acidic food bolus. The volume of juice per day is up to 2 liters. The basis of the juice is water, bicarbonates, potassium and sodium ions and enzymes.
Some enzymes are inactive because they are very aggressive. These enzymes include:
- trypsin, its inactive form is trypsinogen, which is activated by intestinal enterokinase;
- chymotrypsin, which is formed from chymotrypsinogen by activation with trypsin.
They are proteolytic enzymes, that is, they break down protein together with carboxypeptidase.
- amylase - breaks down carbohydrates (starch), also available in the oral cavity;
- lipase breaks down fats that are partially broken down into small droplets by bile;
- ribonuclease and deoxyribonuclease act on RNA and DNA.
Functions of the pancreas and gallbladder in the body
The functions performed by the pancreas and gastrointestinal tract are aimed at maximizing the digestion of incoming food. The role of these organs in the digestive process is different, but their general activity involves the breakdown of food components and providing the body with necessary substances and energy.
The pancreas, due to its structure, is intended for the synthesis of pancreatic juice, which contains 20 enzymes, combined into 3 groups:
- lipase - breaks down fats,
- protease - proteins,
- amylase - carbohydrates.
These enzymes are produced in an inactive form. Their structure changes under the influence of the duodenal enzyme, enterokinase. It is released when a bolus of food enters the stomach and becomes active, in turn, in the presence of bile, converting trypsinogen (protease) into trypsin. With its participation, other pancreatic enzymes are activated, which enter the intestinal lumen when food enters there.
Bile is a catalyst for pancreatic and duodenal enzymes. The qualitative composition and quantity of enzymes released depend on the food consumed.
The pancreas produces 1.5−2 liters of pancreatic juice per day. Through the small ducts of the acini (islands consisting of glandular cells that have their own ducts and vessels), the secretion enters the larger excretory canals, through which it flows into the main - Wirsung - duct. Through it it is poured into the small intestine in small portions. The required amount of pancreatic secretion is regulated by the sphincter of Oddi.
Main functions of the ZhP:
- accumulation of bile produced by the liver,
- implementation and control of its receipt in the KDP.
Bile is produced by the liver constantly. It also continuously enters the hepatic duct and gallbladder. Up to 50 ml of bile can accumulate in the bladder (this is its volume), which, if necessary, thanks to the contraction of the muscle walls, enters through the excretory and common bile canal into the duodenum. A functional feature of the gallbladder is the ability to concentrate bile in such a way that in its space of 50 ml it accumulates in a highly concentrated form corresponding to a volume of 1 liter or more.
Bile and bile pigments are involved in the breakdown and absorption of lipids. The release of the contents of the gallbladder is associated with the digestion process and is controlled by the autonomic nervous system: the organ receives a signal that a food bolus (chyme) has entered the duodenum and contracts, releasing the secretion into the duct. This occurs in response to fatty foods. Otherwise, with continuous entry into the intestines (in the absence of food and intestinal contents), the organ mucosa would be damaged under the aggressive influence of acids.
The gallbladder is not an irreplaceable organ: after its resection, the function of storing bile is performed by the duodenum.
How is the gallbladder connected to the pancreas?
The gallbladder is connected to the pancreas anatomically and functionally.
Anatomically, the ducts of the pancreas (the Wirsung duct and the accessory duct, the Santorini duct, which is located in the head of the pancreas and can be connected to the main duct or be independent) and the common bile duct (gallbladder duct) flow into the lumen of the duodenum. There are several options for their final location:
- Type 1 - 55%: Wirsung and common bile are combined into a common ampoule,
- Type 2 - 33%: the ducts merge into one near the duodenum without forming an ampoule,
- Type 3 - 4%: channels are not combined,
- Type 4 - 8%: merge at a great distance from the nipple of Vater.
The connection between the organs is especially pronounced in the first type of duct structure, when they are combined into one common one to form an ampoule, into which both pancreatic juice and bile enter simultaneously. This structure often leads to pathology, since the common duct can be obstructed by a stone, tumor, or blocked by a polyp, stopping the release of contents into the intestine.
