Echogenicity in medicine is a term that refers exclusively to ultrasound diagnostics. It characterizes the ability of tissues to reflect ultrasonic waves, delaying their penetration into deeper layers. Accordingly, the denser the organ, the more waves it will reflect, the brighter the image on the monitor screen will be. This condition is interpreted as an increase in the echogenicity of structures.
Physical basis of pancreatic echogenicity
An ultrasonic sensor emits ultrasonic waves that easily pass through air structures and are reflected from denser ones. Normally, the pancreas has an average tissue density (not liquid, not dense) and evenly reflects waves over its entire surface. The returning waves are captured by the same sensor, which is recorded on the monitor screen.
Important! Increased or decreased echogenicity of the pancreas is not a diagnosis. Such changes are only a sign of the presence of a chronic pathological process in the organ. In this case, the doctor is obliged to prescribe additional diagnostics in order to establish the underlying disease and correct therapy.
Treatment of the disease
Not everyone knows what increased echogenicity of the pancreas is and what to do in this case. It is necessary to consult a medical specialist. He will prescribe additional studies that will help determine the exact cause of the increased level of echogenicity. Once the cause is known, the doctor draws up a course of treatment. If the cause is lipomatosis, then there is no need for treatment.
In the same situation, when you are diagnosed with acute pancreatitis, this may mean hospitalization. After all, this disease is characterized by severe pain in the abdominal area. Symptoms such as nausea or diarrhea are also common. Quite often, mixed echogenicity of the pancreas is diagnosed, which indicates that the tissue of the organ is heterogeneous.
In what cases does the echogenicity of pancreatic tissue increase?
Increased pancreatic permeability can change normally or when any pathology occurs. Thus, increased echogenicity is a sign of diseases and pathological conditions such as:
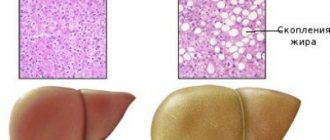
- Lipomatosis is fatty degeneration of organ tissue. Normal pancreatocytes are replaced by adipose tissue cells - adipocytes. As a result of this process, the pancreas becomes denser and gradually ceases to fully perform its inherent functions. Lipomatosis can be observed normally in older people. In young and middle-aged people, degeneration of the pancreas according to the type of lipomatosis is a sign of a serious systemic pathology that requires further examination.
- Fibrosis is the replacement of normal pancreatic tissue with dense connective tissue. On the monitor screen you will see a focus of compaction, uneven contours of the pancreas, and tubercles on its surface. Fibrosis is the outcome of a chronic long-term inflammatory or infectious process, as a result of which the connective tissue grows dead cells, thereby closing the defect in the organ.
- Swelling of the capsule and stroma of the pancreas. This phenomenon is observed in the acute phase of pancreatitis. At the same time, the organ itself swells and becomes denser. At the same time, dyspeptic disorders are observed: vomiting, loose stools, flatulence and bloating.
- Cancerous degeneration of the pancreas. Cancer can grow into an entire organ or part of it. The tumor tissue has a structure different from normal, which is recorded on the monitor as an area of increased echogenicity. Symptoms of weight loss, weakness, and decreased appetite speak in favor of cancer. If cancer is suspected, the patient is referred for additional examination.
- Progressive death of pancreatic cells due to toxic poisoning, pancreatitis. The patient will be in serious condition with symptoms of abdominal pain, hyperthermia, and vomiting.
- Diabetes mellitus type 1 or 2.
Diagnosis of benign pancreatic tumors
Doctors at the Yusupov Hospital make a final diagnosis based on the characteristic clinical picture of some benign tumors and the results of instrumental and histological research methods. A consultation with a gastroenterologist allows you to guess the type of tumor, find out how long ago the symptoms appeared and whether they are progressing.
A biochemical blood test in the case of glucagonoma and insulinoma confirms changes in blood glucose levels. Tumor markers must be determined: carcinoembryonic antigen, CA 19-9. Their level in the case of a benign nature of the disease is not increased.
The most informative methods for diagnosing benign pancreatic tumors in gastroenterology are instrumental studies. Doctors at the Yusupov Hospital perform an ultrasound examination of the abdominal organs to visualize the formation, determine the size of the tumor, and the condition of the regional lymph nodes. Highly informative research methods are magnetic resonance and computed tomography. They can detect small benign pancreatic tumors.
