What is echogenicity called and how is it detected on ultrasound?
The concept of echogenicity refers to the ability of tissues and internal organs to reflect ultrasonic impulses and waves. A reduced level of ultrasound reflection ability is called hypoechogenicity, and an increased level is called hyperechogenicity.
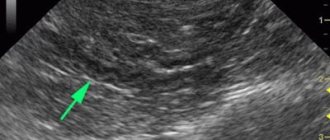
On the monitor screen of an ultrasound machine, this indicator is visualized in the form of a gray scale, which, depending on the state of performance of the organ under study, changes its shade level.
For example, a hypoechoic formation in the pancreas is visualized as one dark gray spot or a black spot. But the average level of this indicator is visualized as a light gray shade of the pancreas with distinct, even contours. An increase in echogenicity, or hyperechogenicity, appears as a lighter area, up to white shades.
It is important to remember that the norm of the pancreas echogenicity indicator corresponds to the level of this indicator of a healthy liver. Any decrease or increase in echogenicity is also always compared with liver parameters.
When echogenicity becomes reduced
Situations where the echogenicity of the pancreas is reduced during ultrasound examination can be observed in cases of diffuse and/or a number of focal changes. In complex sonography of the gastrointestinal tract, the ability to reflect ultrasound by pancreatic tissues is determined in comparison with the liver and gallbladder structures. The pancreas (PG) is not examined separately to determine this indicator.
A decrease in signal registration on a monitor or sonogram, visually perceived as darkening, is indicated by a decrease in echogenicity.
Diffuse (widespread) changes affect the entire gland. The darkening is visible evenly. In the structure of the pancreas, areas of normal reflected signal may appear that are related to the organ and are not pathological.
Items with increased echo response should be considered violations. The contours of the gland with widespread hypoechogenicity will be either clear or barely distinguishable against the background of surrounding structures.
Hypoechoic pancreas
Focal areas of reduced echogenicity are visible as darkening or almost black formations. The number varies. Their contours are visualized clearly or may be blurry and heterogeneous. The background of the underlying pancreatic tissue is also variable: decreased, normal or increased echo response.
Functional and, especially, anatomical changes in the gland that can reduce the intensity of reflected ultrasound are based on the development of edema or replacement of normal tissue.
Causes of pathological changes in the level of echogenicity
The development of the following pathological processes can reduce or increase the level of the ability of the pancreas to reflect ultrasound:
- the formation of calcifications, or as they are also called small pebbles in the pancreas;
- development of pancreatic pathology (inflammatory process) of an acute or chronic nature;
- development of tumor-like neoplasms;
- the progressive stage of lipomatosis, that is, the replacement of healthy glandular tissues with fatty tissues;
- necrotic lesion of the parenchyma.
The development of each of the above pathological processes is clearly visible on the monitor screen of the diagnostic apparatus.
Types of hypoechoic formations
Detection of a hypoechoic structure of the pancreas during an ultrasound examination may indicate the development of an acute form of pancreatic damage to this organ. Moreover, the acute form of pancreatitis is accompanied by a loss of clarity of the contours of the gland, which prevents a full examination of the parenchymal organ. Over time, as this pathology progresses, the contour lines of the gland become more and more blurred, until it is completely impossible to visualize them.
In some cases, it is possible to identify individual hypoechoic areas against the background of multiple hyperechogenicity. Such processes can occur when, after intense fibrolipomatous processes in the gland, destructive disorders with an inflammatory nature begin to develop.
The progressive stage of acute pancreatitis contributes to a significant increase in the size of the parenchymal organ, and also acts as an acute factor that reduces echogenicity.
In some cases, echogenicity may be reduced to such an extent that the pancreas is almost impossible to distinguish from the splenic and portal veins.
Zones of hypoechoic formations are also detected during the development of hemorrhagic pancreatitis. Hemorrhagic pancreatitis can not only reduce the level of echogenicity of the organ under study, but also increase it to a significant size and cause an edematous state of the soft tissues adjacent to this organ.
A decrease in the level of pancreatic density can be either diffuse or focal. With a diffuse decrease in the ability to reflect ultrasound, edema occurs when the level of fluid content in the gland increases. This mainly happens with the development of acute pancreatitis, or the manifestation of a severe allergic reaction with existing hypervolemia, that is, an increased level of water content in the body.
The formation of focal hypoechogenicity may be preceded by the following pathological changes:
- cystic lesion of the parenchyma;
- development of a pancreatic cyst;
- the appearance of a tumor-like neoplasm;
- an increase in the diameter of the ducts of the gland being studied.
It is important to remember that the focal type of the gland’s ability to reflect ultrasound can be not only reduced, but also increased, depending on what type of tumor-like neoplasm occurs.
Treatment methods
Therapeutic methods of treatment for any type of pathological deviation of the echo structure of the gland from the norm are developed taking into account the results of additional diagnostic methods, such as laboratory testing of feces, urine and blood, as well as based on the diagnosis. Most often, medications are prescribed, which are based on synthetic or natural enzymes that help reduce the overall level of load on the affected organ, or, for a certain period of time, perform its functions in the absorption of nutritional components from food taken.
