Causes of the disease
The most common causes of reflux - esophagitis are poor diet, prolonged alcohol consumption and very spicy foods. With improper treatment or its absence, scars form on the walls of the esophagus. Reflux can also occur due to muscle weakening, when the valve begins to leak gastric juice.
The most common causes of esophagitis are:
- high pressure and distension in the peritoneum;
- improper diet;
- spicy, smoked and fatty dishes;
- stress;
- chemical factors;
- obesity;
- ulcers;
- period of bearing a child;
- excessive drinking;
- smoking.
Any of these factors can lead to exacerbation and return of the disease. Even a simple bend forward is enough for this.
What causes the pathology?
At the beginning of the disease, a person feels a constant burning sensation, pain in the abdomen and chest. If you do not consult a doctor in time, erosion-affected lesions and small ulcers form, which grow over time and worsen the physical condition.
Accompanying illnesses:
- ulcer;
- pyloroduodenal stenosis;
- chronic cholecystitis;
- hiatal hernia;
- chronic pancreatitis;
- oncological diseases - tumors in the stomach (cancer);
- poor esophageal patency.
The development of reflux esophagitis occurs due to weakening muscle tone and poor functioning of the esophageal (cardiac) sphincter. It remains open, and the mass contained in the stomach freely enters the esophagus.
Causes of reflux esophagitis:
- high pressure on the diaphragm;
- decreased muscle tone of the lower esophageal sphincter (LES);
- poor bowel cleansing and problems with fluid excretion;
- stress;
- irritation of the mucous membrane when eating hot food and drinking, alcohol, or drinking large amounts of coffee;
- binge eating;
- chemical factors (excess iodine, strong acids, alkalis), toxic substances entering the esophagus through air or food;
- smoking;
- violation of acid formation;
- increasing the aperture;
- stenosis;
- impaired gastric emptying.
Reflux esophagitis of the esophagus sometimes occurs after surgery performed on the stomach. The development of the disease is often provoked by a diaphragmatic hernia. Excess weight or heavy lifting increases pressure on the abdominal cavity and part of the stomach penetrates into the chest.
The development of reflux esophagitis is provoked by: poor diet, poor lifestyle, pathological condition and physiology of the body:
- the process of gestation;
- overvoltage;
- food allergies;
- obesity;
- poisoning from food, drink or chemicals;
- taking medications that help relax the sphincter muscle.
Types of esophagitis
The classification of esophagitis is divided into 2 main forms - acute and chronic. They in turn are divided into:
- pseudomembranous;
- catarrhal (otherwise superficial);
- necrotic;
- exfoliative;
- hydropic;
- erosive;
- phlegmonous (can be limited or diffuse).
Acute esophagitis occurs at the bottom of the esophagus and is often combined with gastric diseases.
Pathology occurs against the background of vitamin deficiency, gastrointestinal problems, and infections. Acute reflux causes pain when eating or drinking liquids. Chronic appears as a separate disease or forms as a complication after the acute form. Accompanied by stable inflammation of the esophagus. Pain appears in the sternum. Often the chronic form is supplemented by gastritis
Stages of development
Esophagitis develops in stages. At the first stage (A) of the disease, the affected area is 4-5 millimeters in diameter. There may be several such places on the mucous membrane. In this case, the affected areas do not touch.
At the second stage (B) of the disease, several defective areas expand and become more than 5 mm in diameter. At the same time, the affected areas begin to merge. Large defective areas are formed. However, they do not apply to the entire mucous membrane.
One third of it is affected at stage 3 (C). The last stage, the fourth, is accompanied by extensive ulcers on the mucous membrane. The affected areas occupy 75 percent of the surface. Stenosis may be diagnosed.
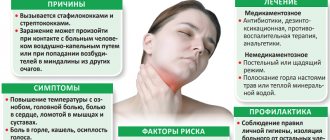
Symptoms
The first signs appear: general malaise and fever. A person is tormented by pain behind the sternum, throughout the esophagus. Additional symptoms of reflux esophagitis may include heartburn, vomiting, or hiccups.