To identify benign pancreatic tumors with multiple foci, scintigraphy is performed at the Yusupov Hospital. Radioactive drugs are introduced into the body, which are actively accumulated by tumor cells. Their radiation is recorded in the image. If a pancreatic hemangioma is suspected, doctors perform angiography to assess the blood flow in the formation and its relationship with the systemic blood flow. In order to study the histological structure of the neoplasm and differentiate it from malignant tumors, surgeons perform a puncture biopsy of the pancreas, followed by a morphological examination of the biomaterial.
Types of echogenicity of structures and tissues
An increase in echogenicity is usually classified according to the time criterion. There is a temporary and permanent increase in the echogenicity of structures.
- Permanent ones are the result of lipomatosis, fibrosis, cancerous degeneration, diabetes mellitus, when irreversible changes have already occurred in the organ. Treatment with medications cannot completely correct the situation; they only alleviate symptoms by replacing the functions of the damaged pancreas.
- Temporary changes are those that are easily amenable to medical treatment and are therefore completely reversible provided that the underlying disease is adequately treated. A temporary increase in echogenicity occurs during acute respiratory viral and bacterial infections, after eating, or when changing your usual lifestyle. In addition, it has been noted that tissue compaction is most often observed in the autumn and spring periods.
Also classified according to the degree of distribution. There are localized and diffuse increases in echogenicity.
A local increase in permeability is determined only in a small area of the organ, while the surrounding tissues are not damaged. The pathological formation is located within a lobe or small lobule. They may be:
- Cystic and pseudocystic areas are rounded cavities located inside the tissue, surrounded by a capsule and not extending beyond. These cavities are filled with cloudy liquid. Cysts and pseudocysts are a complication of acute or chronic pancreatitis.
- Areas of calcification and petrification that arose as a complication of chronic inflammatory processes.
- Areas of lipomatosis - fatty degeneration affecting one of the lobes of the gland.
- Areas of fibrosis - scarring with connective tissue replacement of one or two lobes of the pancreas.
- Duct stones.
- Metastatic screening of a cancerous tumor in one of the lobes of the gland.
A diffuse increase in echogenicity is observed with capsule edema (a sign of acute pancreatitis), lipomatosis and fibrosis, affecting all parts and lobes of the organ. And also in case of cancerous degeneration.
What diseases are possible with increased echogenicity?
Increased echogenicity of the pancreas may indicate the following pathologies:
- lipomatosis (functional gland cells are replaced by fat cells containing little fluid);
- pancreatic necrosis (death of glandular cells);
- diabetes;
- some types of tumors;
- metastases in the pancreas in cancer.
We should not forget that edema characteristic of acute pancreatitis, as well as tumors containing fluid, appear on the ultrasound screen as a decrease in echogenicity.
Principles of treatment
Since increased echogenicity is not a diagnosis, but only a sign of a disease, it does not require treatment in itself. If an ultrasound examination reveals an increase in permeability, the doctor is obliged to send you for additional examination, where the underlying disease will be revealed.
Important! Increased echogenicity cannot be treated on its own. To get rid of organ compaction and relieve its obsessive symptoms, you need to look for and treat the underlying disease.
If the changes are caused by inflammation (pancreatitis), conservative therapy is carried out aimed at eliminating symptoms and transferring the disease into remission. If there is fatty degeneration, it is recommended to reduce body weight and limit fat in the diet. In case of fibrosis, petrification and stones, the issue of surgical treatment through surgery on the pancreas is decided at the consultation, as a result of which the problem of increasing the echogenicity of the pancreatic structures will be solved.
Diagnostics
The initial stage consists of examining the patient and collecting anamnesis.
The standard for diagnosing pancreatic diseases is a combination of ultrasound examination and laboratory tests of blood and urine; an integrated approach allows an accurate diagnosis to be made.
In blood tests, alpha-amylase activity is important. The clearance of amylase is determined in comparison with the clearance of creatinine; with pancreatitis, the ratio of the former to the latter is higher than 5. The amylase content in the urine is examined, an increased indicator indicates pancreatitis.
