Description
A perforated or perforated duodenal ulcer is a serious condition with high mortality. When the duodenum is ulcerated, the stomach is often affected. This forms a passage from the organ to other parts of the gastrointestinal tract or peritoneum. Due to constant exposure to irritants of a chemical, physical and bacterial nature located in the duodenal contents. Against this background, peritonitis develops. This consequence requires a strict diet and urgent surgical intervention.
Perforation of the ulcer most often occurs in the anterior wall of the bulbous part of the duodenal process. This outcome is equally characteristic of the acute course and the acute chronic phase of the ulcerative process. The average size of wounds is 3 mm, less often - up to 100 mm.
General information
Ulcerative defects of the gastrointestinal tract, in one form or another, occur in approximately 10% of the entire adult population of the planet. In 70-80% of cases, the disease develops at the age of 20-50 years. The disease occurs more often in men than in women. In particular, women are protected by the sex hormones estrogens, which can reduce stomach acidity.
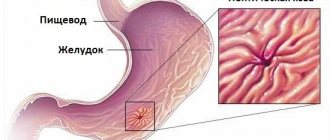
A perforated or perforated ulcer is a dangerous complication of a stomach or duodenal ulcer, when a hole forms at the site of the ulcer through which gastroduodenal contents (food particles, microorganisms, gastric juice, bile) flow into the abdominal cavity. Typically, the perforation looks like a round hole with smooth edges with a diameter of up to 5 mm.
Discharge from the stomach or duodenum causes a chemical burn of internal organs, accompanied by severe pain. Possible infection. As a result, peritonitis develops, to eliminate the consequences of which, and the perforation itself, immediate medical attention is necessary.
In the esophagus, small and large intestines, this phenomenon occurs very rarely. Perforated ulcers are typical specifically for the stomach and duodenum. Therefore, the concept of “perforated (perforated) ulcer” is associated with them.
There is a clear connection between the location of a perforated ulcer and the patient’s age:
- In 80% of cases, perforation is observed in the duodenum in men 20-40 years old. In this case, an ulcerative defect can develop rapidly, and its perforation often takes an unsuspecting person by surprise.
- Cases of perforation of stomach ulcers are more common in people over 50 years of age. In these cases, chronic ulcers are more likely to perforate.
According to various sources, perforation is observed in 3-35% of patients with gastrointestinal ulcers. This indicator depends on various factors: from the climatic conditions of the country of residence, the level of development of medicine, food traditions and ending with individual food preferences and bad habits. For patients in the post-Soviet space, this figure, according to some data, is approximately 8%.
Read more about perforated ulcers
A perforated gastric ulcer is not considered an independent disease. It occurs against the background of an existing peptic ulcer (acute or chronic) of the stomach and duodenum. When a peptic ulcer is not treated, hydrochloric acid can corrode the organ mucosa until a through hole appears.
This dangerous defect can appear in the intestines, stomach, and esophageal walls. But most often, perforation appears in the lower part of the stomach or in the duodenal bulb. The diameter of the perforated hole can reach 10 cm.
Perforated ulcers of the stomach and duodenum occur in almost 10% of patients with a history of gastric ulcers.
Due to the rapid spread of infection in the abdominal cavity, the mortality rate for perforated ulcers is very high.
If emergency medical care is provided, the mortality rate is no more than 18%. When more than 12 hours pass from diagnosis to surgery, mortality rates reach 70%.
Perforated gastric ulcers occur in various categories of the population, including children, but men are several times more susceptible to it than women. More often this disease is diagnosed in men 20-50 years old.
Analysis of case histories suggests that almost 70% of perforated ulcers before perforation are not indicated by any clinical manifestations, i.e. are "mute".
How does perforation occur?
A perforated duodenal ulcer occurs as a result of ineffective conservative therapy or failure to form scar healing. As a result, instead of healing, a through hole is formed in the duodenum.
More often, perforation of the duodenum affects young men under the age of 40, whose duration of peptic ulcer is more than 3 years.
The contents of the duodenum penetrate through the perforation into the abdominal cavity, causing inflammation of the peritoneum. The perforated hole is surrounded by fibrinous deposits. In some cases, perforation is accompanied by bleeding from a duodenal ulcer.
The most common location is the area of the duodenal bulb.
