About hiatal hernia and reflux esophagitis
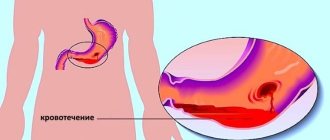
Hiatal hernia (HH) and reflux esophagitis is a disease of the esophagus and ligamentous apparatus of the diaphragm, in which an enlargement of the esophageal opening of the diaphragm occurs and the ligaments that fix the esophagus and stomach are stretched. As a result of stretching, the upper part of the stomach extends into the chest cavity and the functioning of the lower esophageal sphincter is disrupted.
A change in the angle of His and disruption of the lower esophageal sphincter leads to the reflux of acidic gastric contents or bile from the duodenum into the esophagus with the development of inflammation and restructuring of the mucous membrane, up to the occurrence of esophageal cancer. According to the European and American Gastroenterological Associations, if a hiatal hernia persists for 5–12 years without treatment, the risk of developing esophageal cancer increases by 270% after 5 years and by 350–490%, depending on age, after 12 years.
Reflux esophagitis is an inflammatory process in the esophagus that occurs as a result of the reflux of gastric or intestinal contents into the esophagus and its impact on the mucous membrane of the esophagus.
A hiatal hernia is usually combined with GERD. Gastroesophageal reflux disease is characterized by a complex of dyspeptic, pulmonary and cardiac disorders, usually arising as a result of hiatal hernia and pathological gastroesophageal reflux.
Why does a hiatal hernia occur?
The disease can be congenital or acquired. The reasons that provoke it are very diverse.
All three forms of pathology arise under the influence of the same factors. Congenital include hernias and hernial pockets that form during the period of intrauterine development, and also the provoking factor is underdevelopment of the diaphragm.
Purchased items include:
- chest injuries;
- inflammatory processes in this area; age-related changes;
- increased intra-abdominal pressure.
Often the disease occurs due to a combination of several causes, for example, when the organs of the peritoneum come out through the natural opening of the diaphragm (congenital defect) during a coughing attack in a smoker (acquired causative factor).
Classification of hiatal hernias
There are three main types of hiatal hernia.
- Sliding (axial) hernia.
Occurs in almost 90% of patients. In this case, the cardia lies above the esophageal opening of the diaphragm, and therefore the relationship between the esophagus and the stomach changes, and the closure function of the cardia is sharply disrupted. - Paraesophageal hernia.
Occurs in approximately 5% of patients. It is characterized by the fact that the cardia does not change its position, and the fundus and greater curvature of the stomach emerge through the enlarged opening. - Short esophagus.
As an independent disease, it is rare and represents a developmental anomaly. Usually occurs in combination with a sliding hernia and is a consequence of spasm, inflammatory changes and scar processes in the wall of the esophagus.
Classification of reflux esophagitis
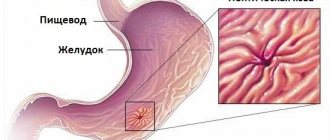
Rice. 1. Normal position of the stomach and angle of His (diagram).
Rice. 2. Moving part of the stomach into the chest cavity and changing the angle of His in case of hiatal hernia (diagram).
To unify and evaluate gastroscopic examination data, the Savary-Miller classification of the severity of esophagitis is used, distinguishing four stages of the disease:
- Stage I - round and longitudinal lesions that do not merge and spread from the Z-line to the mucous membrane of the esophagus;
- Stage II - merging transient lesions in the Z-line area, not covering the entire surface of the mucous membrane;
- Stage III - ulcerative lesions that coalesce in the lower part of the esophagus and cover the entire surface of the mucous membrane;
- Stage IV - chronic ulcerative lesions of the esophagus, fibrous stenosis, shortening of the esophagus (Barrett's esophagus).
causes
The diaphragm is the muscle that separates the lungs from the abdominal cavity; When you take a deep breath, the diaphragm, which is dome-shaped when relaxed, contracts and flattens. Through this movement, it allows air to enter the lungs.