Antispasmodic drugs will help reduce pain and eliminate the feeling of unpleasant discomfort.
As a complement to the main treatment, a strict dietary diet is prescribed. Exceptions should be made to the following ingredients:
- alcohol-containing and carbonated drinks;
- fatty foods;
- semi-smoked and smoked food products;
- fried and heavy foods.
On the first day of treatment, it is recommended to take only alkaline water, and then subsequently, with an improvement in overall health, you can add vegetables and boiled lean meat to the diet.
It is worth remembering that the speed of the recovery process of the affected organ completely depends on the strict adherence to the dietary regimen, because basically all pathological disorders in the pancreas occur against the background of poor nutrition and consumption of excessive levels of fast carbohydrates and fast food.
Patients often wonder if the echogenicity of the pancreas is increased, what is it and how to treat such a deviation?
This formulation may be unexpected for a person who is undergoing a routine medical examination or undergoing an ultrasound scan for any indication.
Don’t panic, because increased echogenicity of an organ is not a diagnosis.
Diffuse decrease in echogenicity
Violation of the texture of the entire organ, accompanied by changes in structure and size. Often, with a widespread process in the pancreas, the structure of its ducts changes. The following signs are recorded during inflammation:
- acute pancreatitis - the structure is unclear, the contours are uneven, the dimensions are enlarged, small areas of complete absence of an echo signal can be detected (hemorrhages, necrosis);
- chronic pancreatitis (early stage) - the structure is relatively clear, the contours are uneven, the dimensions are normal or slightly larger.
During the development and course of inflammation, edema is considered as the main factor that reduces the echogenicity of glandular tissue. An increase in the content of interstitial fluid leads to a weakening of the reflection of ultrasound.
What does the term “echogenicity” mean?
Echogenicity is not a diagnosis. This is the term used to describe an ultrasound examination of the abdominal organs.
If the doctor indicates it in the description, this means that the tissues of the organ to which the ultrasound is directed reflect it. The ultrasound reflected by the organ is picked up by a sensor that emits waves.
On the monitor, the specialist sees a picture that is formed based on the difference between the directed and reflected waves.
Each organ is characterized by its own level of echogenicity. During the study, the signal may be homogeneous or heterogeneous.
Useful article? Share the link
During an ultrasound, organs with a denser structure are displayed on the screen in light gray. It is worth noting that the liquid is not capable of reflecting rays, it transmits them.
This feature is called “echonegativity”, and formations such as cysts or hemorrhages are called anechoic.
Why is the rate increasing?
Echogenicity can increase as a result of various reasons. Local increase indicates the presence of compactions. This is how tumors, metastases, the presence of stones or salt deposits are determined.
The reasons for increased echogenicity of the pancreatic parenchyma may be:
- The patient suffers from lipomatosis of the gland. This disease is characterized by the replacement of glandular tissue with fat cells, while the size of the organ itself does not change;
- the patient has swelling of the organ, which can develop with pancreatitis;
- A pancreatic tumor has been diagnosed, and the patient experiences a number of symptoms: the patient is losing weight, the skin is pale, there is no appetite, bowel movements are disturbed;
- the patient suffers from pancreatic necrosis - this means that the cells of the organ die. During an ultrasound, the area with dead cells will appear as a bright area on the monitor;
- Diabetes mellitus can provoke pathology. With this disease, the patient feels constant thirst, body temperature rises, urination becomes quite frequent, especially at night;
- The patient develops fibrosis. This disease is characterized by abnormal bowel movements, the appearance of pain in the abdominal cavity, and the color of the organ on the monitor differs from the color of the liver.
Increased echogenicity may occur diffusely and temporarily:
- the patient has reactive inflammation, for example, with influenza, pneumonia, and other diseases;
- the patient has suddenly changed his diet or lifestyle;
- diffusely, the indicator may increase in certain seasons;
- the patient ate a large amount of food.
With a temporary disruption of the pancreas, the increase in echogenicity occurs moderately.
When the echogenicity of the entire gland increases
A diffuse change in the permeability of pancreatic tissue to ultrasound can be a symptom of pathology, but can also be observed normally. This cannot be said about foci with increased echogenicity - this is almost always a pathology.
The gland has normal dimensions, but its echogenicity is increased (this can be seen in the two-dimensional graph that displays the density of the liver)
The echogenicity of the pancreatic parenchyma is increased in the following pathologies:
- Glandular lipomatosis, when glandular tissue is replaced by fat cells containing almost no intracellular fluid; however, they are not enlarged. This condition is most often asymptomatic. Read more about this disease in the article:
- Swelling of the gland that develops with acute pancreatitis. Accompanied by abdominal pain, diarrhea, vomiting.
- Organ tumor. If the ultrasound describes the pancreas with increased echogenicity, then there are necessarily symptoms of the disease: weight loss, pallor, weakness, lack of appetite, frequent bowel movements.