There is also a close functional connection between these organs. Digestion of food occurs with the direct participation of pancreatic juice containing enzymes. They are the ones who break down carbohydrates, fats and proteins into simpler components, which are absorbed into the blood and participate in further processes of human life. Bile acids, which are part of bile, stimulate the secretion of pancreatic secretions. In turn, the release of bile into the intestinal lumen is regulated by the humoral and nervous pathways.
Enzymes enter the duodenal channel in an inactive form. For their full activity, enterokinase is necessary - an enzyme produced by the cells of the wall of the small intestine. It becomes active under the influence of bile acids released by the gallbladder in response to signals from the autonomic nervous system when chyme (bolus of food) enters the duodenal lumen. The process of digesting food cannot occur without pancreatic secretion or bile. Any disturbance in their synthesis or entry into the duodenum leads to diseases of the digestive system and severe complications. Pathology in one of these organs can influence the development of changes in the other.
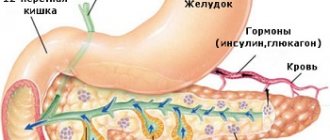
Function of internal (endocrine) secretion
The structure of the pancreas implies the presence of individual islets of Langerhans, which occupy 1-2% of its parenchyma. A number of hormones are released:
- Beta cells synthesize insulin. It is the “key” for the entry of glucose into cells, stimulates fat synthesis, reduces its breakdown, and activates protein synthesis. Produced in response to hyperglycemia.
- Alpha cells are responsible for the production of glucagon. Ensures the release of glucose from the depot in the liver, which increases blood sugar. Synthesis activates a decrease in glucose levels, stress, and excessive exercise. Inhibits insulin production and hyperglycemia.
- Delta cells synthesize somatostatin, which has an inhibitory effect on the functioning of the gland.
- PP cells synthesize pancreatic polypeptide, which reduces the excretory function of the gland.
Pancreatic juice is secreted when:
- evacuation of the food bolus into the duodenum;
- production of cholecystokinin, secretin and acetylcholine;
- the work of the parasympathetic nervous system.
Pancreatitis
From a clinical point of view, pancreatitis (inflammatory process of the pancreas) can occur in acute or chronic form. The cause of the disease may be the cessation of the flow of juice produced by the organ into the duodenum due to blockage of the duct. With prolonged inflammation, gland enzymes begin to digest their own cells. The cause of inflammation can also be damage to the gland due to its swelling.
Acute pancreatitis is most often caused by the presence of gallstones that block the ducts, or alcoholism, which results in obstruction of the small ducts of the organ.
Channels
The figure shows that the pancreatic ducts open into the duodenum.
- Santorini channel (additional).
- Small and large duodenal papillae.
- Wirsung's duct.
The most important is the Wirsung, it completely repeats the shape and bends of the gland and serves as a collector for the interlobular tubules. The ductal “tree” can be scattered, that is, the tubules flow into the main one in large numbers (about 60) and penetrate the entire thickness of the gland. The main type has about 30 tubules and they are located at a greater distance from each other.
The German anatomist Wirsung, who later received his name, became interested in the structural features of the main pancreatic duct. Wirsung noted that the course of the duct completely follows the shape of the pancreas. The source of the duct originates in the tail part and has a small diameter. In the body area the diameter becomes wider. At the level of the head, the duct bends slightly and merges with the common bile duct, having the largest diameter.
The formation of pancreatic secretion begins with small structures of the organ lobules - acini. The secretion exits through the intralobular ducts, and then they connect with the interlobular ducts, forming the main one. The formed pancreatic ducts open into the descending part of the duodenum.
Later, the scientist Vater described in detail the major duodenal papilla and, like many scientists, named it by his own name. The papilla is surrounded by the sphincter of Oddi. From Vater's observations, it became clear that the papilla is a single opening (95% of cases) for the pancreatic and common bile ducts. Study of cadaveric material showed that an additional minor papilla for the orifice of the accessory duct may be present. There is evidence that there is a special type of duct that occurs in 5% of cases. It begins in the thickness of the head, its migration is disrupted and it ends with the Helly sphincter on the wall of the duodenum.