Pathology can occur secretly. Sometimes esophagitis is accompanied by signs that are uncharacteristic of this disease. Each form has the same symptoms:
- lump in throat;
- heartburn;
- sour belching;
- burning or pain in the chest;
- nausea.
An hour and a half after eating, pain in the esophagus begins. This is already pronounced inflammation. Symptoms are worse when the person lies down. Signs of reflux esophagitis may vary depending on the stage and type of disease:
- Pulmonary is caused by heartburn and unpleasant belching. Obstruction of the bronchi appears - prolonged cough, nocturnal suffocating attacks, lack of air. This can trigger the formation of asthma.
- Cardinal is accompanied by symptoms inherent in angina pectoris due to the close proximity of nerve endings. Pain always occurs after sour or spicy foods, fried or fatty foods, or overeating.
- Otolaryngological , in addition to belching and heartburn, is accompanied by sore throat and sore throat. Nasal congestion and discharge in the form of clear mucus may appear.
- The dental form is accompanied by the appearance of caries. This is facilitated by gastric juice, which eats away tooth enamel.
Symptoms of subtypes of chronic reflux esophagitis
| Types of pathology | Symptoms |
| Catarrhal (aka superficial) | Difficulty swallowing food. After eating, a person begins to suffer from dull pain in the esophagus, belching mucus, and heartburn. While eating, a burning sensation and rawness increases behind the sternum. Pain can radiate to the neck, shoulder blades and jaw. Increased salivation appears. |
| Exfoliative | Constant pain between the shoulder blades, worsening when swallowing liquid or inhaling. General weakness, anemia, body temperature rises. When taking tests, a violation of the level of leukocytes is detected. |
| Hydropic | This form is a continuation of catarrhal. In addition to its inherent symptoms, swelling of the esophagus additionally occurs. |
| Erosive | Pain appears, “walking” along the entire length of the esophagus. Mainly during meals. There is a burning sensation in the chest, belching with blood appears and the remains of undigested food come out. The person experiences severe fatigue, fainting, and mild anemia. If an additional infection occurs, bleeding occurs and esophageal cancer may occur. |
| Pseudomembranous | Difficulty swallowing. During this process, the pain in the chest increases. A cough with blood appears. A sign of recovery is the release of pieces of fibrinous film into the oral cavity. |
| Necrotic | Intense pain, dysphagia, frequent vomiting, in which pieces of mucous are visible. In the complicated form, bleeding occurs. This can provoke the appearance of purulent mediastinitis and abscess. |
| Phlegmonous | Pain when swallowing food, fever, dysphagia. A disturbance in the level of leukocytes is detected. Pain occurs when you move your neck. The same sensations occur when palpating the abdominal muscles. A purulent abscess may begin. This is accompanied by vomiting with blood clots. The person shudders, sweats profusely and feels unbearable pain in the sternum. |
The hemorrhagic form is a type of acute esophagitis. Appears very rarely, against the background of severe erosive inflammation. Accompanied by bloody vomiting and melena (tarry stool).
Note! Without timely treatment of the disease, it can last for years. Over time, the symptoms will intensify, and eventually irreversible changes in the mucous membrane will occur and scars will appear on it.
Symptoms and treatment strategy for reflux esophagitis
The first warning sign is heartburn. The latter can occur regardless of the time of day, after eating, or when the body is in a horizontal position.
In addition, pain occurs in the chest area, which is often perceived as cardiac pain. Sometimes the listed symptoms are completely absent, but there is a violation of the swallowing process. The latter indicates the development of cicatricial narrowing and the progression of pathology.
Other symptoms of the disease:
- Sour or belching air;
- Failures in the swallowing reflex, disruption of food passage;
- Chronic cough, blockage of the bronchi with viscous secretions;
- Rhinitis and pharyngitis. The mucous membrane of the pharynx and nose becomes inflamed due to frequent contact with the contents of the stomach;
- Destruction of tooth enamel by acidic gastric juice.
Sometimes even an experienced doctor finds it difficult to identify this disease, since it has a similar clinical picture to many gastrointestinal pathologies.
In order to detect the disease in a timely manner, it is necessary to conduct a number of studies. Typically, a set of diagnostic procedures includes esophagoscopy (examination of the esophagus using endoscopic equipment), X-rays, biopsy of the mucous membrane, esophageal pH-metry (to determine the level of acidity).
