Problems with the pancreas are familiar to a fairly wide range of people. Pancreatitis affects neither adults nor children. And the earlier the disease is detected, the more effective the treatment will be.
Ultrasound examination helps to clearly see the clinical picture. The picture on the monitor screen will show what the pancreas looks like and how rooted the disease is in the body.
Types of pancreatitis
Inflammation of the pancreas has three types: acute, chronic and reactive. The acute form of the disease is characterized by changes in the tissue (it disintegrates), hemorrhage and accumulation of purulent substance are possible.
In the chronic form, the disease progresses slowly. A constant diet and medication are required.
A disease is called reactive if an attack of acute pancreatitis occurs along with the onset of diseases of the liver, stomach, duodenum, and gall bladder.
Ultrasound diagnosis of the pancreas
Ultrasound diagnostics of the pancreas allows us to examine deviations from the norm and modifications of the organ, which may indicate an acute or chronic inflammatory process. An indicator of dysfunction of the organ is, first of all, uneven, convex, lumpy , unclear contours of the pancreas
, or tissue modifications. Thus, a vague outline may indicate diseases of the stomach, duodenum, or the onset of inflammation and swelling in the pancreas. If the contour is convex and smooth, it indicates a cyst has formed on the gland.
An uneven contour is an indicator of pancreatitis or new growths. If the contours are lumpy or blurred, then you should undergo a more in-depth examination to determine cancer. An ultrasound will also help determine the condition of the pancreatic tissue. The density of the fabric should be medium. If its increase is detected, this may indicate a chronic form of pancreatitis.
Symptoms of the disease
In the chronic form, the patient experiences pain in the upper abdomen. Painful sensations can be felt in the left, less often the right hypochondrium. Appear due to poor diet and alcohol consumption. The pain can be either dull or sharp. There is also a feeling of nausea and bouts of vomiting.
The acute form is characterized by the following picture:
- sudden, severe pain in the upper abdomen, leading to shock, can radiate under the left shoulder blade,
- debilitating vomiting,
- diarrhea.
With reactive pancreatitis, the patient experiences pain, cutting and dull, of a girdling nature. There is a taste of bile in the mouth, and vomiting is also characteristic.
What can be determined using ultrasound
All patients with inflammation of the pancreas are prescribed an ultrasound examination. It is carried out for both acute and chronic pancreatitis, and if the disease is suspected.
An ultrasound will show the condition of the contours and tissues of the gland:
- if the contour is blurry, it means that inflammatory changes are occurring in the pancreas and swelling has begun. But it may also be evidence of a disease of the stomach or duodenum,
- the contour is convex, but at the same time smooth - a cyst has formed on the gland,
- uneven outlines are characteristic of pancreatitis and neoplasms,
- lumpy, blurry edges indicate cancerous formations.
An ultrasound examination also demonstrates the condition of the pancreatic tissue. In a healthy person it is of medium density. If the density is increased, it means that the connective tissue has grown. This condition is typical for chronic pancreatitis, but may be evidence of age-related changes. There are white areas on the screen.
If the fabric density is reduced, the image on the screen will be black. This condition is typical for the acute form of pancreatitis.
At each stage of the disease, the contours of the pancreas and its structure change. In the first stage of the acute form of the disease, the contours of the pancreas are blurred and uneven, the density is reduced, and the duct is dilated.
At the second stage, a cyst or abscess may appear. The contour will be rounded, the density of the tissues will decrease.
With chronic pancreatitis, the contours become unclear. If stones appear in the gland, the contour will become rounded, and the density in this place will increase.
What does the blurred contours of the pancreas indicate?
As mentioned above, the gland has several variants of a normal ultrasound image, so normally it can be either homogeneous or coarse-grained. It is important to understand that uneven contours of the pancreas are not the only criterion by which pathology can be suspected or confirmed.
When examining abdominal organs, including the pancreas, ultrasound doctors evaluate their location, size, density, structure, evenness and clarity of boundaries, and the nature of blood flow. With normal sizes of the head, body and tail of the pancreas, fuzzy contours are normal and do not require special attention.
In some cases, uneven or unclear contours can be caused by inflammatory or structural pathologies:
- Cysts are most often round, anechoic (“black” on the screen) formations with clear and thin boundaries that can deform the contour of the gland and compress the lumen of the main large duct. They are divided into true and false. The last type of cyst (pseudocyst) is often a consequence of an acute inflammatory process (pancreatitis) or trauma.
- Abscesses are pus enclosed in a cavity. On ultrasound they are detected as hypoechoic, round or irregularly shaped areas with a heterogeneous echostructure. In the color flow mode, the blood flow is single or absent at all. Such changes are always accompanied by a clear clinical picture: fever, chills, severe pain in the projection of the abscess.
- Tumors can have a structure identical to the gland, clear boundaries and a round shape. Malignant neoplasms are usually heterogeneous, large, deform the contour of the organ, and have pronounced mixed blood flow. Their most common location: head or tail. Sometimes tumors compress the excretory duct, causing reactive swelling of the pancreas.