- , accompanied by the death of organ cells, will also appear on ultrasound as a lighter area. This disease has such signs as severe abdominal pain (up to the development of painful shock), disturbance of the general condition, uncontrollable vomiting, and diarrhea.
- As a result of diabetes mellitus, which is manifested by thirst in the absence of hot conditions, elevated temperature, active work, as well as frequent and abundant (including night) urination.
- Development of connective tissue in the gland () - usually as a result of previous inflammation or metabolic disorders. In this case, a person may remember cases of unstable stool and abdominal pain. Ultrasound shows not only an increase in echogenicity, but also a decrease in the size of the gland and the tuberosity of its contours.
The hyperechoic pancreas can also be a temporary phenomenon, manifested by:
- as a result of reactive inflammation in many infectious diseases: influenza, pneumonia, meningococcal infection. This requires treatment of the underlying disease;
- when changing the type of food consumed;
- after a lifestyle change;
- at certain times of the year (usually spring and autumn);
- after a recent heavy meal.
In such temporary conditions, the echogenicity of the pancreas is moderately increased, in contrast to pathologies, when significant hyperechogenicity is noted.
Local increase in echogenicity
Fatty inclusions in the pancreatic tissue will appear hyperechoic
What are hyperechoic inclusions in the pancreas? It can be:
- pseudocysts - liquid formations that develop as a result of acute pancreatitis; with this disease, the contour of the pancreas becomes uneven, jagged, hyperechoic;
- calcification of tissue areas - calcifications; they are also formed as a result of inflammation (usually chronic);
- areas of adipose tissue; they replace normal gland cells in case of obesity and excessive consumption of fatty foods;
- fibrous areas - where areas of normal cells have been replaced by scar tissue; usually this occurs as a result of pancreatic necrosis;
- stones in the gland ducts;
- fibrocystic degeneration of the gland is either an independent disease or an outcome of chronic pancreatitis;
- metastatic tumors.
Signs of increased echogenicity of the organ
In acute pancreatitis, there is an increase in pressure in the pancreatic ducts, and the structure of the organ becomes heterogeneous.
As a result, the organ can be injured, and enzymes that help digest food can get into nearby tissues.
In this way, digestion of organ tissues and intoxication of the body can occur.
With increased echogenicity of the pancreas, the following signs may be observed:
- the patient develops nausea and vomits;
- blood pressure drops;
- heart rate increases;
- in the left hypochondrium the patient feels severe pain.
In chronic pancreatitis, increased echogenicity of the parenchyma causes swelling of the organ and the formation of hemorrhages.
Digestive enzymes are not produced in the required quantities. The patient feels a decrease in appetite, disruptions in bowel movements, and a feeling of a full stomach in the absence of food.
On the monitor during an ultrasound, the structure of the organ is heterogeneous.
If malfunctions in the pancreas began not so long ago, then during an ultrasound examination the echogenicity of the organ parenchyma will be normal.
Only after some time will the clinical manifestations intensify, pain in the abdominal region will appear, and a heterogeneous structure of the pancreas will appear during ultrasound.
If the pancreas is not functioning properly, the patient may develop diabetes mellitus. In older people suffering from this disease, lipomatosis is diagnosed.
With this disease, glandular tissues are replaced by fat cells. It is worth noting that with age, organ cells lose fluid.
Changes in the parenchyma of the pancreas
The article was prepared by a specialist for informational purposes only. We urge you not to self-medicate. When the first symptoms appear, consult a doctor.
Diffuse changes in the pancreatic parenchyma
The pancreas is a large organ of internal and external secretion. It is located on the posterior abdominal wall in the retroperitoneal zone, consists of a head, body, tail, and is partially covered in front by the stomach. In the thickness of the pancreas there is a duct directed from the tail to the head. The gland produces pancreatic juice, which contains enzymes that help digest proteins, fats and carbohydrates.
The pancreas tissue contains endocrine glands that produce insulin for the absorption of glucose. A healthy pancreas has homogeneous tissue and large contours. The cause of diffuse changes in the parenchyma of the pancreas, according to doctors, is acute and chronic pancreatitis and elevated blood sugar levels.
Often, diffuse changes in the pancreatic parenchyma are diagnosed in elderly people with various problems of the cardiovascular system, diseases of the liver and biliary tract, and digestive tract organs. The cause of changes in the parenchyma of the pancreas can also be infectious and inflammatory diseases of internal organs that contribute to metabolic disorders.
Increased echogenicity of the pancreatic parenchyma
When performing ultrasound diagnostics, you can find out the density of internal organs. If decreased or increased echogenicity of the pancreas is detected, then this is a serious reason to undergo an extensive examination, providing an accurate diagnosis and determining methods for eliminating problems.
Increased echogenicity of the pancreatic parenchyma is detected during inflammation with the formation of fibrosis, which develops against the background of metabolic disorders, when healthy parenchyma tissue is replaced by fat, during acute pancreatitis and relapse of chronic inflammation that changes the density of the parenchyma.