In 10% of cases, perforation occurs in the retroperitoneal region or subhepatic space. Such atypical perforation is called covered. Subsequently, a subhepatic or retroperitoneal abscess is formed in this place.
Causes of the disease
In most cases, the cause of perforation is a complication of a chronic or acute ulcer. That is, perforation (perforation) occurs when a chronic ulcer reaches a state where all layers of the organ wall are corroded through and through. Or bringing an acute ulcer to a similar state.
Often the reason for bringing the disease to a critical state is due to the patient himself, his lack of seriousness towards treatment. Neglect of doctor's recommendations: diet, diet, bad habits. This is, for example, when a patient continues to drink alcohol, even after discovering an ulcer.
Seasonal exacerbations play an important role. Thus, exacerbations of peptic ulcers in spring and autumn, respectively, lead to an increase in cases of perforation of ulcers during these periods.
In up to 20% of cases, the cause of perforation of the ulcer is the asymptomatic development of the disease or without obvious symptoms. With this course of the disease, the ulcer can be detected after perforation.
The following negative factors can provoke perforation:
- Increased aggression on ulcer formation from gastric juice (increased acidity).
- Sudden increase in intrauterine pressure.
- Non-compliance with the diet: consumption of junk food and drinks.
- Drinking alcohol, smoking.
- Defective diet.
- Chemical poisoning.
- Non-steroidal anti-inflammatory drugs (aspirin, ibuprofen, ketonal, etc.), some chemotherapy drugs, corticosteroids, anticoagulants.
- Severe emotional stress.
- Exacerbation of the underlying disease.
- Hereditary tendency to disease.
- Infection with the bacterium Helicobacter pylori.
- Overeating in the presence of an ulcer.
- Active physical activity during exacerbation of peptic ulcer disease. And also, significant physical activity immediately after eating.
The destructive effect can be either direct - the direct physical or chemical effect of food, drinks and other substances on the gastrointestinal mucosa. So and indirectly, when disturbances in the production of hormones and other substances in the body lead to a weakening of the protection of the walls of the stomach and duodenum.
There are factors that combine several harmful effects at the same time. This is, for example, smoking. Direct damage to the mucous membrane occurs when saliva gets in contact with harmful smoke substances dissolved in it and partial penetration of the smoke itself into the stomach. And the harmful effects of smoke elements entering the body through the lungs into the blood.
These same negative factors are the initial causes of defects in the mucous membranes of the gastrointestinal tract.
Etiology
The chance of developing the disease is possible if a person is diagnosed with the chronic stage of an ulcer or has had acute attacks. A perforated duodenal ulcer can also form for the following reasons:
- inflammation near the source of damage;
- overeating;
- increased level of hydrochloric acid;
- consumption of prohibited foods and alcohol;
- strenuous physical activity.
As a result of modern research, doctors have determined that the cause of the disease is the bacterium Helicobacter pylori. The formation of a perforated ulcer is directly influenced by those factors that cause the development of a common peptic ulcer:
- deterioration of immunity;
- stress;
- sleep disturbance;
- taking illegal or heavy drugs;
- smoking and alcohol;
- unbalanced diet;
- heredity;
- the presence of other gastrointestinal ailments.
Classification of perforated ulcers
Ulcers causing perforation vary according to the following parameters.
According to the nature of ulcers causing perforation:
- Perforation of acute ulcers.
- Perforation of chronic ulcers.
According to the clinical development of the disease:
- A typical form of development is the entry of the contents of the stomach or duodenum into the abdominal cavity. In this case, there are 3 periods of development of the disease:
- Severe painful shock.
- Imaginary well-being.
- Development of acute diffuse peritonitis.
- Atypical form of development: Covered perforation (the hole is obscured by the omentum or adjacent organ).
- The contents of the stomach or duodenum flow into the abdominal space, the cavity of the lesser or greater omentum, adhesive zones and other places (except for direct entry into the free abdominal cavity).
- Perforation with bleeding into the abdominal cavity or gastrointestinal tract cavities.
Because of these differences, the subsequent course of the disease after perforation, its symptoms and consequences can vary greatly. So, if the discharge from a perforated ulcer enters the abdominal region, then the course of the disease and symptoms become extremely atypical. With covered perforations, pain can either disappear or take on a form characteristic of another disease.
According to the location of the perforated ulcer:
- Stomach.
- Duodenum.
- Pyloroduodenal zone (zone of transition of the stomach to the duodenum).