Main pancreatic duct
The main channel is named Wirsung, in honor of the German scientist who discovered it for science. The main duct originates from the tail part of the organ and stretches to the duodenum 12. The flow of fluid is regulated by the sphincter, which is located at the end of the duct. Its size varies along its entire length - at first it has a diameter of two millimeters, towards the middle it reaches three, and at the edge it is already more than four. In appearance, the canal resembles an arc, which follows the structure of the pancreas.
The duct has small channels along its entire length that flow into it. Their number is individual for each person, and, depending on this, their distance changes. There are two types of ducts - main and loose, with the first type there can be about 35 canals, and with the second type there are more than 60. With the main form, the distance between the ducts varies by about 1.5 cm, but with the second type it is significantly reduced. The length of the main stream can reach 20 centimeters.
Classification
The excretory ducts consist of two large ones (main pancreatic and accessory) and many small ones, originating in the lobules of the pancreas. The mucous membrane of the ducts contains cells that produce the hormone cholecystokinin, which is involved in managing digestion (controls the feeling of fullness and appetite).
Main
Its second name is the Wirsung duct. It begins in the tail of the pancreas, passes through its entire body, then, connecting with the common bile duct, approaches the large preudenal nipple, through which it exits into the duodenum. The main duct has a length of up to 25 cm. Its diameter in the tail part of the pancreas is up to 1.5 mm, in the body of the gland - approximately 2.5 mm, and in the head - up to 3.3 mm.
Additional
It is also called the Santorini channel. It begins in the head of the pancreas, then merges with the main duct (in some people, the accessory duct has an independent outlet into the digestive tract).
Norms for the size of the Wirsung duct of the pancreas
The type of main duct depends on the individual characteristics of the human body. More often it resembles an arc in shape, but there is also a knee-shaped type. Patients also have an S-shaped canal, which exactly follows the shape of the pancreas.
In the body, the main duct is similar in its properties to a river into which small streams flow. Their shape and size largely depend on their number. The more channels included in the system, the wider it is. There is a certain standard at which minor deviations are acceptable:
- the head measures about 3.3 mm;
- the body varies in diameter from 2 to 3 mm;
- the tail can be from 1 to 1.7 mm.
Structure and functions
Small excretory ducts flow into the main canal along its entire length, the number of which varies depending on individual characteristics (from 20 to 60). The anatomical structure of the pancreatic canal is characterized by great variability. Approximately 60% of people have a joint exit of the bile duct and the main pancreatic duct through the major preudenal (Vaterian) nipple into the duodenum.
Not everyone has an accessory duct of the pancreas, and if it is present, individual anatomical features also have variations. Research data does not yet provide a clear percentage of all forms of structure; according to rough estimates, about a third of humanity has a separate outlet for the additional duct through the small preudenal nipple. The function of monitoring and regulating the flow of secretions into the gastrointestinal tract is carried out at the exit of the ducts.
Where do the pancreatic ducts drain?
The main duct merges with the common bile duct through a separate pancreatic sphincter. After fusion, they form the ampulla of the nipple of Vater, inside which there is a smooth circular muscle - the sphincter of Oddi. This organ plays the role of a valve that controls the flow of bile and pancreatic secretions into the digestive tract, preventing reuptake. Until the digestion process begins, the sphincter of Oddi is contracted. When food enters the duodenum, the sphincter opens, allowing the release of bile and enzymes.
Developmental defects
In addition to individual characteristics, anomalies and developmental defects are noted in the structure of the ducts. In approximately every tenth individual, the final section of the main duct is atrophied; the entire pancreatic secretion enters the duodenum through the additional duct. Even less commonly (about 4%), separate exits of the bile and pancreatic ducts are observed.
A rare anomaly is an accessory (aberrant) pancreas. This is a separate local accumulation of pancreatic tissue, which may have its own output channel.