The absorption coefficient of ultrasonic radiation depends on the increased echogenicity of the parenchyma. Malignant tumors that form in the parenchyma have a higher absorption coefficient of ultrasonic energy than benign tumors.
Consolidation of the pancreatic parenchyma
Methods for studying the parenchyma of the pancreas include questioning and examination of the patient, laboratory, instrumental and radiological methods. Compaction of the parenchyma can be a consequence of various diseases of the pancreas.
Symptoms include pain in the epigastric region and left hypochondrium, disorders of the digestive system that cause a person to feel discomfort, general weakness, and severe weight loss. The appearance of compaction of the parenchyma of an organ has a certain influence on the diet and nature of nutrition, the presence of cholelithiasis, cholecystitis, and cystic fibrosis.
Heterogeneous structure of the pancreatic parenchyma
The pancreas of a healthy person has a homogeneous structure, equal echogenicity, clearly visible contours, an uncinate process, correct position and normal dimensions of the head and tail. Deviation from the norm is determined by an increase in the size of individual parts of the pancreas and the heterogeneity of the structure of its tissues.
Heterogeneity of the pancreas is evidence of the presence of various diseases, including pancreatitis and diabetes mellitus. This pathology can be found in any part of this organ. Diffuse heterogeneous changes can be caused by edema, inflammation and the formation of pseudocysts.
Reactive changes in the pancreatic parenchyma
Reactive changes in the parenchyma are a consequence of inflammation of the pancreas due to the aggressive effect of the liver and gallbladder on it. This causes pain, dyspepsia and increased blood sugar and occurs because the glandular tissue of the parenchyma with a reactive pancreas produces pancreatic juice and hormones in insufficient quantities. One of the most common causes of reactive changes in the parenchyma can be an allergic reaction.
Diffuse changes in an important organ contribute to a reactive change that spreads evenly throughout the pancreas without the presence of local foci indicating neoplasms or stone formation. Treatment of this pathology is one of the pressing issues of modern gastroenterology.
The combination of medications prescribed by the attending physician and properly organized nutrition can prevent the development of various complications. It must be remembered that timely contacting a doctor and carefully following the instructions can be a guarantee of successful treatment.
Author of the article:
Mochalov Pavel Alexandrovich |
Doctor of Medical Sciences therapist Education: Moscow Medical Institute named after. I. M. Sechenov, specialty - “General Medicine” in 1991, in 1993 “Occupational diseases”, in 1996 “Therapy”. Our authors
How to treat the disease?
Only a doctor should treat an illness. Before prescribing treatment, the patient needs to undergo the necessary tests and identify the cause of the increased echogenicity.
A number of ailments can cause this deviation, and the doctor will prescribe medications that will treat the reasons that caused the deviation:
- acute pancreatitis. For this disease, medications are prescribed that reduce acid production, as well as those that will inhibit the enzymatic activity of the organ;
- lipomatosis The doctor will prescribe a strict diet. It should reduce the consumption of animal fats;
- presence of calcifications. A strict diet must be prescribed and surgery may be necessary;
- reactive pancreatitis. The doctor will prescribe medications that will treat the disease. It is important to follow a diet.
For all diseases that cause increased echogenicity of the pancreatic parenchyma, drinking alcoholic beverages and smoking should be avoided.
If the patient experiences pain in the abdominal area, then it is necessary to take medications that relieve pain - Diclofenac or Ketotop.
If a positive result does not occur, this means that you need to take stronger tablets, such as Promedol or Morphine.
To relieve swelling and relax the spasming muscles of the organ, you need to take No-shpa, Platyfillin.
Atropine, as well as enzymes and antioxidants, will help restore the production of pancreatic enzymes.
It happens that the echogenicity of the pancreatic parenchyma increases as a result of diet or after a cold.
This means that you should review your diet and take medications that help with colds.
A week after the measures taken, you need to undergo an ultrasound examination again - the echogenicity of the organ should be normal.
Do not be upset if the ultrasound report contains the wording “increased echogenicity”. Such a conclusion cannot be considered a diagnosis.
For such patients, the doctor will prescribe additional tests and listen to the patient’s complaints. Only after this the specialist will be able to draw a complete picture of the disease and prescribe the correct treatment.
Nowadays, you can very often come across an ultrasound report that states that the echogenicity of the pancreas is increased. Some people, having read this about their organ, immediately begin to look for treatment on the Internet, while others, on the contrary, consider it absolutely unimportant. Meanwhile, such an ultrasound symptom may indicate a very serious pathology of the gland. It is not a diagnosis and requires consultation with a gastroenterologist.
The concept of echogenicity
Echogenicity is a term that is used only to describe the ultrasound picture. It refers to the ability of the tissue to which ultrasound is directed (that is, high-frequency sound) to reflect it. The reflected ultrasound is recorded by the same sensor that emits the waves. Based on the difference between these two values, a picture of different shades of gray is constructed, observed on the device’s monitor screen.