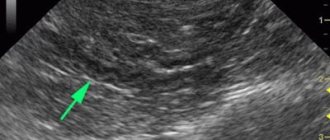
During an ultrasound, a specialist analyzes the structure of the gland, its ducts and vessels. If swelling of the organ and an increase in the diameter of the Wirsung duct are detected, we can talk about acute pancreatitis. Edema gives a picture of reduced echogenicity on the screen, this is due to an increase in fluid content in the organ. The predominant part of tumors is also characterized by low echogenicity.
A diffuse moderate increase in the echogenicity of the pancreas does not lead to a diagnosis; additional studies are required.
The presence of stones, calcifications, scar changes, pseudocysts, and other homogeneity disorders suggests a chronic course of pancreatitis.
With a large accumulation of gas in the intestine, ultrasound waves do not make it possible to clearly and completely visualize the pancreas. This feature imposes nutritional requirements during the period of preparation for ultrasound - it is necessary to exclude foods that increase gas formation.
Interesting video: Increased echogenicity of the pancreas
Diffuse changes in the pancreatic parenchyma
The pancreas is a large organ of internal and external secretion. It is located on the posterior abdominal wall in the retroperitoneal zone, consists of a head, body, tail, and is partially covered in front by the stomach. In the thickness of the pancreas there is a duct directed from the tail to the head. The gland produces pancreatic juice, which contains enzymes that help digest proteins, fats and carbohydrates.
The pancreas tissue contains endocrine glands that produce insulin for the absorption of glucose. A healthy pancreas has homogeneous tissue and large contours. The cause of diffuse changes in the parenchyma of the pancreas, according to doctors, is acute and chronic pancreatitis and elevated blood sugar levels.
Often, diffuse changes in the pancreatic parenchyma are diagnosed in elderly people with various problems of the cardiovascular system, diseases of the liver and biliary tract, and digestive tract organs. The cause of changes in the parenchyma of the pancreas can also be infectious and inflammatory diseases of internal organs that contribute to metabolic disorders.
Increased echogenicity of the pancreatic parenchyma
When performing ultrasound diagnostics, you can find out the density of internal organs. If decreased or increased echogenicity of the pancreas is detected, then this is a serious reason to undergo an extensive examination, providing an accurate diagnosis and determining methods for eliminating problems.
Increased echogenicity of the pancreatic parenchyma is detected during inflammation with the formation of fibrosis, which develops against the background of metabolic disorders, when healthy parenchyma tissue is replaced by fat, during acute pancreatitis and relapse of chronic inflammation that changes the density of the parenchyma.
The absorption coefficient of ultrasonic radiation depends on the increased echogenicity of the parenchyma. Malignant tumors that form in the parenchyma have a higher absorption coefficient of ultrasonic energy than benign tumors.
Consolidation of the pancreatic parenchyma
Methods for studying the parenchyma of the pancreas include questioning and examination of the patient, laboratory, instrumental and radiological methods. Compaction of the parenchyma can be a consequence of various diseases of the pancreas.
Symptoms include pain in the epigastric region and left hypochondrium, disorders of the digestive system that cause a person to feel discomfort, general weakness, and severe weight loss. The appearance of compaction of the parenchyma of an organ has a certain influence on the diet and nature of nutrition, the presence of cholelithiasis, cholecystitis, and cystic fibrosis.
Heterogeneous structure of the pancreatic parenchyma
The pancreas of a healthy person has a homogeneous structure, equal echogenicity, clearly visible contours, an uncinate process, correct position and normal dimensions of the head and tail. Deviation from the norm is determined by an increase in the size of individual parts of the pancreas and the heterogeneity of the structure of its tissues.
Heterogeneity of the pancreas is evidence of the presence of various diseases, including pancreatitis and diabetes mellitus. This pathology can be found in any part of this organ. Diffuse heterogeneous changes can be caused by edema, inflammation and the formation of pseudocysts.
Reactive changes in the pancreatic parenchyma
Reactive changes in the parenchyma are a consequence of inflammation of the pancreas due to the aggressive effect of the liver and gallbladder on it. This causes pain, dyspepsia and increased blood sugar and occurs because the glandular tissue of the parenchyma with a reactive pancreas produces pancreatic juice and hormones in insufficient quantities. One of the most common causes of reactive changes in the parenchyma can be an allergic reaction.
Diffuse changes in an important organ contribute to a reactive change that spreads evenly throughout the pancreas without the presence of local foci indicating neoplasms or stone formation. Treatment of this pathology is one of the pressing issues of modern gastroenterology.