Structural anomalies
More often, an anomaly in the structure of the pancreas is associated with a genetic defect. There was a malfunction during the formation of the organ. In the case where the main duct has two branches, a person has congenital stenosis. Then problems arise in the output channels. In most cases, they narrow, which provokes the development of various pathologies of the digestive system. The most common disease of the pancreas is pancreatitis. It can occur in a chronic form, that is, it forms an inflammatory process in the pancreas. It may also be accompanied by neoplasms in the head of the organ. The formations quite often develop into malignant tumors, and the patient is diagnosed with oncology. If the patient does not start treatment on time, surgical intervention will not be possible. The surgeon needs to remove part of the organ so that nothing threatens the person’s life.
Important. If there are disturbances in the ducts, changes in the water balance may occur, which leads to cystic fibrosis. The biliary tract is directly connected to the duct system in the pancreas. With any pathology with them, a person has problems with digestion and the pancreas.
In addition, the main duct can not only narrow, but also expand. This is a consequence of other disorders. For example, this occurs in the presence of cyst formation or pancreatitis. The main and accessory pancreatic ducts enlarge due to swelling of the soft tissues around the organ. Symptoms appear depending on the diseases themselves. A change in the size of the duct can only be treated with complex therapy, that is, the disease itself must be eliminated. With proper and qualified treatment, the ducts will restore their normal size and function correctly. The most important thing is to pay attention to the emerging signs of digestive disorders in time. Since it is much easier to cure the initial form of the disease. Indeed, in severe cases it will take more time, and it is also possible that the doctor will prescribe surgery. And the removal of part of the organs leads to the fact that the internal systems will no longer function normally, as in a healthy body. You will need to follow a certain diet. To identify violations, it is necessary to undergo a complete examination of internal organs every six months.
We also recommend viewing: Medicines for a sick pancreas: what, why, for how long?
Causes of anomalies
Some pancreatic duct anomalies have genetic causes. Other defects develop under the influence of bad habits of the mother or intrauterine infections.
Long-term use of certain drugs can affect the fetus and lead to the development of anomalies.
An increase in the diameter of the main duct may indicate chronic pancreatitis, the presence of stones; less often, a tumor of the head of the pancreas or ampulla of the nipple of Vater can be suspected. Also, dilation of the Wirsung duct can be caused by postoperative adhesions or injuries.
Pathologies of the pancreatic ducts
Changes in structure and deviations in the structure of the ducts are developmental anomalies. But acquired pathology has also been described.
Genetic defects can cause the common canal to bifurcate: it splits into two branches.
The main pathologies of the ducts include:
- stenosis;
- extension;
- obstruction;
- inflammation.
Cystic fibrosis develops in the pancreatic parenchyma due to stagnation and changes in fluid.
When the ducts narrow, the areas preceding the stenosis expand, which leads to stagnation in them. When the duct of Wirsung expands, increased pressure is created in this place.
Blockage of the main duct is the main cause of pancreatitis. There is blockage of small channels and their expansion behind the site of stenosis - increased pressure is created in them.
Causes and symptoms
The norm of the duct is established: it must have smooth walls, and the lumen must be clean, without stones. When the duct is pathological, the surface of its internal walls becomes uneven - this further worsens its condition. To detect such changes on ultrasound, it is necessary to visualize not only the head of the pancreas, but also the entire biliary tract.
Reasons for dilated ducts include:
- malignant formation of the head of the pancreas or the ampulla of Vater's papilla of the duodenum - this is accompanied by obstructive jaundice;
- stones blocking the patency of the common pancreatic duct, which are often combined with gallstones and dilatation (expansion) of the common bile duct;
- chronic inflammatory process in the pancreas;
- strictures that developed after operations (partial pancreatectomy, Whipple resection).
When a tumor develops or stones form, there are no symptoms until the formation increases to 4 cm. This increases the danger of the disease and the complexity of diagnosis: only when it reaches impressive volumes does the tumor or stone begin to disrupt the functioning of the organ. As a rule, pancreatic cancer is detected at stages 3 or 4, when the tumor is already actively growing in vital organs and vessels, which makes it impossible to completely remove it. The chances of survival in such cases are extremely low.