Each organ has its own echogenicity index, and it may be homogeneous or not. The following dependence is observed: the denser the organ, the more echogenic it is (displayed as a lighter shade of gray). Liquids do not reflect ultrasound, but transmit it. This is called “echonegativity,” and fluid structures (cysts, hemorrhages) are called anechoic. For the urinary and gall bladder, the cavities of the heart, intestines and stomach, blood vessels, and ventricles of the brain, this “behavior” is the norm.
Thus, we have analyzed what the echogenicity of the pancreas is - this is the ability of this glandular tissue to reflect high-frequency sound emitted by an ultrasound transducer. It is compared with the properties of the liver (they should either be equal, or the pancreas should be a little lighter), and based on the resulting picture, they talk about a change in the echogenicity of the gland. The homogeneity of the organ is also assessed by this indicator.
An increase in the echogenicity of the pancreas is described when there are fewer normal glandular cells in the tissue of the organ (as we remember, fluid reduces echogenicity, and glandular cells are rich in it). Such a change can be observed both locally and diffusely. In addition, some factors may temporarily affect this indicator.
Warning! The description of echogenicity alone is not a diagnosis.
Types of echogenicity of the pancreas
There are several types of echogenicity:
- Isoechogenicity is the normal state of the organ, looks like a uniformly colored gray color.
- Hypoechogenicity - a decrease in the ability of the gland to reflect waves; the screen is black.
- Hyperechogenicity is the opposite situation - the organ is too dense, the degree of reflection is increased, during diagnosis the white color of the pancreas is determined.
- Anechoicity – reflection is completely absent, looks like a black area.
In addition, the echogenicity of the pancreatic parenchyma can be diffuse and local. The first speaks about changes in the entire organ, the second about pathological inclusions in the gland tissue (cyst, tumor).
Treatment of pathological hyperechogenicity
Treatment of conditions where the echogenicity of the pancreas is increased is prescribed only by a gastroenterologist, who must find the cause of this ultrasound symptom:
- if the cause is acute pancreatitis, therapy is carried out with drugs that reduce the production of hydrochloric acid in the stomach and inhibit the enzymatic activity of the pancreas;
- if hyperechogenicity is caused by lipomatosis, a diet with a reduced amount of animal fats in the diet is prescribed;
- if the etiological factor is calcifications, fibrosis or stones in the ducts, a diet is prescribed, and the need for surgical treatment is decided;
- reactive pancreatitis requires treatment of the underlying disease and diet.
Advice! Not a single specialist proceeds from the assumption that it is necessary to treat the tests, and not the person. Increased echogenicity of the pancreas is an ultrasound symptom, not a diagnosis. It requires further examination, and therapy is prescribed only on the basis of subsequent data.
Echogenicity is an important indicator when studying the internal organs of the human body. With its help, you can estimate the density of the object being studied. If the echogenicity in an organ increases or decreases, this is a reason to contact a specialist. For example, increased echogenicity of the pancreas - what does it mean, what actions should be taken if it is detected.
The gallbladder, endocrine glands, bladder, various types of cysts, etc. are fluid structures. They are homogeneous, and therefore ultrasound waves pass through them freely without reflecting them. That is, such liquid structures are echo-negative, even if the ultrasound power is increased. On the contrary, dense structures (bones, stones, etc.) are echo-positive, since they do not allow ultrasound to pass through them, completely reflecting it. During the study, the liver parenchyma is taken as a sample of echogenicity. It is with its indicators that the echogenicity of organs such as the kidneys and pancreas is compared. Among other organs that can reflect signals during ultrasound are the thyroid gland, adrenal gland, etc.
If your medical document says “increased echogenicity of the pancreas” during the examination, the doctor may suspect an inflammatory process or the appearance of edema. Diseases of this organ that change echogenicity also include increased gas formation, calcification of the gland, tumors of various origins and etiologies. A pancreatic tumor may appear due to changes in the cells of the endocrine and exocrine sections. 95% of malignant neoplasms occur in the last group of these cells, while endocrine cells are much less common.
The echogenicity of the pancreas in the normal state will be homogeneous. But with pancreatitis (acute, chronic), with portal hypertension, the echogenicity of the gland parenchyma increases. If the size of this organ is not increased, and the echogenicity of the pancreas is increased, this may indicate lipomatosis, when part of its tissue is replaced by fat. Sometimes this disease occurs in elderly patients with diabetes.
When the size of the gland decreases, such diffuse changes may indicate fibrosis, that is, replacement of gland tissue with fibrous (connective) tissue. Most often this happens when a person has suffered inflammation in the pancreas or has a metabolic disorder.
The increased echogenicity of the pancreas, coupled with other results of studies and examinations of the patient, allows the doctor to make an accurate diagnosis. Based on only one ultrasound, which gave a diagnosis of “increased echogenicity of the pancreas,” treatment is not prescribed, because this symptom may indicate a number of diseases of this organ.