Diagnosis of the disease
When diagnosing esophagitis, the degree of damage to the mucous membrane and the form of the disease are determined. For this, an x-ray is used, the images of which clearly show whether the valve is allowing gastric juice to pass through. During endoscopy, the entire length of the esophagus is examined.
We recommend watching the video: Reflux esophagitis - My medical history
Before treating reflux, scintigraphy is performed. It shows the presence or absence of abnormalities in the gastrointestinal tract. A biopsy is taken for histological analysis. The pH-metry procedure determines the degree of acidity in the stomach.
What is catarrhal and erosive reflux esophagitis?
The catarrhal form of the disease is most often diagnosed. In addition to the main symptoms listed above, the doctor, during a diagnostic study, detects swelling and hyperemia of the esophageal mucosa. Catarrhal esophagitis occurs due to insufficient function of the cardiac sphincter of the esophagus.
Erosive reflux esophagitis is characterized by stronger and deeper damage to the mucous membrane. This form of pathology is less common than the previous one, but much more often leads to various complications. Thus, the disease is accompanied by the formation of ulcers and erosions on the mucous membrane of the esophagus.
There are 3 degrees of pathology:
- I – single formation of small erosions;
- II – increase in the affected area;
- III – formation of a chronic ulcer.
Treatment
Treatment of esophagitis is always complex. The scheme includes medications, diet, physiotherapy, exercise therapy and other methods. Initially, therapy is aimed at eliminating the causes of the disease.
General events
Treatment of gastric reflux begins with general measures aimed at correcting quality of life. This significantly reduces muscle damage, which helps speed recovery:
- Stop smoking, as nicotine increases acidity and relaxes the digestive muscles.
- After eating food, you should not lie down immediately; it is better to sit quietly or go for a walk. Fast walking and running are excluded.
- Limiting physical activity helps reduce symptoms of the disease. You cannot lift anything more than 3 kilograms.
- A couple of hours before bedtime, food and alcohol are excluded.
- You need to sleep on a raised (15-20 cm) pillow.
- Avoid wearing tight clothing.
If there are additional diseases (obesity, ulcers, etc.), you need to treat them. Otherwise, therapy for reflux esophagitis will not have an effect.
Medication
When a diagnosis of reflux esophagitis is made, a treatment regimen is prescribed depending on the type of development of the disease:
- To reduce the activity of AP enzymes, Pantoprazole and Rabeprazole are used.
- After the 13th week of pregnancy, Lansoprazole is prescribed.
- For bronchial asthma, Esomeprazole.
- If liver function is impaired, any PPIs (proton pump inhibitors) are used, but Rabeprazole is preferable.
- To quickly and steadily reduce acidity, Pantoprazole or Lansoprazole is used.
If PPI therapy is ineffective, then histamine blocker medications are prescribed. However, they are used in large dosages, so they are used only when absolutely necessary - Nizatidine, Famotidine, Roxatidine and their analogues.
To reduce the aggressive impact of reflux and its quantity, prokinetics are prescribed. They improve digestion and facilitate the passage of food. The most effective include:
- "Domperidone";
- "Cisapride";
- "Metoclopramide."
To quickly eliminate pain in the esophagus or heartburn, antacids are prescribed. They do not cure the disease, but they partially alleviate the symptoms of reflux. Can be assigned:
- "Maalox";
- "Renny";
- Gaviscon;
- "Almagel";
- "Megalak".
The listed drugs act quickly, retain their effect for a long time, and significantly reduce acidity. For treatment of cardia insufficiency (incomplete closure of the valves), Ranitidine, Omeprazole, Solpadeine, and Regidron are used. In case of complications, antibiotics are prescribed.
Diet features
Treating reflux with diet is one of the main directions in the treatment of esophagitis. Food can only be prepared in a few ways:
- Meat and fish can be wrapped in special food bags. This helps you cook food without adding oil. Spices are replaced with chopped vegetables, dried herbs and a small amount of salt.