Since the common bile duct is also involved in the process, connecting in most cases in the area of the head of the pancreas with the Wirsung duct, one of the first signs is jaundice. According to the mechanism of development, it is obstructive, mechanical. Cholecystitis develops. Subsequently, stones form that can clog the gallbladder and its ducts. The pathological process intensifies, the bladder clogged with stones becomes inflamed and transforms into cholelithiasis (GSD).
In addition to jaundice, other symptoms appear:
- pain of varying intensity in the left hypochondrium with irradiation to the lower back;
- decreased appetite and rapid weight loss;
- nausea, vomiting, discomfort in the stomach when eating - since the stomach, liver, small intestine and large (colon) and other digestive organs border the pancreas and are involved in the pathological process;
- thirst, general weakness, sharp decrease in ability to work.
According to medical statistics, stones in the ducts rarely develop, but are included in the list of pancreatic pathologies. They can occur independently or be the result of pancreatitis. If the stone has formed in the Wirsung canal, obstruction occurs at the site of its localization and intraductal pressure increases. The enzymes are not discharged into the duodenum; under pressure they retrogradely enter the gland tissue, and the process of autolysis—self-digestion—begins. The parenchyma of the gland is destroyed - pancreatic necrosis develops, and massive death of pancreatic cells occurs. This corresponds to severe pancreatitis with high mortality. Conservative therapy is ineffective. Treatment is carried out surgically.
Diagnostics
Diagnosis is carried out using laboratory and instrumental research methods.
Laboratory tests include the determination of biochemical tests:
- diastasis of blood and urine;
- transaminases (ALT, AST, GGT), bilirubin, total protein and fractions;
- coprogram - stool analysis.
In addition, the following are used:
- Ultrasound of the abdominal organs and retroperitoneal space;
- EFGDS – esophagoduodenoscopy;
- CT or MRI;
- angiography of the pancreas;
- laparoscopic diagnosis.
The simplest method of functional diagnostics is ultrasound. If you look at the entire pancreas, from head to tail, there is a noticeable change in the diameter of the main common duct: the lumen of the channel increases in size. You can also clearly see the parenchymal organs adjacent to it, determine the increase or decrease in the size of the gland itself and the main duct, identify pathological formations in the form of cysts, stones, tumors, and evaluate the density and homogeneity of tissues. Inflammation in the parenchyma of an organ can significantly increase its density, as well as the thickness of the walls of the ducts. In this case, the Wirsung duct and changes in it may not be visualized, and additional research methods must be performed to clarify the diagnosis.
FGDS allows, using a special optical device, to assess the condition of the mucous membrane of the esophagus, stomach, and duodenal bulb, and to detect narrowing of the duodenum with an annular pancreas.
To obtain layer-by-layer sections, MRI is prescribed - the most accurate way to study the Wirsung duct in detail.
Treatment
Asymptomatic pancreatic ductal anomalies do not require treatment. Therapy for pathology of the pancreatic excretory ducts is reduced to the correction of diseases that have caused changes in the ducts or their complications. It depends on the severity of the disease and the extent of damage to the pancreas. Conservative and surgical treatment methods are used.
All patients with functional disorders of the pancreas in terms of complex therapy are prescribed diet No. 5p according to Pevzner. She excludes fatty, fried, spicy, smoked, and salty foods. During periods of exacerbation of diseases of the digestive tract caused by enzyme disorders, it is recommended to take food in small portions 5-6 times a day. Food should be steamed, boiled or stewed, but not fried. It is necessary to include a sufficient amount of easily digestible proteins (lean meat, fish), a lot of fiber (porridge, thermally processed and chopped fruits and vegetables).
Enzyme replacement and, if necessary, glucose-lowering therapy are prescribed for impaired carbohydrate metabolism.
In the intensive care unit, a group of drugs that have an antisecretory effect is used - protease inhibitors. They inhibit the secretion of enzymes by the pancreas - Contrical, Trasylol, Gordox. Pantripin. Recently, their role in treatment has decreased, and their use is limited due to high side effects - severe allergic reactions, which in severity and danger exceed the therapeutic effect.