The combination of medications prescribed by the attending physician and properly organized nutrition can prevent the development of various complications. It must be remembered that timely contacting a doctor and carefully following the instructions can be a guarantee of successful treatment.
Expert editor: Mochalov Pavel Alexandrovich | Doctor of Medical Sciences general practitioner
Education: Moscow Medical Institute named after. I. M. Sechenov, specialty - “General Medicine” in 1991, in 1993 “Occupational diseases”, in 1996 “Therapy”.
A person’s complaints of severe pain in the left hypochondrium often indicate inflammation of the pancreas. The examination of the patient begins with an ultrasound of the abdominal organs. A diagnostic method based on measuring the intensity of reflection of sound waves from the surface of organ tissues makes it possible to identify the smallest deviations in the functioning of the digestive system.
Pancreas. Topography of the pancreas. Projection of the pancreas.
Pancreas
located in the retroperitoneal space retroperitoneally, behind the stomach and omental bursa, in the upper half of the abdomen. The bulk of the gland secretes secretion through the excretory ducts into the duodenum; the smaller part of the gland in the form of the so-called islets of Langerhans (insulae pancreaticae [Langerhans]) belongs to endocrine formations and releases insulin into the blood, which regulates blood sugar.
Pancreas
belongs to the upper floor of the peritoneal cavity, since it is functionally and anatomically connected with the duodenum, liver and stomach.
Pancreas
divided into three sections: head, body and tail. The area between the head and the body is also identified - the neck of the gland.
Topography of the pancreas. Projection of the pancreas.
On the anterior abdominal wall the pancreas
is projected in the epigastric, partially in the umbilical and in the left hypochondrium regions. The upper edge of the pancreas is projected onto the anterior abdominal wall along a line running from right to left through the middle of the distance between the xiphoid process and the navel (level of the body of the first lumbar vertebra). In this case, the right part of the line lies slightly below the horizontal, and the left part lies above.
In general, we can say that with respect to the horizontal plane the pancreas
more often it is located obliquely: the head of the gland lies lower, and the body and tail are higher.
What is echogenicity
Echogenicity is a sign system used by uzologists, which allows one to establish the correspondence of the anatomy of organs to the level of reflection and absorption of high-frequency waves. Liquid tissue of the pancreas is characterized by an average echogenicity. The echo density of the liver parenchyma is used as a standard sample.
p, blockquote 5,0,0,0,0 –>
Echogenicity scale for assessing study results
Using ultrasound, you can not only determine the degree to which internal organs perceive high-frequency waves, but also obtain information about other equally important parameters. During the examination of the gland, the following parameters are carefully studied:
p, blockquote 6,0,0,0,0 –>
- Size.
- Form.
- Structure.
- Circuit.
When determining the volume of the pancreas, the length of the head, body and tail is calculated. Ideally, they should not exceed 30, 24 and 25 mm, respectively. An increase in the latter indicates local or general inflammation in the organ. Abnormally large sizes are a typical sign of pancreatitis. Causes of increased size can also be: abdominal trauma, cystic fibrosis, biliary dyskinesia, hepatitis, infectious diseases. Local changes are associated with malignant tumors and cysts.
p, blockquote 7,0,0,0,0 –>
In appearance, the digestive gland resembles a comma and has an oblong shape. Sometimes there is a thickening in the head area. Ring-shaped, additional, split forms are deviations from the norm. Improper development of the organs of the digestive system is associated with disturbances in the processes of embryogenesis.
p, blockquote 8,0,1,0,0 –>
Healthy pancreas. The dark longitudinal stripe is the hypoechoic shadow of the duct.
As for the external contours, they must be clearly defined in the longitudinal and cross sections. Blurring of any part of the gland may indicate the development of an inflammatory process. Blurred outlines and swelling also cause diseases of the organs adjacent to the pancreas (stomach and duodenal ulcers). Uneven borders are created by tumors, cysts, and stones. The contours of malignant formations are lumpy and blurry.
p, blockquote 9,0,0,0,0 –>
The structure of the digestive gland should be homogeneous and fine-grained. Having discovered single fatty inclusions or numerous calcifications and pseudocysts in the organ, the doctor has every reason to suspect fibrolipomatosis and chronic pancreatitis in the patient.
p, blockquote 10,0,0,0,0 –>
Insufficient preparation of the person himself can lead to errors in research results. Three days before the procedure, the patient must adhere to a diet that eliminates the possibility of increased gas formation. For prevention, patients are recommended to take adsorbents. On the day of the procedure, it is advisable to empty your bowels and limit your food intake.