- When baking in the oven, you also don’t need a lot of oil, which eliminates the need to cook fatty dishes. It is best to add water to the ingredients. Then meat, fish or vegetables will become soft and will be quickly digested.
- Modern models of microwave ovens facilitate the preparation of dietary dishes. Radiation does not affect the quality of food. It turns out low-fat and tasty.
- You can cook dishes in a slow cooker. The extinguishing mode is usually recommended. At the same time, the products do not lose their nutritional value and produce abundant juice. You can only season food with herbs instead of spices.
- Food can be boiled, stewed or steamed on the stove.
Attention! The likelihood of esophagitis increases due to poor diet, smoking, drinking large doses of coffee, undiluted fruit juices and alcoholic beverages.
For intestinal esophagitis, the use of mayonnaise or butter in dishes is excluded, or they are added in minimal quantities. Ketchup, hot sauces, horseradish and mustard should not be used for dressings. They will irritate the mucous membranes even more and increase the acidity of gastric juice. Excessively hot or cold food is prohibited.
When diagnosing reflux esophagitis, therapy includes strict dietary restrictions.
| Completely excluded | Allowed |
| · natural juices; · alcohol, soda and other drinks that increase stomach acidity; · sweets; · coffee, strong tea; · black bread; · White cabbage; · fresh milk; · legumes; · marinades, smoked meats; · spicy dishes, spices, pickles · fruits (mostly citrus fruits); Fried and fatty foods; · rich broths and soups; · chewing gum. | · crackers, yeast-free bread; · fermented milk products (low-fat cheese, cottage cheese, yoghurts); · soft-boiled eggs or steamed omelette; · porridge with water (you can add a little milk); · boiled, stewed or steamed lean meat (can be baked in the oven). |
The menu includes vegetables and fruits, but it is not recommended to eat them raw; it is advisable to bake or stew them. You need to eat every three hours, in small portions. The last dinner should be 4 hours before bedtime.
Physiotherapy
GERD can be treated with physical therapy. It is prescribed for severe symptoms and pain. Types of physiotherapeutic procedures for esophagitis:
- TCEA (transcranial electroanalgesia);
- aerotherapy;
- electrosleep therapy;
- electrophoresis with antispasmodics;
- baths with sodium chloride;
- galvanization;
- interference therapy;
- UHF (ultra high frequency inductothermy);
- cryotherapy in the epigastric region;
- magnetic and laser therapy;
- pine and iodine baths;
- galvanization of the brain of the head.
Physiotherapy depends on the form of the disease, its severity, and the presence or absence of complications. It helps restore the functionality of the autonomic nervous system, partially reduces inflammation, and accelerates the healing process. At the same time, it improves the functioning of the digestive system and relieves spasms.
Exercise therapy
With esophagitis, physical exercise helps speed up the healing process and helps strengthen the body.
Workouts and exercises are selected depending on the severity of reflux. In this case, the maximum load tolerance must be taken into account. Exercises help get rid of heartburn, develop the muscular system, strengthen the sphincter, and promote rapid healing of ulcers.
The main direction is breathing exercises. The main methods include diaphragmatic, according to Strelnikova. Breath-holding exercises are worked on separately, and aerobic training is carried out.
Surgery
Surgical treatment of esophagitis is a last resort and is used for serious complications. Surgical intervention may be prescribed for severe bleeding in the esophagus, persistent stricture, or irreversible damage to the sphincter.
Also, surgery is prescribed in the case of a precancerous condition of the mucous membrane, with active proliferation and degeneration of cells. Surgery is indicated for stage 1 and 2 cancer. During surgery, the esophageal tube is completely or partially removed, the integrity of the organ is restored, and the tumor is excised.
Diet for reflux esophagitis
Diet correction is a mandatory component of the treatment complex. First of all, you need to exclude the following products from the menu:
- alcohol (increases acidity, relaxes the sphincter);
- strong tea, coffee, soda;
- chocolate (promotes relaxation);
- mushrooms;
- mayonnaise, ketchup, hot seasonings;
- smoked meats;
- marinades;
- legumes, especially peas and beans (increase intra-abdominal pressure);
- canned food;
- sour juices;
- fresh and sauerkraut;
- fat;
- black bread;
- fast food, chips, chewing gum;
- fried foods.