- The location of the ulcer in the stomach and duodenum at the same time (combined ulcer)
In up to 85% of cases, the anterior wall of the duodenal bulb is perforated. Against this background, gastric perforation occurs much less frequently. At the same time, in young people, perforation of ulcers of the duodenal zone (duodenum) is more common, and in older people, perforation of gastric ulcers predominates.
Diet before and after surgery
Proper nutrition is an integral element of the treatment of any pathology of the gastrointestinal tract. When diagnosing a perforation, you should be especially careful, since the recommendations relate not only to the recovery period, but also to the time before the operation itself.
Before excision of an ulcer or resection of the stomach, you must completely abstain from food. The human gastrointestinal tract should be empty at the time of surgery. Only in this case will the specialist perform the operation as efficiently as possible, which reduces the risk of complications.
You should also refuse food for several days after the procedure. This requirement must be observed to quickly restore the entire gastrointestinal tract. For the same reason, treatment after surgery involves a gentle diet.
4-5 days after the perforation is eliminated, liquid dishes and drinks are introduced into the patient’s diet. Such a diet is designed to reduce peristaltic activity, as well as reduce the secretion of digestive enzymes and, accordingly, their activator - hydrochloric acid. The aggressive effect on sensitive mucous membranes will be minimal. An excellent option for a patient after suturing a perforated form of peptic ulcer would be light vegetable soups or broths with lean meat. For drinks, it is best to prefer water or jelly. This diet must be followed for at least 5 days, after which the menu is expanded to include:
- vegetable purees;
- steam omelettes;
- rice porridge;
- dietary meat cutlets.
The attending physician will warn that diet is an effective tool for restoring the normal functioning of the gastrointestinal tract, so it is necessary to strictly follow nutritional recommendations.
Most of the usual products remain prohibited not only during the rehabilitation period after excision of the perforation, but throughout life. To avoid relapses of peptic ulcers, a person is forced to adhere to a special diet that excludes the use of:
- fatty meat;
- smoked meats;
- spices;
- vinegar;
- sauces;
- canned food;
- Luke;
- garlic;
- sour vegetables and fruits;
- coffee;
- carbonated drinks;
- alcohol.
Nutrition for perforated ulcers is designed to ensure minimal load on the gastrointestinal tract by reducing the time food remains in the stomach cavity and reducing the concentration of hydrochloric acid, which corrodes the walls of the organ.
Possible complications and prognosis
A perforated stomach ulcer is a serious condition in which a person suffers from severe pain. Many people are interested in whether surgery is necessary if examination shows damage to the muscle walls. Gastroenterologists answer that without urgent surgical intervention, the chances of recovery are minimal. Inflammation quickly spreads throughout the abdominal cavity, which can lead to purulent peritonitis. It is this pathology that ultimately leads to death, observed in 5% of all registered cases.
Complications after surgery are rarely recorded. They may be associated with poor-quality suturing, which provokes an abscess or sepsis in the abdominal cavity. Sometimes there is a recurrence of perforation, which forces specialists to perform the excision procedure again.
Any form of peptic ulcer is dangerous to health, so measures should be taken at the first symptoms. Treatment without surgery is possible if the muscle layer is not damaged. In this case, the doctor will select medications that will prevent further destruction. Medicines will be prescribed that affect the causes of pathology – pathogens. If the disease continues to progress, then it is not advisable to treat it with medication. In case of perforation, urgent surgery and subsequent diet are required.
Symptoms during typical development of the disease
The first period is pain shock (chemical peritonitis)
Depending on the intensity of the leakage of gastroduodenal contents into the abdominal cavity, the first period can last from 3 to 6 hours. This depends on the diameter and location of the perforation, the degree of filling of the gastrointestinal tract with food.
Thus, peritonitis usually develops more rapidly when the anterior wall of the stomach is perforated. In some cases of perforation of the duodenum, extensive peritonitis can develop with a significant delay.
At the first stage after perforation, a complex of symptoms of an “acute abdomen” develops, caused by serious damage to the internal organs.
The first obvious symptom of perforation is severe “dagger” pain in the epigastric region (Dieulafoy’s symptom). Pain occurs due to chemical burns of internal organs and tissues by hydrochloric acid of digestive juice. The patients themselves call it unbearable.