Types of change
When examining the pancreas, its echogenicity is compared with that of a healthy liver; in the normal state, the density of the pancreas is the same as that of the liver, or slightly higher. Changes can have varying degrees and distribution in the body of the gland. A diffuse (encompassing the entire volume of the organ) increase in the echogenicity of the pancreas does not always mean a disease; the presence of local compactions most often indicates pathology.
Echogenicity is displayed on the device screen in the form of a scale of shades of gray; the higher the density of the tissues being examined, the closer the shade is to white.
Slightly
With a slight increase in echogenicity, the ultrasound specialist indicates the presence of changes, but does not make diagnostic conclusions. A slight increase in pancreatic tissue density may be observed in healthy people.
With age, the density of the pancreas increases; the criterion for normality in such cases is the uniformity (homogeneity) of the tissues; if it is preserved, pathology is excluded. Also, in older people, the detection of small hyperechoic inclusions is not considered a pathology.
Moderately
If the homogeneity of the gland is preserved, a diffuse increase in density may not mean disease. To interpret the result, the following are important: the patient’s age, his diet, and the condition of nearby organs. Sometimes such a change is temporary; when nutrition is normalized, a repeated examination may not detect deviations from the norm.
A segmental increase in the density of glandular tissue indicates pathology even with moderate severity of the change.
Much
A significant diffuse increase in the echogenicity of the pancreas indicates degenerative damage to the organ. With a local focal increase in the echo signal, a dangerous disease can also be suspected. Both conditions are most often accompanied by severe clinical manifestations and require therapeutic measures.
What does increased echogenicity mean?
An unusual increase in the recoil force of the waves indicates compaction of the parenchyma and a reduction in the amount of fluid in it. Diffuse hyperechogenicity, the causes of which are external factors, is not considered a pathology. Most often it manifests itself in the hot season, after eating hot and rich food, and during colds.
p, blockquote 12,0,0,0,0 –>
Echogenicity increases markedly with inflammation. Causes for concern may be: tumors, metastases, calcium deposits and stones, cysts, fibrosis. Such inclusions are the consequences of ignoring the early symptoms of pancreatitis.
A number of parameters indicate acute pancreatitis:
p, blockquote 14,0,0,0,0 –>
- General increase in organ size.
- Presence of large echogenic areas.
- Heterogeneity of structure.
- Exceeding the width of the gland duct.
- Blurred boundaries.
A more severe form of the disease involves changes in the density and contours of neighboring organs. Possible formation of pseudocysts.
p, blockquote 15,0,0,0,0 –>
When diagnosing chronic pancreatitis, the following picture is observed:
p, blockquote 16,0,0,0,0 –>
- Echogenicity increases slightly.
- The width of the duct increases by more than 2 mm.
- The size of the gland itself increases.
- Unclear outline.
- Heterogeneous structure.
- There is fluid in the omental bursa behind the stomach.
The disease may be accompanied by the formation of stones. In the picture they appear as spots with an echogenic trace. The progressive disease is easy to notice due to the significant discrepancy in the ratio of the size of the gland to the Wirsung duct. The latter is greatly swollen in width.
p, blockquote 17,1,0,0,0 –>
Parameters such as increased echogenicity and blurred contours suggest that healthy cells in the organ have replaced fat cells, which occurs with lipomatosis. Hyperechogenicity along with a decrease in the pancreas indicate the development of fibrosis. The growth of connective tissue and its replacement of normal cells is accompanied by the appearance of scars.
Cases of increased echogenicity
A slight diffuse increase in the density of the pancreas without the development of its pathology is observed in the following cases:
- eating disorders (overeating);
- a course of taking certain medications;
- stress, lack of sleep, other psycho-emotional overloads;
- alcohol abuse;
- dysfunction of the liver, gall bladder;
- development of colds of the upper respiratory tract.
Often ultrasound signs of such disorders disappear after normalization of nutrition, successful treatment of concomitant diseases and improvement of the general condition of the body.