On the left side of the diaphragm there is a small opening through which the esophagus, the tube that carries food and liquids to the stomach, passes. Under normal conditions, this opening ( hiatus ) is really small and fits perfectly into the esophagus.
The stomach, when all is well, is completely below the diaphragm.
Obesity: In some people, the hiatus (the hole in the diaphragm) weakens and widens, often for no apparent reason. It could be a hereditary disease, or even
- excessive force during exercise (such as heavy lifting) or straining during bowel movements,
- lesions of an anatomical cause,
- especially long break from birth (congenital).
Regardless of the cause, a hernia occurs: part of the stomach goes up into the chest cavity because the opening has expanded. This situation is called a hernial hernia.
Hiatal hernias are very common over 50 years of age.
There are mainly 3 types of hernia known:
- Hiatal sliding hernia: This is the most common type, the hernia runs up and down, entering and exiting the chest cavity. These hernias are usually small and usually do not cause problems or symptoms.
- Fixed hiatal hernia (or paraesophageal): In this case, the upper part of the stomach remains compressed into the chest. Even in this situation, symptoms may be minor. However, problems with the esophagus are more likely to occur.
- Complex or mixed hiatal hernia: Fortunately, this type of hernia is rare. A hernia can take many forms, even in situations where the entire stomach forms a hernia in the chest. It is very likely that this type of hernia is causing problems and that treatment, which often includes surgery, is necessary. However, complex hernias are very rare.
In more specialized contexts, a fourth form of hernia is also included in this classification, which simultaneously includes hernias of other internal organs such as the colon and spleen.
Hiatal sliding hernia
This is the most common form, occurring in more than nine out of ten patients; the name refers to the discovery of a more or less large portion of the stomach that slips through the hiatus, the opening in the diaphragmatic muscle through which the esophagus passes. It is often associated with the condition of obesity.
This is the cause of the most common symptom, reflux (increased acid from the stomach into the mouth).
Slipping is sometimes a dynamic, reversible condition and is particularly sensitive to changes in abdominal pressure (swallowing, straining, coughing, ... these can contribute to the release of the hernia, which can subsequently restore the original position).
Risk factors
- Age 50 or older,
- obesity,
- pregnancy.
This disorder is more common in women than men, probably due to intra-abdominal forces that occur during pregnancy.
Symptoms, signs and clinical picture of hiatal hernia and reflux esophagitis
The most common symptoms are heartburn, often persistent, painful, occurring both after meals and on an empty stomach, especially when bending over and in a lying position, as well as belching of sour, bitter air or regurgitation of food. A characteristic symptom of a hiatal hernia is pain, usually of a burning nature, which occurs in the epigastric region, behind the sternum, in the left hypochondrium, and intensifies with physical activity and bending over. There is often a feeling of a lump in the throat and pain when swallowing food. In this situation, a person feels discomfort behind the sternum, up to severe bursting pain spreading to the left shoulder and shoulder blade (just like with angina), burning, a feeling of lack of air or dissatisfaction with inhalation. Some patients often experience a sudden increase in blood pressure for no apparent reason. At night there is increased salivation, attacks of coughing and choking, and by morning hoarseness appears.
Diagnostic methods
Diagnosis is based on the clinical picture described above and instrumental examination methods. Instrumental examination methods used to diagnose hiatal hernia and endothelial hernia include:
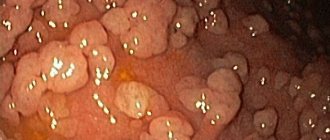
- fibrogastroscopy - during which the condition of the mucous membrane of the esophagus, stomach and duodenum is assessed, and prolapse of the gastric mucosa into the esophagus is detected,
- X-ray examination of the esophagus and stomach, during which the hiatal hernia itself is revealed, its size, fixation, and the motility of the esophagus and stomach and the presence of reflux of barium suspension into the esophagus are assessed,
- The third study, which helps the surgeon in determining the indications for surgery and choosing the method of surgical correction, is daily pH-metry of the esophagus and stomach, during which the level of gastric secretion and the presence of pathological refluxes from the stomach into the esophagus are determined. The most important criterion for the presence and severity of reflux esophagitis is the total time at which the pH is less than 4 units. Increased number of refluxes lasting more than 5 minutes. and an increase in the duration of the most prolonged reflux indicates a decrease in esophageal clearance and suggests the presence of hypomotor dyskinesia of the esophagus.