First, the pain is felt in the stomach area. Then it descends along the right or, less often, along the left side and then covers the entire volume of the abdomen.
Unbearable pain intensifies with any movement. Therefore, the patient tries not to move. He usually lies on his side, often on the right, and presses his legs bent at the knees to his chest with force.
A characteristic symptom of a pronounced “board-shaped” abdomen occurs - strong constant tension in the muscles of the anterior abdominal wall. The abdomen is slightly retracted, the patient tries not to use it when breathing, and does not allow doctors to touch it.
When duodenal ulcers are perforated, a pain symptom may appear around the navel and right hypochondrium. Pain can radiate to other organs and parts of the body. Thus, pain during pyloroduodenal perforations can be felt in the right scapula and clavicle, or in the left - during perforation of the body of the stomach (Eleker's symptom).
A clear symptom of perforation of an ulcer is the presence of gas in the abdominal cavity, which enters it, like food masses, through the resulting hole. The presence of gas is judged by the disappearance of hepatic dullness, which is determined using percussion (tapping the surface of the abdomen) by a characteristic sound. Gas is most often concentrated under the right dome of the diaphragm, and, depending on the position of the body, it can also be localized in other places in the free abdominal cavity.
Perforation is accompanied by the following symptoms:
- slowing of the pulse immediately after perforation (Grekov's symptom);
- shallow, rapid, intermittent breathing;
- the face is constantly tense, sunken eyes;
- pallor, cold sweat, cold extremities;
- blood pressure is reduced.
Vomiting during perforation is not typical. However, in 20% there is a single vomiting immediately before perforation.
A characteristic symptom of acute peritonitis during perforation is the Shchetkin-Blumberg symptom, determined by palpation. To do this, the doctor carefully applies shallow pressure with his fingers on the stomach and after a few seconds sharply removes his hand. In the presence of peritonitis, such actions will sharply increase the pain.
The Shchetkin-Blumberg symptom with obvious abdominal tension can not be checked. But in older people, overweight people, and those who are intoxicated, such a sign of a perforated ulcer as tension in the abdominal muscles may be absent or weakly manifested. In this case, the Shchetkin-Blumberg symptom becomes an important indicator for diagnosing the patient.
Second period – imaginary well-being
The period of false well-being is characterized by a weakening of acute symptoms and lasts about 8-12 hours. The name comes from the patient’s false feeling that the disease has subsided.
This period is characterized by the following features:
- The pain weakens or disappears completely.
- Tension of the abdominal muscles weakens, breathing with the participation of the abdomen is restored.
- The patient's behavior reveals a state of euphoria - a characteristic state after suffering severe physical pain.
The pain disappears as a result of neutralization of hydrochloric acid of gastric juice by abdominal exudate (liquid released into the abdominal cavity from small blood vessels during inflammation) and weakening of the sensitivity of nerve endings. Patients perceive this as an improvement in their condition.
Taking painkillers makes the period of false well-being more pronounced.
However, the condition continues to worsen. The following symptoms indicate the continued development of intoxication:
- temperature increase;
- dry mouth, gray coating on the tongue;
- a rapid increase in the number of leukocytes in the blood;
- increased heart rate, possible development of arrhythmia;
- signs of gas in the abdominal cavity become more distinct;
- the appearance of fluid in the abdominal cavity;
- development of flatulence (accumulation of gases in the intestines) due to the development of intestinal paresis (partial or complete cessation of food movement in the intestines).
Despite a significant reduction in pain, involuntary tension of the abdominal muscles is observed, and the Shchetkin-Blumberg symptom also remains positive.
Thus, during a period of false well-being, the disease continues to consistently develop rapidly, but with a temporary weakening or disappearance of pain, which misleads the patient.
Third period – sharp deterioration (development of acute peritonitis)
After the second, latent period of the disease, a sharp deterioration in the condition occurs:
- Nausea and severe vomiting are the first sign.
- Dehydration: the skin and mucous membranes become dry.
- Diuresis (the volume of urine produced) is significantly reduced, up to anuria (cessation of urine flow into the bladder).
- Abdominal tension persists.
- Breathing again becomes shallow and frequent.
- The volume of the abdomen is increased due to accumulated gas and fluid.
- The temperature rises sharply to 38-40 °C with a further drop to 36.6 °C and below.
- The pulse increases to 100-120 beats, blood pressure decreases significantly.