When the pancreas is healthy, it produces more than a liter of pancreatic juice per day, which helps in digesting food. If increased echogenicity of the pancreas or other changes in the activity of the organ are detected, digestion is disrupted, which leads to serious health problems. After all, the digestive juice produced by the pancreas, in addition to digesting fats, carbohydrates, and proteins, also produces insulin, which helps tissues fully absorb glucose. It is not for nothing that the pancreas is also called an organ of secretion (external and internal). Therefore, it is so important to start treatment on time if the doctor told you after an examination that the echogenicity of the pancreas has increased.
Any changes in the pancreas identified during an ultrasound examination must be confirmed by other diagnostic examinations. Only after this complex therapy is prescribed.
Ultrasound examination of the pancreas is the most accessible, accurate and safe method of general diagnostics, actively used in modern gastroenterology. It allows you to identify changes in the size of the pancreas with a high degree of information, identify areas with atypical echogenicity, assess the diameters of the ducts, and confirm the presence of malignant and benign formations.
Echogenicity of the pancreas: how to understand this expression?
Ultrasound is one of the most accurate methods for studying internal organs.
A sensor aimed at the skin, like a magic wand, allows the diagnostician to understand what is happening inside a person, to see what changes have occurred in the structure of organs, to detect congenital pathologies, or to give a signal about the need to prevent them.
“Echogenicity” in ultrasound diagnostics means the ability of tissues to reflect the waves sent by the ultrasound sensor. And for some organs consisting of homogeneous tissues, this concept is not relevant, because waves pass through them unhindered without being reflected.
Speaking about the study of the pancreas, in this case we mean an organ with a dense structure, therefore the concept of echogenicity is an indicator of its health. Changes and deviations from the norm in the tissue structure will be visible on the device monitor, because The density of the pancreas will change.
What does "echogenicity" mean?
Echogenicity is the ability of the organs being examined to reflect ultrasound rays. The higher the echogenicity level, the denser the area subject to ultrasound.
Hollow organs and organs with fluids inside, such as:
- stomach;
- intestines;
- bladder;
- gallbladder.
Cysts are also classified as echo-negative formations. This means that ultrasound in this case will not provide the whole picture; other, more informative, in this case, examinations will be needed.
Echopositive ones are:
- liver tissue;
- spleen;
- pancreas, etc.
What does “isoechoic pancreas” mean?
An isoechoic pancreas is the norm for examination.
Increased or decreased echogenicity indicates an inflammatory process occurring in the pancreas.
Average echogenicity is characteristic of a homogeneous structure.
Mixed echogenicity indicates the presence of a heterogeneous structure of the tissues of the organ.
What signs can be used to understand deviations from the norm?
Doctors use the following terms to describe the organs found in tests:
- hyperechoic, echogenic structure - means that during examination, organs and tissues reflect ultrasound well (for example, bones), they appear bright white on the screen;
- anechoic (echotransparent) structure – characterizes the presence of liquid; there is a black spot on the screen;
- hypoechoic structure - used to characterize soft tissues; such tissues are dark gray on the screen;
- homogeneous structure – evenly distributed reflection from the organ;
- acoustic enhancement - bright area under organs with fluids;
- acoustic shadow is an echo-negative area (dark on the screen), which, for example, when examining the pancreas, can indicate pancreatitis or swelling of the organ. May indicate the formation of stones in organs.
Pancreatitis may also be indicated by hyperechogenicity or increased echogenicity of the pancreas, which can similarly be noticed by a diagnostician in the presence of a tumor, its calcification, increased gas formation, or portal hypertension.
Normal pancreas according to ultrasound
In a normal state, the pancreas is uniformly echogenic, its size is normal.
If a high echogenicity of the organ parenchyma is established, then this may be an indicator of the replacement of natural cells with fat cells, which indicates the onset of lipomatosis. It can progress in older people or people with diabetes.
A smaller deviation in the size of the pancreas from the norm may indicate replacement of organ tissues with connective tissue, which is characteristic of developing fibrosis.
At the same time, it is worth considering that echogenicity is not a constant value and it changes under the influence of:
- irregular stool passing;
- flatulence;
- season;
- appetite disorders;
- nutrition and lifestyle.
Which may mean that it is impossible to assess the condition of the pancreas only by its echogenicity; for a complete picture, it is necessary to take into account the structure of the organ, its size, as well as the presence of neoplasms in its parenchyma.
Therefore, it is important to prepare before the study; if many factors that affect echogenicity are difficult to influence, then everyone can adjust their diet:
- a few days before the ultrasound, give up milk;
- don't eat cabbage;
- exclude legumes;
- do not drink carbonated drinks.
What diseases are possible with increased echogenicity?
Based on the degree of echogenicity indicated by the diagnostician, one can judge what diseases have probably affected the pancreas.
| Diseases that can be determined by the degree of reflectivity of ultrasound of the pancreas | |
| Acute pancreatitis | Significantly increased; Increased with altered tissue structure |
| Chronic pancreatitis | Moderately elevated |
| Lipomatosis (replacement of organ cells with fat) | Average |
| Fibrosis | Increased with a decrease in the size of the gland |
What does echography of the pancreas show?