In addition, therapy consists of a set of measures that help restore the functional activity of the digestive organs. For this we use:
- antispasmodic, anticholinergic, analgesic drugs for pain relief;
- novocaine blockade for high intensity pain;
- artificial somatotropin - growth hormone (Octreotsid, Sandostatin), to reduce the production of enzymes;
- proton pump inhibitors for increased acidity of gastric juice, which significantly enhances the synthesis of pancreatic enzymes;
- antibacterial drugs to treat or prevent infection in combination with an antimicrobial drug (Metronidazole);
- antihistamines;
- diuretics for swelling of the pancreas.
Symptoms
An abnormal structure of the ducts may have no clinical manifestations at all; sometimes the symptoms are subtle. To recognize symptoms, it is important to have a clear understanding of the relationship between pathologies of the ducts (pancreatic and common bile) with the functioning of the pancreas and gallbladder.
A change in the diameter of the pancreatic ducts or their spasm is manifested by disturbances in the functioning of the digestive system - abdominal pain (colic), diarrhea, constipation.
Symptoms are more pronounced when acute pancreatitis occurs. Intense pain in the projection of the pancreas (or encircling pain), nausea, vomiting is observed, after which brief relief occurs. The pain often radiates to the back; the person strives to assume the fetal position, which gives a slight improvement in the condition.
Pancreolithiasis
Pancreolithiasis is a pathological condition characterized by the formation of stones in the Wirsung duct of the gland or its branches. Signs of the disease are spasmodic pain in the epigastric zone, radiating to the lumbar region.
The presence of stones, preventing the outflow of pancreatic juice, leads to digestive disorders. With such stagnation, ultrasound reveals that the Wirsung duct is dilated, and stretching of the walls of small ducts is observed.
However, it is worth remembering that the ultrasound picture does not provide complete information for making a diagnosis. Additional examinations are necessary. Since often when diffuse modifications of the pancreas or liver are detected, for example, the Wirsung duct is not visualized. Other diagnostic methods help to study it in more detail.
Diagnostics
Existing diagnostic methods make it possible to detect minimal pathologies of the ducts. Ultrasound is the most commonly used. With this study, the main duct is clearly observed, it is possible to assess its size and detect narrowing or expansion.
Sometimes some area of the ducts is not visualized or the procedure is difficult (for example, with excess body weight); in such cases, endoscopic ultrasound is used, which is a combination of ultrasound and endoscopy and allows the sensor to be brought directly to the object of study.
The most informative technique is endoscopic retrograde cholangiopancreatography (ERCP).
During the procedure, the doctor, under the control of an endoscope, fills the canals with an x-ray contrast agent, after which he observes the ducts using an x-ray unit. The disadvantage of this method is its invasiveness.
Laboratory tests are also important: a biochemical blood test, determining the concentration of pancreatic digestive enzymes (their deviation from the norm towards a decrease indicates the presence of a problem).
How to diagnose and distinguish pathologies?
Pathologies of the pancreas and gallbladder have much in common in their clinical symptoms. With pancreatitis, as with inflammation in the gallbladder, there may be pain in the right hypochondrium. The pain becomes intense after breaking the diet and consuming fatty, spicy, fried foods, alcohol, even in small quantities.
Physical activity and stress can also cause discomfort and pain in the hypochondrium, radiating to the arm, shoulder, lower back, and with pancreatitis they become encircling.
Dyspeptic manifestations appear:
- nausea,
- vomit,
- heartburn,
- belching,
- flatulence.
Symptoms of asthenic syndrome occur:
- severe weakness
- fatigue,
- bad dream,
- lack of appetite.
It is sometimes difficult to differentiate the exacerbation of a chronic inflammatory process in the gland and the gallbladder due to the similarity of the clinical picture, which, with a certain history, can be associated with each of the digestive organs. Features of pancreatitis are:
- pancreatic diarrhea - fatty grayish frequent stools with a foul odor and remnants of undigested food (one of the first manifestations of the disease),
- repeated vomiting that does not bring relief,
- pain of various localizations.