Local hyperechogenicity requires clarification of the diagnosis.
Heterogeneity of structure
In a healthy person, pancreatic tissue is homogeneous, fine-grained, and homogeneous. The echostructure suspiciously increases in subacute and chronic pancreatitis, cysts and tumors.
p, blockquote 20,0,0,0,0 –>
Acute interstitial pancreatitis is often diagnosed in people who abuse alcoholic beverages and high-fat foods. On palpation they feel sharp pain. Unpleasant symptoms are associated with swelling of the gland. A person complains of cramps in the upper abdomen may contact a doctor.
p, blockquote 21,0,0,0,0 –>
The heterogeneity of the structure is indicated by arrows (white and dark areas).
Severe pain in the left or right hypochondrium occurs with chronic pancreatitis. During periods of exacerbation of the disease, the patient experiences an increase in temperature, abnormal blood pressure, changes in the color of the skin and sclera (jaundice). The patient is worried about constant nausea, vomiting, and lack of appetite. In addition to poor nutrition, the following diseases can affect the development of pancreatitis:
p, blockquote 22,0,0,0,0 –>
- Cholecystolithiasis.
- Ulcer penetration.
- Viral hepatitis.
- Parasites (worms).
- Typhoid and typhus.
- Alcohol abuse.
There are many lovers of alcoholic beverages among men, so the likelihood of chronic pancreatitis in the stronger half of humanity is much higher than in women.
p, blockquote 23,0,0,0,0 –>
Heterogeneity of structure in children
Changes in the homogeneity of the structure of the pancreas often occur in childhood. They manifest themselves as disruptions in the functioning of the gastrointestinal tract. Disturbances occur due to spasms of the gland ducts and increased enzyme activity. The obstructed outflow of the latter causes swelling of the pancreas in the child.
p, blockquote 24,0,0,0,0 –>
This form of the disease occurs even in children 1 year of age. Parents who do not follow the schedule for introducing complementary foods (early inclusion of meat and fish dishes in the menu) can be blamed for this.
p, blockquote 25,0,0,1,0 –>
Symptoms and diagnosis of diseases of the vascular system
The pancreas is an extremely sensitive organ that responds to the most minor abnormalities. Especially when it comes to the pathology of its blood supply.
Medical practice notes that it is quite difficult to diagnose disorders of innervation (supply of tissues with nerve cells) and blood supply to the pancreas, since this pathology is not an independent disease, but is a derivative of a severe clinical picture of the cardiovascular system.
In this case, the diagnosis of the underlying disease becomes primary.
These root causes include:
- atherosclerosis;
- heart failure;
- arterial hypertension as a consequence of atherosclerosis.
The diagnostic conclusion is made taking into account the above reasons, which decisively influence the efficiency of the bloodstream.
These diseases lead to pathological changes in the parenchyma (functionally active cells). As a result, normal pancreatic cells die, and connective tissue takes their place. As a result, fibrosis occurs, i.e., the proliferation of connective tissues and the formation of scars. In this case, it will be unnecessary to talk about the normal functioning of the organ.
Heart failure leads to disruption of the venous blood supply. And, as a consequence, swelling of the pancreatic organ occurs, an increase in its size and dysfunction. Inflammatory processes are activated in the parenchyma, which are diagnosed by an increase in diastase (alpha-amylase enzyme) in the urine and blood.
Nothing surprising or beyond understanding will happen if the reader once again reads the statement that alcohol is the most dangerous of the subjective factors leading to disturbances in the blood supply to the pancreas. Subjective - because only the person himself, by turning on or blocking his volitional trigger, is able to predetermine the further path of events.
Why deviations are dangerous
Negligence towards pancreatitis can increase the risk of new foci of inflammation. The combination of diseases affects the overall health of a person. A critical manifestation of complications is disability.
p, blockquote 26,0,0,0,0 –>
If treatment of the disease is not started at its early stage, pancreatic enzymes enter the blood and create conditions for infection of other organs. Several diseases find a corresponding response:
p, blockquote 27,0,0,0,0 –>
- Liver and kidney failure.
- Bleeding in the stomach and intestines, erosions, ulcers.
- DIC syndrome (blood clotting disorder).
- Purulent-necrotic parapancreatitis.
- Mechanical jaundice.
- Liver hepatosis.
- Cholangitis, cholecystitis.