- Acute pancreatitis is a severe inflammation of the gland, which has vivid symptoms. Due to diffuse edema, the organ increases in size, its echogenicity decreases, and the parenchyma becomes clearly heterogeneous. Contours lose their clarity and become blurred. The Wirsung duct is significantly expanded. After some time, cysts, abscesses or hemorrhages may appear in the gland.
Chronic pancreatitis also leads to changes in the evenness and clarity of the boundaries, in which connective tissue grows in the gland and small calcifications appear. All this deforms the organ, giving it a characteristic ultrasound picture.
Cyst and tumor
If a black tumor with smooth, well-defined edges is visible on the pancreas during an ultrasound, this is evidence that fluid has accumulated in these places (a cyst has grown) or pus has accumulated.
Cancers of the gland appear as black or white spots. It depends on what type of cancer is developing in the body. Mixed cases are possible.
With anomalies of the pancreas, two pancreatic ducts and a blurred structure are visible that unevenly transmit ultrasound flows.
Dilated pancreatic duct on ultrasound
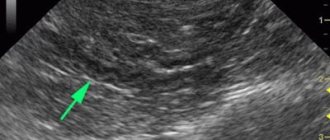
The internal diameter of the normal pancreatic duct is less than 3 mm. The duct is better visualized with transverse scanning in the middle third of the body of the pancreas. In order to make sure that you have found the duct, you need to see the pancreatic tissue on both sides of it. The splenic vein posteriorly or the gastric wall anteriorly may be falsely interpreted as the pancreatic duct.
The walls of the pancreatic duct should be smooth and the lumen should be clean. When the duct is dilated, the walls become uneven; scan not only the head of the pancreas, but also the entire biliary tract.
The main causes of dilatation of the pancreatic duct: tumor of the head of the pancreas or ampulla of Vater's papilla (combined with jaundice and dilatation of the biliary tract); stones of the common bile or pancreatic duct; chronic pancreatitis; postoperative adhesions.
| Photo. A man with insulin-dependent diabetes mellitus complains of weight loss and abdominal pain for several months. Ultrasound shows an enlarged common pancreatic duct with an uneven wall. Upon further examination, calcifications with a shadow behind them are clearly visible in the duct (B). |
| Photo. A patient with acute pancreatitis: a large pseudocyst has formed at the level of the tail (see above), the dilated pancreatic duct opens into a pseudocyst. |
How to prepare for an ultrasound
First of all, it is necessary to organize proper nutrition. Do not consume foods that promote gas formation: soda, sweets, legumes, mayonnaise, cabbage, etc. Gases inflate the intestinal loops, which, in turn, close the pancreas. The study may fail.
To reduce gas formation, it is appropriate to take adsorbents, pancreatic enzymes, and carminatives.
During the period of preparation for ultrasound examination, you should reduce the consumption of meat and meat products, dairy products, and fish. And it also follows:
- exclude alcoholic drinks,
- forget about smoking,
- you can take medications that reduce gas formation,
- The last meal should take place 6–8 hours (in children 3 hours) before the start of the study.
Preparing for an ultrasound and what a healthy pancreas looks like
Calcifications inside the pancreas can give an acoustic shadow, but if they are small, they appear as a separate bright echostructure without an acoustic shadow. In chronic pancreatitis, calcifications are distributed diffusely throughout the pancreas. Stones in the duct are located along the duct.
| Photo. A - There is a small stone in the dilated duct. B - In the dilated pancreatic duct there is a row of several stones with shadowing behind. B — A patient with chronic pancreatitis has huge stones in the dilated duct. Note the intense shading behind. |
| Photo. A, B — Calcifications in the pancreatic parenchyma in patients with chronic pancreatitis. Some calcifications have a shadow. B — A 5-year-old boy with chronic hereditary pancreatitis: calcifications (small arrows) and dilatation of the pancreatic duct (large arrow). C - confluence of the superior mesenteric and splenic veins. |
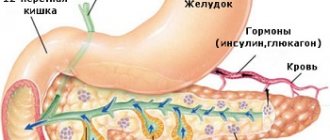
The pancreas is a parenchymal (dense in structure) organ, which consists of lobules and interlobar septa, and is functionally divided into two parts: endocrine and exocrine. The first produces hormones (glucagon and insulin) directly into the bloodstream, and the second - into the lumen of the duodenum (somatostatin, gastrin, lipase, amylase).
Most of the organ is located in the retroperitoneal space, that is, outside the abdominal cavity. Normally, the gland consists of a head, sometimes an isthmus, a body, a tail and has an S-shape. In some cases, there are other variants of the structure of the organ, which are classified as developmental anomalies:
- ring-shaped;
- spiral pancreas;
- aberrant gland (accessory);
- split.
Ultrasound examination of the pancreas is a safe and informative diagnostic method in which inflammatory, traumatic changes or tumors can be detected. The study is usually carried out on the back, the sensor is installed in the epigastric region in a transverse position.