To identify the hiatal hernia and determine the extent of damage to the esophagus, as well as select the correct surgical treatment tactics, you must send me a complete description of gastroscopy, x-ray of the esophagus and stomach with barium for the hiatus, preferably an ultrasound of the abdominal organs, indicating your age and main complaints. In rare cases, if there is a discrepancy between complaints, X-ray data and FGS, it is necessary to perform daily pH measurements and manometry of the esophagus. Then I will be able to give a more accurate answer to your situation.
Diagnostics
Questioning and examination of patients allows the doctor to suspect a hiatal hernia, but an X-ray examination is required to confirm the diagnosis. Additionally, EFGS (esophagogastroscopy) may be recommended to clarify the condition of the mucous membranes of the esophagus and stomach. If a hiatal hernia is accompanied by chest pain, an ECG is required to rule out heart problems.
For all types of hiatal hernia (axial others), the diagnostic methods are the same.
Treatment of hiatal hernia
Puchkov K.V., Filimonov V.B. Hiatal hernia: monograph. - M.: MEDPRACTIKA - M., 2003. - 172 p.
Treatment of hiatal hernia is 99% consistent with the treatment of its complications - reflux esophagitis and, unfortunately, the therapeutic treatment of hiatal hernia is purely symptomatic: as long as the patient takes medications, limits himself in diet, and strictly follows all the doctor’s instructions and prescriptions, his condition is relatively satisfactory. As soon as the course of treatment is stopped, all the symptoms of hiatal hernia (constant belching, painful heartburn) return. Patients with small, unfixed hiatal hernias without a pronounced clinical picture and only if the patient is ready to take medications for life that prevent the occurrence of reflux esophagitis or reduce the symptoms of the disease are subject to conservative (therapeutic) treatment by a gastroenterologist. But it is worth noting that with the systematic use of drugs that reduce the acidity of gastric juice, for example, omeza, quamatel, ranetidine and others, after 5 years the risk of developing stomach cancer increases by 350%, and after 12 years it increases by 560% compared with persons without hiatus of the same age. At the same time, the lack of acid in the stomach prevents the normal digestion of food, as a result of which its remains enter the large intestine, causing putrefactive processes and the development of severe intestinal dysbiosis.
Folk remedies and methods of treating traditional medicine for hiatal hernia
I would like to especially note the folk remedies and methods of traditional medicine used in the treatment of hiatal hernia. Folk or pseudo-folk remedies and methods for the treatment of hiatal hernia recommended by various herbalists, collections of advice for patients and other popular literature lead to a temporary improvement in the patient’s condition and relief from the symptoms of reflux esophagitis, which is perceived by patients as a cure. All folk remedies for the treatment of hiatal hernia are comparable in their mechanism of action to medications - they either reduce the acidity of gastric juice or change the acidity (neutralize) the gastric juice itself. But as a rule, the effectiveness of folk remedies for hiatal hernia is 50–70% lower compared to medications.
Rice. 3. Hiatal hernia before surgery (diagram).
Reasons for development
According to statistics, hiatal hernia is common among people over 55 years of age. This is explained by age-related overstretching or weakening of the ligamentous-articular apparatus. Moreover, asthenics (i.e. physiologically underdeveloped people) are predisposed to this disease.