- The oral cavity is very dry, there is a coating on the tongue in the form of a cracked crust.
- The patient becomes lethargic, lethargic, and restless.
A characteristic sign of diffuse peritonitis and exhaustion “The Face of Hippocrates”:
- blank expression;
- drooping lower jaw;
- cloudy, sunken eyes;
- sunken cheeks, pointed nose;
- sunken temples, tight, dry forehead;
- the skin is pale gray, covered with fine cold sweat.
Systemic inflammatory response syndrome appears. Abdominal bloating occurs due to progressive intestinal paresis. Leukocytosis progresses. The content of hemoglobin and red blood cells in the blood increases. Hyperkalemia develops (an increase in potassium in the blood, which plays an important role in the contraction of the body’s muscles, including the heart). And other disorders of the body.
Symptoms of gastric perforation
During gastric perforation, three stages are distinguished: shock, false well-being and peritonitis.
The period of pain shock has the following clinical symptoms:
- suddenly there is an extremely strong, severe, “dagger” pain in the abdomen. This pain occurs when the ulcer perforates and the contents of the stomach or duodenum enter the abdominal cavity. In the first hours, the pain is localized in the upper abdomen, but then spreads along the right (usually) or left flank of the abdomen. Subsequently, the pain becomes diffuse throughout the abdomen. When tapping the stomach, turning in bed, coughing, the pain increases sharply;
- at the moment of pain and as the clinical picture of perforation further develops, the patient takes a forced position - on the back or on the side with the legs brought to the stomach;
- the most important symptom appears - “board-shaped” (sharply expressed) tension of the anterior abdominal wall, initially in the upper half of the abdomen, later the tension becomes widespread. The abdomen is somewhat retracted and does not participate in breathing. According to the figurative expression of G. Mondor, “tension of the muscles of the anterior abdominal wall is a super sign of all abdominal catastrophes. Tension of the abdominal muscles is a reflex and is associated with irritation of the peritoneum”;
- The Shchetkin-Blumberg symptom is characteristic, which is checked as follows. Using the fingers of your right hand, carefully and shallowly press the anterior abdominal wall, wait 3-5 seconds, and then quickly remove your hand. This technique causes a slight concussion of the peritoneum, and in the presence of peritonitis, when the hand is quickly removed, the pain increases sharply. The Shchetkin-Blumberg symptom is extremely characteristic of acute inflammation of the peritoneum. It should be noted that if there is severe tension in the anterior abdominal wall, it is not necessary to check this symptom. However, this symptom acquires great diagnostic significance in the case when the cardinal sign of a perforated ulcer—tension of the abdominal muscles—is absent or very weakly expressed. This happens in the elderly and people with severe obesity and excessive fat deposition in the abdominal area;
- Percussion of the upper abdomen reveals Jaubert's symptom - tympanitis over the liver area. This is due to the accumulation of gas (coming from the stomach) under the right dome of the diaphragm, which is confirmed by fluoroscopy and radiography of the abdominal cavity;
- a positive phrenicus symptom can be detected - severe pain when pressing between the legs of the m. sternocleidomastoideus (usually on the right) due to irritation of the phrenic nerve;
- the patient's face is pale with an ashen-cyanotic tint, perspiration on the forehead; hands and feet are cold;
- approximately 20% of patients experience one-time vomiting. It should be emphasized that vomiting is an uncommon sign of a perforated ulcer;
- pulse is rare, bradycardia is reflex;
- breathing is shallow, intermittent, rapid.
A period of imaginary (false) well-being develops several hours after the moment of perforation. It is characterized by the following symptoms:
- abdominal pain decreases (due to paralysis of nerve endings) and may even disappear, which is perceived by the patient as a significant improvement in condition;
- a state of euphoria of varying severity appears;
- objective signs of trouble in the abdominal cavity remain - tension in the anterior abdominal wall (in some patients this sign may decrease); positive Shchetkin-Blumberg symptom; reduction or disappearance of hepatic dullness; intestinal paresis develops, which is manifested by flatulence and the disappearance of intestinal peristaltic sounds in the abdomen);
- dry tongue and lips;
- bradycardia gives way to tachycardia, palpation of the pulse reveals poor filling, often arrhythmias;
- blood pressure decreases, heart sounds are muffled.
The period of apparent well-being lasts about 8-12 hours and is replaced by peritonitis.