During the procedure, the specialist evaluates the location, size and contours of the pancreas. The capabilities of ultrasound scanning make it possible to examine the structure of the parenchyma, the state of the lumens of the pancreatic and bile ducts, and identify vascular pathologies. An important stage of diagnosis is the study of the reflectivity of pancreatic tissue - determining its echogenicity.
Normally, the pancreas has average echogenicity. Increased echogenicity may indicate lipomatosis of the gland, chronic pancreatitis, or age-related sclerosis of the gland. Reduced echogenicity is typical for mild forms of acute pancreatitis, as well as chronic forms of this disease. Heterogeneous structure of the pancreas, the so-called. mixed echogenicity, characteristic of pancreatitis, focal lipomatosis, metastatic lesions. Alternating areas of high and low echogenicity may also be a consequence of improper preparation. Therefore, a qualified approach and competent interpretation of the results play a key role when conducting this research.
In addition to the diseases described above, ultrasound of the pancreas allows you to diagnose the following pathologies:
- congenital developmental anomalies;
- cysts;
- malignant tumor of the pancreas;
- diffuse pathologies of the parenchyma;
- concretions (stones) in the ducts of the organ;
- enlargement of adjacent lymph nodes;
- abscess and a number of other pathologies.
What can a violation of the density of the pancreas lead to?
The pancreas plays a major role in the process of digesting food. It produces a digestive secretion that breaks down food into simple chemical compounds. This internal secretion organ is extremely important in the process of normalizing the amount of sugar in the blood, as it secretes the hormones glucagon and insulin. If the production of these hormones is reduced, this can cause diabetes. Therefore, taking care of this internal secretion organ is no less important than taking care of the heart or liver.
In a healthy person, the granular structure of the pancreas is uniform and without dark spots.
The heterogeneous structure of the pancreas will certainly lead to a change in its reflectivity. In acute or chronic pancreatitis, the echo density of the pancreas increases.
In addition, the reflectivity of this organ may be impaired as a result of:
- swelling;
- increased gas formation;
- portal hypertension;
- the occurrence of calcification;
- presence of a tumor.
It is worth paying attention to possible changes in the volume of the gland. If it is not enlarged, but the echogenicity is increased, then this may indicate the manifestation of a disease such as lipomatosis. Most often it occurs in older people with diabetes.
Important information: What tests to take to check the pancreas
Reduced echogenicity of the pancreas indicates hyperplasia - an excessive increase in the number of living cells in an organ or tissue. The disease itself is not dangerous, but it can cause pathological tumors.
The gland can decrease in size if its structure is disrupted by connective tissue cells, which leads to the development of fibrosis. This disease can occur in patients who have serious metabolic disorders or who have had pancreatitis.
All people have different echogenicity of the pancreas. Moreover, it can change throughout life. The doctor can determine the average echogenicity of this organ, but this is far from constant.
Reflectivity is influenced by appetite, the type of food you prefer, lifestyle, or even the time of year.
Therefore, doctors do not make final conclusions based only on the echo density of an organ. Specialists look for the causes of tissue heterogeneity, changes in size, and the appearance of formations or tumors. For example, the detected diffusely heterogeneous tissue structure in combination with an increase in the size of the gland already significantly narrows the list of possible diseases.
Normal parameters of the pancreas during ultrasound examination
The organ is divided into three parts: the head with a process, the body and the tail. Normally, it has smooth, clearly defined contours and is delimited from adjacent tissues. Echogenicity is average, identical to that of a healthy liver. Increased echogenicity of the pancreas in older people is normal.
Description of the normal structure of the pancreas on ultrasound
The tissues are homogeneous, with a fine-grained or coarse-grained echo structure. Vessels without deformations, blood flow within normal limits. Pancreatic duct – without extensions (1.5-2.5 mm). There are no stones.
Normal size of the pancreas
- Head: adults – 18-28 mm, children – 10-21 mm;
- Body: in adults –8-18 mm; in children – 6-13 mm;
- Tail: in adults – 22-29 mm, in children – 10-24 mm.
Preparing for an ultrasound of the pancreas
Proper preparation is of utmost importance when conducting this type of research. The information content of visualization and the accuracy of diagnosis depend on it. The set of preparatory measures is identical to those prescribed before an ultrasound of the abdominal organs: liver, spleen, gall bladder. The main task is to reduce the amount of gases in the intestines, which serve as an obstacle to knot waves.
- following a special diet 2-3 days before the ultrasound;
- taking medications for gas sorption (for people prone to flatulence);
- observance of a 9-12-hour pause in nutrition before the examination.
You can read more about the nuances of preparing for an ultrasound of the abdominal organs and pancreas in the corresponding section of the site.
Before an ultrasound scan of the pancreas, do not do cleansing enemas and do not take laxatives. The examination is carried out on an empty stomach. In special cases, when only the Wirsung duct is diagnosed, a light breakfast is acceptable before the procedure.