The movement of organs into the mediastinum can cause disruption of the human heart and lungs. There are a number of factors leading to the manifestation of a characteristic disease:
1) Disorders of contractions of the intestines and other organs of the gastrointestinal tract (perilstatics). The disease can manifest itself chronically due to the following “provocateurs”:
- stomach and duodenal ulcers;
- inflammation of the pancreas (pancreatitis);
- inflammation of the gastric lining and duodenum;
- chronic cholecystitis.
2) There are prerequisites that a hiatus hernia may occur as a result of abnormal development of the body during gestation. Consequently, a person with defects of the thoracic stomach, short esophagus and other similar anatomical features may be susceptible to this disease;
3) Due to the fact that the hernia is associated with the diaphragm, its development can be provoked by all kinds of defects in the organ:
- development of muscle weakness;
- enlargement of the hernial orifice;
- stretching of the diaphragmatic opening.
4) Increased pressure within the abdominal space can also cause a hiatal hernia. This can be facilitated by:
- tumors or neoplasia in the abdominal cavity;
- flatulence (increased gas formation in the intestines);
- prolonged and severe cough with sputum, as well as related diseases;
- closed or open abdominal injuries;
- pregnancy;
- severe and frequent vomiting;
- dysbacteriosis, diarrhea;
- diseases of the respiratory system.
5) It is possible that lifestyle can also influence the development of a hiatal hernia. It has been proven that people with an asthenic physique who often lift weights often become victims of this disease.
In addition, there is a theory (not yet proven) about the indirect effect of alcohol and nicotine on the development of this disease. Do not forget about nutrition during a hiatal hernia, since overeating and gluttony are also its “allies.” One of the features of the human digestive system is its inability to process large quantities of food. The stomach chamber cannot quickly transfer food to the intestines, which leads to overcrowding and unwanted pressure on the diaphragm.
Surgical methods for treating hiatal hernia (hiatal hernia)
If there is no effect from drug therapy for hiatal hernia, surgical treatment is indicated, the essence of which is to restore normal anatomical relationships in the area of the esophagus and stomach.
Indications for surgical treatment of hiatal hernia:
- ineffectiveness of conservative treatment;
- the presence of complications of the hiatal hernia (esophagitis, erosions and ulcers of the esophagus, anemia, bleeding);
- large size of the hernia, its fixation in the hernial orifice;
- paraesophageal (near esophageal) sliding hernia (high risk of strangulation of the hernia);
- dysplasia of the esophageal mucosa (the esophageal mucosa acquires the structure of the small intestinal mucosa).
Types of surgical treatment for hiatal hernia: all currently existing surgical methods for treating hiatal hernia are aimed at eliminating the hernia (suturing the hiatal hernia to a normal size of 4 cm by crurorrhaphy) and surgically creating an areflux mechanism that prevents the reflux of gastric contents into the esophagus. Most domestic clinics use Nissen fundoplication operations, which consists of surgically turning the fundus of the stomach around the esophagus 360 degrees, which makes it possible to create a cuff that prevents the reflux of gastric contents into the esophagus and, consequently, the development of esophagitis.
Rice. 4. Final view of the surgical field after crurorrhaphy and physiological fundoplication according to Tope (270 degrees)
Rice. 5. Places of punctures of the abdominal wall during laparoscopic surgery to eliminate the hiatal hernia
The Nissen fundoplication operation can be performed using an open or laparoscopic approach, but at the same time it is not without significant drawbacks. First, classical fundoplasty in patients with a fixed, long-standing hiatal hernia can lead to a significant deterioration in the patient’s quality of life. As a result of this type of fundoplication, an absolute valve is formed in the cardia area, and the patient completely loses the ability to use such a natural protective mechanism of the stomach as regurgitation or vomiting. When taking any carbonated drinks, from champagne to sparkling water, the liquid gases cannot leave the stomach through the cardia and swell it. A feeling of heaviness and pain in the stomach also occurs when eating a large amount of food. Secondly, classical fundoplasty does not provide for fixation of the formed cuff, which after some time leads to the cuff slipping and relapse of the disease. After Nissen fundoplasty, relapse of the disease occurs only 1–2 years after the operation.