Peritonitis is the third stage of a typical perforation of a gastric or duodenal ulcer into the free abdominal cavity. Peritonitis is severe and is characterized by the following symptoms:
- thirst; vomiting is possible;
- the patient is lethargic; in the terminal stage of peritonitis, loss of consciousness is possible;
- skin is moist, sticky, sallow in color; body temperature is high;
- facial features become sharper, eyes are sunken (“Hippocrates’ face”);
- the tongue is very dry, rough (like a “brush”), lips are dry, cracked;
- the abdomen still remains sharply tense upon palpation; in sloping areas of the abdomen, dullness of percussion sound is determined; intestinal paresis develops, which is manifested by bloating and a sharp weakening and then disappearance of peristaltic sounds during auscultation of the abdomen; pain with advanced peritonitis can significantly weaken;
- the pulse is frequent, weakly filled, may be thread-like, arrhythmic, blood pressure is significantly reduced, in the terminal stage of peritonitis collapse may develop;
- breathing is shallow, frequent;
- diuresis decreases significantly, up to anuria.
With the development of an atypical form of the disease, perforation of the stomach into the retroperitoneal tissue is possible, and the hole can also be covered by surrounding organs, food in the stomach cavity; it is possible to limit the process in the presence of a large number of adhesions. Covering the perforation can be short-term, long-term or permanent. Such forms of gastric perforation can be much easier, and even self-healing is possible. In addition to peritonitis, sepsis, shock, and hypovolemia can complicate the course of gastric perforation.
Covered perforation: symptoms and development of the disease
The covered form occurs, according to various sources, in 2-12% of all cases of perforation of ulcers. It occurs when the perforated hole is closed by a neighboring organ or omentum (fold of the peritoneum). This phenomenon is possible under the following conditions:
- small diameter of the perforation hole;
- a small amount of food mass in the stomach during perforation;
- close proximity to the liver, intestines, omentum, gall bladder.
The clinical development of a covered perforation is similar to a typical case of perforation of an ulcer. Divided into 3 stages:
- perforation of the ulcer, with pain;
- dulling of symptoms;
- development of peritonitis.
First stage. Due to the leakage of gastroduodenal contents into the abdominal cavity, severe pain suddenly occurs in the epigastric region. This is accompanied by:
- sudden weakness, cold extremities;
- decreased blood pressure, poor blood supply to organs;
- pale skin, cold sweat.
The abdomen is tense, usually locally in the area of the source of pain. The Shchetkin-Blumberg symptom is positive.
Second phase. Painful symptoms begin to subside after covering the perforation, as a result of which the flow of food masses is stopped, and also due to the neutralization of hydrochloric acid with exudate. This is usually observed 30-60 minutes after perforation.
The presence of the disease is indicated by symptoms such as:
- temperature increase;
- development of leukocytosis;
- the presence of a small amount of gas under the diaphragm;
- signs of peritoneal irritation and more.
If the perforation is covered reliably enough, and the volume of leaked mass from the stomach or duodenum is insignificant, then with appropriate treatment recovery is possible. But often the cover turns out to be temporary.
The third stage is characterized by the development of complications. These are limited abscesses (purulent inflammation of tissue) in the area of perforation. In the case of intense release of gastroduodenal contents, diffuse (diffusion) peritonitis develops.
Sometimes symptoms with covered perforation are mistakenly regarded as a normal exacerbation of the disease.
Symptoms appear more slowly if the perforation is obscured by the lesser omentum. In this case, the patient experiences intense pain. There are signs of formation of an abscess of the lesser omentum. Using ultrasound, a limited area of inflammatory infiltrate (accumulation of cell elements mixed with blood and lymph) is detected.
Covered perforation of the ulcer
Covered is a perforation in which the perforation, after a certain amount of gastric contents has flowed into the abdominal cavity, is most often covered by the omentum or the wall of another organ (liver, intestine). Covered perforation of a gastric ulcer occurs in 2-15% of all perforations. Covering the perforation is possible only if the following conditions are met:
- small diameter of the perforation hole;
- slight filling of the stomach at the time of perforation;
- the proximity of the perforated hole to the liver, omentum, intestines, and gall bladder.
In the clinical picture of a covered perforation, three phases are distinguished: perforation of the ulcer, subsidence of clinical symptoms, and a phase of complications.