The pathology of the gallbladder, in addition to the listed signs, is manifested by biliary hypertension caused by stagnation of bile. Manifests:
- yellowness of the skin and mucous membranes,
- itchy skin,
- enlarged spleen, and subsequently hypersplenism syndrome (anemia, leukopenia, thrombocytopenia),
- ascites in severe cases without treatment.
Clinical manifestations are not enough to identify the affected organ. The patient needs to be examined in detail, the functions of the gallbladder and pancreas should be checked. To exclude volumetric processes, it is necessary to check the condition of the organ using functional studies:
- Ultrasound,
- MRI,
- CT,
- splenoportography – radiography of the vessels of the portal system with contrast,
- Dopplerography of liver vessels.
These methods make it possible to determine the condition of the parenchyma and borders of the pancreas, walls, the presence of stones, polyps, and other formations in the pancreas.
Laboratory tests include a number of indicators that need to be checked to clarify the diagnosis:
- general clinical blood test,
- blood for sugar
- diastasis of urine and blood,
- bilirubin (total, direct, indirect),
- total protein and its fractions,
- cholesterol, alkaline phosphatase,
- coagulogram.
The doctor individually prescribes specific examinations, taking into account complaints, anamnesis, objective status and the severity of the condition for which the patient presented. Based on the data obtained, medications are prescribed or the issue of other treatment methods is decided.
Treatment
The goal of conservative therapy is to relieve inflammation and pain. The general practitioner prescribes treatment that coincides with the elimination of pancreatitis. It includes:
- refusal to eat for 1-2 days;
- antispasmodics;
- preparations containing digestive enzymes.
Sometimes surgery is required for stenosis of the Wirsung duct.
Diet
In the complex treatment of diseases of the pancreatic ducts, healthy nutrition will occupy an important place, which must be adhered to for a long time.
The diet is aimed at reducing the secretion of the gland. This is achieved by adjusting the composition, single volume and meal schedule. The protein component should predominate in the diet; it is necessary to avoid salty, spicy, fatty, fried and vegetable fiber. It is preferable to steam food.
Cold and too hot dishes are prohibited; meals should be taken at the same time. The daily amount of food should be divided into 5-6 meals; overeating is prohibited. It is better to use yesterday's bread. In many hospitals and sanatoriums, the required diet is called diet No. 5.
How to clean the pancreatic ducts
Cleaning the ducts is a dubious measure that does not have the approval of official medicine. If stones are present, stimulating secretion may lead to blockage of the duct. But in case of stagnation, the excretory channels can gradually become clogged with clots of pancreatic juice, which leads to the formation of stones.
Some folk recipes aimed at preventing secretion stagnation have reasonable physiological grounds, but their use requires a reliable exclusion of stones in the pancreatic and bile ducts. Before starting the procedures, you should limit your diet for a week: exclude alcohol, fried, salty, fatty, spicy foods, drink as much water as possible. Recipe examples:
- Pour 6-8 bay leaves with 1 glass of boiling water and leave in a thermos overnight. Drink 50 g of infusion before each meal for a week;
- in the evening, pour 1 glass of buckwheat with 0.5 liters of low-fat kefir, eat half of the resulting mass for breakfast, and the other half 2 hours before bedtime.
Other herbal remedies that help cleanse the pancreatic ducts include parsley and chicory roots and sea buckthorn leaf.
Ultrasound picture
Modifications of the pancreas (disturbance of the organ parenchyma) can be caused by various causative factors. They are visible during ultrasound examination, which allows you to assess the size and structure of the parenchyma, see the contours, the presence of pathologies, as well as the condition of the gland ducts. Signs of individual diseases diagnosed during the examination also show probable abnormalities that may affect the pancreatic duct of Wirsung.
By the way, it is worth noting that many healthy people may experience symptoms of diffuse changes associated with the environmental situation and the consumption of products with various preservatives and stabilizers.
Prevention of duct diseases
Primary prevention is aimed at eliminating the negative effects of bad habits, psycho-emotional fatigue, lack of sleep, and abdominal injuries. Maintaining an active lifestyle, creating a favorable psychological environment, healthy eating - these recommendations help to avoid diseases of the pancreas and ducts.