If discomfort occurs after eating, you need to pay attention to what foods were eaten and, accordingly, exclude them from the diet.
The diet must include the following products:
- pureed cottage cheese (low fat);
- sour cream and milk (low fat);
- fresh and soft-boiled chicken and quail eggs;
- homemade crackers;
- any porridge;
- steam cutlets;
- baked sweet apples;
- baked vegetables;
- baked and boiled fish.
You can diversify your diet with foods that do not cause discomfort after consumption. In addition, you need to pay attention to your diet. It is necessary to avoid nervous overload at work, get good sleep, eat 4-5 times a day (eat slowly, avoid rushing), after a meal it is recommended to walk or work while standing (you cannot sit).
It is recommended to wear loose clothing that does not restrict movement in the abdominal area. In addition, you cannot strain the abdominal muscles, so lifting weights is also excluded.
Traditional methods
The treatment regimen for reflux esophagitis includes folk remedies as an auxiliary therapy. In this case, herbal decoctions, healing baths and teas are used.
One of the popular methods for treating reflux with heartburn is baking soda. However, this brings additional harm. During the first passage through the esophagus, the mucous membrane is even more irritated. In response to alkalization, a strong release of acid occurs, and reflux becomes even more aggressive. Therefore, it is advisable to use antacids instead of soda.
Reflux esophagitis, caused by spicy, fatty or smoked foods, can be treated in the initial stage with simple herbs. Herbal decoctions of motherwort, licorice, lemon balm and flax seeds help relieve inflammation.
Esophagitis in adults often causes heartburn and belching. Rose hips, valerian, dandelion flowers and calamus powder save from them. Plantain juice has a strong healing effect. However, it is contraindicated in people with acid reflux.
For the treatment of chronic esophageal esophagitis, chamomile decoctions are made. They can be combined with flax seeds. The product is drunk three times a day. Flax seeds simultaneously have an enveloping effect and reduce high acidity. This is a good prevention of cancer and reduction of symptoms of the disease.
Honey should be consumed a couple of hours before meals. It is advisable not in whole form, but diluted with a small amount of liquid. You should not consume honey during an exacerbation of esophagitis. This will lead to irritation of the esophageal mucosa.
Sea buckthorn oil has a healing effect, improves secretory function and digestion. Potato juice envelops the mucous membrane, creating an additional protective film. This helps reduce heartburn and chest pain.
Inflammation of the esophagus: how to treat it
Treatment of acute inflammation of the esophagus:
- for the treatment of infectious diseases that cause esophagitis, antibiotics are used in full dose (parenterally);
- food intake is stopped for several days, and in the case of chemical burns, necrotic or severe hemorrhagic esophagitis, the patient is transferred to parenteral nutrition, with a subsequent transition to chemically and mechanically gentle food;
- to relieve the symptoms of inflammation, solutions of the medications novocaine, collargol, tannin are used internally;
- To reduce the phenomena of esophageal dyskinesia, prokinetics in tablets are used (Domperidol, Itoprid);
- for multiple erosions, solcoseryl is used;
- for hemorrhagic esophagitis complicated by bleeding, aminocaproic acid, Dicynon, Vikasol are used;
- Correction of strictures is carried out by bougienage.
How to treat chronic inflammatory processes in the esophagus:
- Diet therapy. The frequency of meals, methods of cooking, the list of permitted and requested products are discussed in detail with the attending physician.
- Drugs that reduce the pH of the stomach contents by neutralizing hydrochloric acid (antacids - Maalox, Almagel, Gaviscon, Phosphalugel), or by suppressing its formation in the stomach: PPI (Omeprazole, Rabeprozole) or IGR (Famotidine, Roxatidine, Nizatidine).
- Drugs that enhance the motility of the stomach and intestines, accelerate the movement of food from the stomach into the intestines, enhance peristalsis of the esophagus, normalize the tone of the sphincters - prokinetics (Domperidol, Itopride).
- Physiotherapeutic treatment (laser therapy, magnetic therapy, balneotherapy, cryotherapy).
- Folk remedies.