- Abdominal abscess.
Necrosis of the gland parenchyma develops tumors and cysts. Malignant tumors often appear in older men. Unusual thinness, loss of appetite, abdominal pain are the main symptoms of the disease. Only adequate timely therapy can reduce the chances of such complications occurring.
p, blockquote 28,0,0,0,0 –>
Venous drainage
Venous vessels should not be overlooked when considering the blood supply. The pancreas has a very developed arterial network. The outflow of blood is also carried out by a mass of small vessels, which merge into multiple branches and ultimately flow into the portal vein system.
From the head of the gland, the uncinate process and the duodenum, blood collects through vessels that run parallel to the pancreatic-duodenal arteries. The most functional are the inferior pancreatic-duodenal veins, which are included in the superior mesenteric vein with one, rarely two, trunks. Additionally, blood from the head of the gland and parts of the duodenum is collected in the right gastroepiploic vein.
As for the tail and body of the gland, the outflow of blood in this case is carried out through the pancreatic branches of the splenic vein. Blood is also collected by the great inferior vein, which subsequently drains into the inferior or superior mesenteric vein.
The effect of alcohol on blood flow
If you consume alcoholic beverages in large quantities, it poses a great danger to your health. It is not uncommon for such bad habits to lead to cell death.
The negative effect of drinking alcohol is associated with the work of small blood vessels in the gland. Under the influence of alcohol, the arteries narrow, because of this they cannot tolerate substances that contain useful vitamins to nourish cells. The lack of nutrients leads to cell death.
With long-term consumption of alcoholic beverages, a situation arises when whole pieces of tissue die. Situations are also possible when salt concentration occurs in the tail of the pancreas. Moreover, in women this process occurs much faster than in the opposite sex. Diagnosis of this process, as a rule, occurs in late stages, and therefore the treatment process is quite complicated.
Arterial blood supply
The pancreas does not have its own arterial vessels. The blood supply process comes from the aorta (its abdominal part). The celiac trunk branches off from it, dividing into vessels that supply arterial blood to the pancreas. They form a whole network of small-caliber arteries and arterioles. In total, the following are involved in the bloodstream:
- superior anterior and posterior vessels of the pancreas,
- inferior pancreaticoduodenal artery with anterior and posterior branches,
- inferior pancreatic artery,
- dorsal pancreatic,
- tail artery.
Each of the listed vessels branches into arteries of smaller caliber down to the smallest arterioles and capillaries that take part in the blood supply to each lobule of the pancreas.
Lymphatic drainage is carried out through lymphatic vessels that pass along the blood vessels: lymph flows into the nearby pancreaticoduodenal and pancreatic lymph nodes, then into the celiac and splenic lymph nodes.
Gastric artery
The vessel is located directly behind the section in which the flow of food into the stomach is controlled. In the initial sections they cross the intestine.
The length of the artery ranges from 25 to 40 millimeters, their diameter is 5 millimeters. Pathological changes are often associated with its position in the peritoneum.
Damage to these vessels is associated with abnormal problems in the drainage of the arteries from each other. To get rid of the impending danger, a bypass is performed on the blood artery of the liver, which is located on the right.
Speaking about the role of the pancreatic veins, it is necessary to note their many functions. In particular, thanks to this vein, the course of the artery of the gland is accompanied.
As long as the patient does not need surgical intervention, the anomaly does not have a serious impact on his condition.
There are cases when the liver artery enters the mesenteric artery, which is located in the upper part. Whereas in the correct position it should be part of a branch of the celiac trunk. In this case, serious problems arise in the body.
Important. The pancreatoduodenal arteries produce the outflow of blood, which enters the gland
They provide blood to the liver.
Secretory activity of the organ and nerve impulses
Many people are interested in questions about how the pancreas works. Blood supply and innervation are important issues to consider.
As already mentioned, the activity of the organ is regulated by parasympathetic fibers of the vagus nerve. Nerve impulses received from these nerve endings activate the processes of production and secretion of digestive enzymes.
Sympathetic nerves act differently. Short-term irritation of the splanchnic nerve stops the secretion of pancreatic juice. However, prolonged stimulation is also accompanied by intense enzyme release.
It is worth noting that even if the nerves described above are damaged, pancreatic secretion does not stop, as it is supported by humoral regulatory mechanisms.