Secondary prevention is needed if the disease has already been diagnosed. To prevent exacerbations, it is important that the pancreas functions without overload, the ducts regularly remove secretions through the sphincters, which open and close on time. Following the doctor's instructions and following a diet will help normalize all processes and prevent relapses.
Symptoms of the disease
The clinical picture of an ectopic organ depends on its location and size. When the accessory duct is located on the wall of the stomach, a person will feel the symptoms of gastritis: heartburn and pain after eating. If the pathology is localized in the duodenum area, the victim will feel pain in the left upper abdomen, nausea, and weakness. Many people do not have any signs of having an additional organ in their body. Symptoms begin to appear when the following complications occur:
Symptoms begin to appear when constipation occurs.
- constipation;
- intestinal obstruction;
- inflammatory process;
- necrosis;
- bleeding.
When the diameter of the lumen in the canals changes, a person feels colic and abdominal pain, muscle spasm. His digestion is disrupted.
Anomalies of duct development
Anomalies of the ducts are a deviation from the norm of their anatomical structure or functional activity. Anomalies of the pancreatic outlet channels are:
Anomalies that are present at birth include:
- absence of the Santorini excretory canal;
- separate entry into the small intestine of the Wirsung and accessory ducts;
- cystic changes in the ducts;
- annular pancreas, in which the duct has the shape of a loop;
- spiral pancreas (the common canal of the gland is also spiral-shaped);
- additional pancreas.
Acquired anomalies include fibrocystic pancreatitis, which occurs primarily in infants. This is most often associated with atresia - pathological underdevelopment or complete absence of canals, which results in cystic formations. The absence or sharply reduced number of tubules leads to the fact that enzymes do not enter the intestine, and their quantity in the intestinal juice is sharply reduced. This causes a disruption in the processes of digestion and absorption of nutrients in the intestines. This state gradually leads to:
- to low weight gain of the baby with good appetite;
- to the gradual exhaustion of the child for no apparent reason;
- to stunting;
- to intestinal obstruction.
If a child is born with an annular pancreas anomaly, it may not show any clinical signs throughout his life. Sometimes it is discovered by chance during a detailed examination only in old age. The pancreatic duct in such cases forms a loop. The abnormal development lies in the fact that the pancreas tissue encircles the descending part of the duodenum, gradually narrowing its lumen over time. In this case, incomplete development of the ducts leads to stagnation in the antrum of the stomach and, as a consequence, to disruption of the duodenal bulb. Against this background, the following are developing:
- peptic ulcer of the stomach or duodenum;
- cholelithiasis.
It has also been established that the development of all acinar glands, which include the pancreas and the salivary glands (including the sublingual glands), proceeds in the same way. There is a connection between the congenital pathology of these glands. Sometimes there is a congenital expansion of the common bile duct - the common bile duct - with the further development of the inflammatory process - cholangitis.
Causes of anomalies
The causes of abnormal duct development are unknown in most cases. Most often they are caused by:
- genetic changes;
- adverse factors to which a pregnant woman is exposed: smoking, alcohol, drugs, as well as the effects of radiation, high temperature;
- infections in a woman during pregnancy: rubella, herpes, listeriosis (affects immune tissues and the liver) and others;
- constant stressful situations;
- use of drugs prohibited for pregnant women.
Due to untimely diagnosis and lack of adequate treatment, changes in the ducts of the pancreas can gradually lead to disruption of the digestive processes and irreversible consequences in the tissues of the organ. To avoid this, you need to be attentive to your health, give up bad habits, eat right, avoid stress, and if you feel unwell, consult a specialist without self-medicating.
The pancreas plays an important role in the body's digestive system. The two main functions of the pancreas are intrasecretory and exocrine. In this regard, it is called mixed. One part produces pancreatic juice, and the other releases hormones. Thereby regulating metabolism in the body.
Pancreatic ducts
An auxiliary function is the process of producing and controlling insulin, which determines blood sugar levels.