Therefore, most European surgeons use partial Toupe fundoplication at 270 degrees in their practical work
, which allows patients to guarantee the physiological functioning of the sphincter in the postoperative period, as well as to preserve natural protective mechanisms - belching and the gag reflex, the importance of which for maintaining the quality of life of patients was discussed above.
Watch a video of operations performed by Professor K.V. Puchkov. You can visit the website “Video of operations of the best surgeons in the world.”
Since the early 90s, laparoscopic access has been used to correct hiatal hernia, which allows the surgeon to perform any type of fundoplication and reliably suture the hernia defect in the diaphragm. The formation of a physiological fundoplication according to Tope requires the surgeon to master the endoscopic suture, therefore, before performing such operations, one should undergo long-term training on special simulators.
It is worth noting that hiatal hernia is often combined with cholelithiasis and duodenal ulcer, which also require surgical treatment. In this situation, laparoscopic access seems ideal and allows simultaneous (combined) operations to be performed on different organs of the abdominal cavity, for example, on the gallbladder, on the sphincter of the papilla of Vater, and on the diaphragm and stomach itself. With appropriate qualifications of the surgeon, the duration of the operation increases by only 30–40 minutes, and the number of complications remains low. When performing a simultaneous operation using laparoscopic access through punctures for the hiatal hernia, cholecystectomy (chronic calculous cholecystitis) and selective proximal vagotomy (chronic duodenal ulcer) are simultaneously performed.
After laparoscopic surgery for the correction of a hiatal hernia, 3–4 incisions of 5–10 mm in length remain on the skin of the abdomen. From the first day, patients begin to get out of bed, drink, and the next day take liquid warm food. Discharge from the hospital is carried out on days 1–3, depending on the severity of the disease. The patient can begin work in 2–3 weeks. A strict diet should be followed for one and a half to two months, a softer one - for six months. Further, as a rule, the patient leads a normal lifestyle - without medications or diet. Laparoscopic surgery for hiatal hernia is the best way to instantly correct the existing problem and restore quality of life to patients.
Postoperative period
For several days, swelling usually persists in the area of the surgical field, which can somewhat narrow the lumen of the esophagus and impede the passage of food. Therefore, discomfort may be felt when swallowing for several days (sometimes up to 2 weeks). Often after surgery, a nasogastric tube is left in the lumen of the esophagus for 1-2 days, through which the patient is fed liquid food.
The first day it is recommended to drink only water (up to 300 ml). The remaining fluid is administered by infusion of saline solutions into a vein.- On the second day, you are allowed to eat a small portion of liquid food (low-calorie soup).
- Gradually, portions are increased, soft foods are added that easily move through the esophagus.
- Gradually over 2 months the patient returns to a normal diet.
- All drinks and food taken in the postoperative period should be warm (comparable to body temperature) so as not to cause additional swelling.
In the postoperative period, antibiotics, painkillers are prescribed, and if gastrointestinal motility is impaired, prokinetics (cerucal, motilium) are prescribed. The sutures are removed on the 7th day, after which the patient is discharged from the hospital under the supervision of a gastroenterologist.
It is very important after surgery to exclude factors that may contribute to relapse of the disease, namely:
- Avoid heavy physical activity.
- Don't overeat.
- Eat right to avoid flatulence and constipation.
- If necessary, treat diseases of other gastrointestinal organs to normalize gastric and intestinal motility.
- Avoid tight, tight belts.
- Adequately treat bronchopulmonary diseases to reduce chronic cough.
Possible complications after surgery:
- Bleeding.
- Perforation of the stomach or esophagus.
- Pneumothorax.
- Inflammation with the development of peritonitis or mediastinitis.
- Obstruction of the esophagus.
- Relapse of the disease.
If indicated, surgery to remove a hiatal hernia can be performed free of charge in a public clinic. In paid clinics, the cost of such an operation ranges from 60 to 150 thousand rubles.