With a fixed inhalation or exhalation (optimally - inflate the stomach upward), the doctor manages to fully remove the gland. Sometimes, due to a pronounced subcutaneous fat layer or flatulence, only its head and body are visualized.
An ultrasound image of an unchanged gland can have a different appearance, both in its echogenicity and in its structure. It should be remembered that the echogenicity of a normal pancreas is equal to that of the liver, but may be slightly higher or lower. An important criterion is that the density of the organ should not exceed the density of the surrounding fatty tissue (it is “white” on ultrasound).
The pancreatic parenchyma is fine- or coarse-grained, sometimes with thin hyperechoic layers in the form of “cut meat,” which sonologists mistakenly take for signs of chronic pancreatitis. In older people, its echogenicity is practically equal to the echogenicity of the surrounding tissue due to natural age-related changes. In this case, the contours of the pancreas are uneven and unclear.
In a small number of cases, the Wirsung duct can be slightly dilated in healthy people (through it the gland releases its enzymes into the lumen of the duodenum). Do not forget that ultrasound is an operator-dependent diagnostic method, so sometimes difficulties arise in interpreting the data obtained.
To investigate and evaluate diffuse changes in the pancreas, reviews are collected according to all international recommendations. The correct conclusion is the immediate task of the sonologist and the prescription of therapy by the treating doctor.
But improper patient preparation can lead to incorrect diagnostic decisions and incorrect treatment.
First of all, the patient should follow a number of the following recommendations:
- It is not recommended to eat food 12 hours before the procedure.
- You should have a bowel movement the day before the test.
- Ultrasound is performed on an empty stomach and in the first half of the day.
- A few days before the procedure, the patient excludes from the diet all foods that contribute to excessive gas formation.
- If the patient has flatulence, then sorbents should be taken.
With ultrasound screening, the organ is completely accessible for inspection. All its parts are visually accessible.
The shape of the organ resembles the letter “S” of the English alphabet.
A healthy gland has normal sizes and smooth, regular walls. The contour is correct without any deviations from the norm.
The structure of the organ is in most cases homogeneous, but some hyperechoic inclusions may be present.
Adjacent organs are also examined, including the liver, parts of the intestines, and kidneys.
Often changes in these organs can affect the structural state of the pancreas.
It is worth remembering that even if there are suspicious signs on an ultrasound, you should not panic. An accurate diagnosis often requires a number of laboratory and instrumental tests, ranging from a simple blood test to a trephine biopsy of gland tissue.
After the procedure, the sonologist, within a short period of time, deciphers the sensor readings and gives the wording to the patient.
Signs of pancreatic diseases are discussed in the video in this article.
Sugar level
Man
Woman
Enter your sugar or select your gender to get recommendations
When ultrasound is prohibited
The doctor will not prescribe an ultrasound if there is an allergy to the gel used or if the patient’s life is at risk. When the patient's condition has stabilized, an ultrasound examination can be performed. Patients who are obese in the third stage do not undergo such testing, since there is no good overview.
If there are abrasions and wounds, an ultrasound will also not be performed. This is because it is impossible to get good contact. The result is a bad review.
In case of problems with the pancreas, it is necessary to organize treatment correctly and in a timely manner and undergo tests determined by the attending physician. Relying on your own strength and grandmother's remedies is a dangerous game with your health.
1
When does such a change in an organ occur?
Normally, the pancreatic margin and the parenchyma of the organ itself are clearly visualized on ultrasound.
But under some circumstances and diseases, a wavy area, scalloped angle and other changes in echogenicity may be visualized.
Changes can be local or diffuse.
These are important diagnostic criteria for establishing the prevalence of the process.
A diffuse process occurs in the following pathologies:
- Swelling or anasarca. Swelling of internal organs occurs when they are directly affected or due to secondary damage in the case of pathology of another organ. Primary edema occurs in the case of pancreatitis. In this case, swelling is an indication for immediate treatment. Anasarca is swelling of all organs and tissues of the body, including the pancreas. This condition develops due to severe damage to the cardiovascular system or renal filter.
- Autolysis or necrosis of pancreatic tissue. This is an extremely severe surgical pathology, which is a consequence of acute pancreatitis. In this case, all functional active cells of the organ die, and the pancreas is not clearly differentiated. Autolysis is accompanied by the release of a large number of enzymes into the bloodstream. During a blood test, the doctor notes how the enzyme activity of the blood increases.
- Fatty degeneration of pancreatic tissue. In this case, active cells are replaced by inactive adipose tissue. The process is chronic and is not accompanied by severe symptoms.
- Type 1 diabetes mellitus, despite its hormonal nature, has a pathological focus. In the first type of disease, death occurs by the islet of Langerhans diffusely throughout the organ and this is noticeable on ultrasound.
- Tumor process of an organ or metastatic lesion. To exclude cancer, a number of other studies should be performed, such as MRI, CT and biopsy.
- Polycystic lesions or multiple cysts of the organ. Such pathological foci have a clear appearance and a smooth edge; phenomena are characteristic of a disease such as cystic fibrosis.