The echogenicity of the liver and pancreas will be increased
During an ultrasound of the pancreas, the echogenicity of the liver and pancreas parenchyma is interpreted as a norm. These organs are interconnected and any deviations in these organs will mean that there are problems that need to be eliminated in the future. Such an examination of the parenchyma using ultrasound can be primary, or it can be repeated after the person has passed a series of additional tests. Repeated examination will confirm the diagnosis.
Carrying out the procedure at the Endos gastroenterology center
During the ultrasound, the patient takes off his outer clothing and lies on his back, quickly removing his clothes. The diagnostician applies a special gel to the projection site, places the device’s sensor on the body and slowly moves it across the abdomen. During the procedure, for better visualization of the organ, the patient is asked to perform several simple actions: hold his breath, fill his stomach with air, etc. Diagnostics usually does not exceed 8-10 minutes and does not cause any discomfort.
Upon completion of the procedure, the doctor prepares a transcript of the ultrasound of the pancreas, which is immediately given to the patient. It reflects detailed data on the condition of the organ and the nature of the identified pathologies, if any. If the clinical picture is unclear, additional examination methods are prescribed. Based on their results, gastroenterological specialists make an accurate diagnosis and prescribe further treatment.
Preparation and execution
In order to obtain correct results that correspond to the real state of affairs, it is necessary to prepare for the study using an ultrasound machine. Complex or specialized procedures are not required for quality preparation.
The main thing that a person must do is not to eat before the examination (usually an ultrasound is scheduled in the morning so that the procedure takes place on an empty stomach). There is a recommendation to refrain from eating for up to 12 hours before the start of the study.
It is important to consider that in approximately 1/3 of all studies, difficulties arise in obtaining a high-quality image on the monitor and reliable information. This is due to the presence of flatulence. That is why it is recommended to observe some dietary restrictions 2-3 days before the procedure.
Excluded from the menu:
- fresh vegetables and fruits;
- Rye bread;
- various dairy products;
- legumes
It is recommended to use a decoction of dill and mint seeds, as it reduces the likelihood of developing flatulence. Additional recommendations are bowel movements (12-24 hours before the procedure) and refusal to take laxatives, as well as performing cleansing enemas.
An ultrasound is performed as follows:
- The abdominal area should be freed from clothing (the patient takes off his shirt).
- A man lies on his back on a couch.
- The specialist applies a special gel to the area of the abdomen being examined.
- After this, it connects sensors to this area.
- Directly during the examination, the patient must, at the request of the doctor, take a deep breath and also hold his breath for several seconds.
You will also need to inflate your stomach - this is necessary in order to displace the intestines. This will allow your doctor to better see the pancreas and the areas around it.
Also during the procedure, for better visualization of the parts being examined, the doctor makes rotational or rocking movements with the sensor of the device.
During the study, the size of the gland and liver are measured, and the structure and surrounding tissues of these organs are examined. The examination time is no more than 8 minutes; the patient does not experience any negative or painful sensations during the process.
Video about preparing for an abdominal ultrasound:
How to sign up for an examination
You can sign up for a profile ultrasound by calling +7 or leaving an online application on our website. We offer the highest diagnostic standards and affordable prices in Moscow. The cost of a comprehensive examination of the abdominal organs is 1,800 rubles.
Working hours: from 8:00 to 20:00, seven days a week. We are located: Moscow, metro station Shchukinskaya st. Gabrichevskogo 5, k 10. Access to the complex by car is made using a pass previously issued on our website.
I would like to express my deep gratitude to the doctor and nurse for their sensitive attitude towards patients, for their impeccable, well-coordinated work, for their professionalism! I heard so many negative reviews about the colonoscopy procedure that I was afraid to go. But at the appointment, even when they warned me that it would be painful, I did not experience any discomfort. Once again I want to say – thank you so much!
I made an appointment for a morning appointment, but didn’t have dinner. I was very afraid, but decided to have a gastroscopy in my sleep. It turned out – one little injection and that’s it! I woke up as if nothing had happened. Thanks to the Endos Center team for their sensitive attitude and professionalism! I advise everyone to do gastroscopy in their sleep. No discomfort. Valeria 38 years old
The attending physician referred me to an endoscopist for gastroscopy. I read reviews on the Internet and chose Endos Center. I had never swallowed a light bulb before, and I must admit I was very worried. Pleasant atmosphere of the clinic, caring, polite staff, miracle doctors. I was not mistaken in entrusting my health to the specialists of the Endos Center.
I made an appointment for a morning appointment, but didn’t have dinner. I was very afraid, but decided to have a gastroscopy in my sleep. It turned out – one little injection and that’s it! I woke up as if nothing had happened. Thanks to the Endos Center team for their sensitive attitude and professionalism! I advise everyone to do gastroscopy in their sleep. No discomfort. Valeria 38 years old
The attending physician referred me to an endoscopist for gastroscopy. I read reviews on the Internet and chose Endos Center. I had never swallowed a light bulb before, and I must admit I was very worried. Pleasant atmosphere of the clinic, caring, polite staff, miracle doctors. I was not mistaken in entrusting my health to the specialists of the Endos Center.