The first phase - perforation of the ulcer - begins suddenly, with intense (“dagger”) pain in the epigastrium, which may also be accompanied by collapse. Tension of the muscles of the anterior abdominal wall develops, but it is usually of a local nature (in the epigastrium or in the upper half of the abdomen).
Then the second phase develops - the subsidence of clinical symptoms. The perforation hole is covered, the acute phenomena of the first phase subside, pain and tension in the muscles of the anterior abdominal wall decrease. However, in many patients in this phase the pain syndrome may persist, although its intensity is significantly weakened. Characteristic is the absence of free gas in the abdominal cavity.
In the third phase, complications develop - limited abscesses of the abdominal cavity, and sometimes diffuse peritonitis.
In some cases, covered perforation is not diagnosed, but is taken for a normal exacerbation of a peptic ulcer.
When an ulcer perforates between the layers of the lesser omentum, clinical symptoms develop slowly, the pain is quite intense, a clinical picture of a forming abscess of the lesser omentum appears - local pain intensifies again, a limited inflammatory infiltrate is palpated (in the projection of the covered perforation). The infiltrate is detected by ultrasound examination of the abdominal cavity.
Atypical development of the disease
Atypical development occurs rarely, about 5% of cases. This course is not due to the direct entry of gastroduodenal contents into the abdominal cavity through a perforated opening, but into limited spaces.
Atypical development of the disease occurs when ulcers perforate:
- cardia of the stomach;
- the posterior wall of the stomach when food masses enter the omental cavity;
- posterior wall of the duodenum, etc.
The disease also makes the disease mild when the perforation leaks into closed areas formed by adhesive processes. And in some other cases.
The atypical course of the disease is characterized by the absence of pronounced symptoms of a typical perforation: the absence of “dagger” pain, a “board-shaped” abdomen, and the rapid development of peritonitis.
Patients may feel aching pain without clear localization. Body temperature rises and weakness is felt.
If the symptoms of atypical perforation are not identified in a timely manner, the disease will be complicated by purulent inflammation of the space where gastroduodenal contents accumulate: the omental cavity, the abdominal space, etc. If the accumulated masses break into the free abdominal cavity, peritonitis will develop.
It is difficult to diagnose the disease in a timely manner. Identification of an atypical form of development of perforation may be difficult due to the following:
- liver dullness remains normal;
- absence of free fluid and gas in the abdominal cavity.
Perforation of the cardial part of the stomach can cause subcutaneous emphysema (accumulation of gas) in the left supraclavicular region (Podlag's symptom), and perforation of the posterior wall of the duodenum can cause emphysema in the navel area (Vigiatso's symptom).
The leakage of gastroduodenal contents into the abdominal tissue causes sharp pain in the epigastric region, radiating to the back. Then the pain subsides. Within 48 hours, phlegmon develops (acute diffuse purulent inflammation), causing fever and chills. On the right, at the level of the thoracic vertebrae, a swelling occurs, upon palpation of which a characteristic crunching sound (crepitus) occurs. X-ray examination reveals gas - the most important symptom indicating perforation.
About 12% of cases of ulcer perforation are accompanied by bleeding, sometimes intense. This is due to perforation of the duodenum in the area of the head of the pancreas. If there is reflux (the release of duodenal contents back into the stomach), vomiting of blood is possible. Bleeding makes diagnosis difficult. Pain, symptoms of peritonitis, abdominal tension are mild or absent. This also causes late detection of the disease.
If the symptoms are not obvious, the presence of a perforation can only be detected by a comprehensive examination: ultrasound, x-ray, or FGDS procedure. In doubtful cases, laparotomy is used.
Endoscopic examination
If it was not possible to clearly diagnose the presence of a perforated ulcer during fluoroscopy and ultrasound, then they resort to a more accurate endoscopic method of examination.
Diagnostic measures to identify a perforated ulcer are carried out using endoscopy. This abbreviation means esophagogastrofibroduodenoscopy, the abbreviated version is fibrogastroscopy. The name comes from the Latin words meaning the esophagus, stomach, duodenum, their fibers and the method of examination.
This diagnostic method consists of examining the gastrointestinal tract cavities from the inside by inserting a gastroscope probe through the mouth and esophagus into the stomach cavity. Thanks to a miniature camera, visual examination of the gastrointestinal tract cavity becomes possible. In this way, the exact location of the ulcer can be determined.
During the insertion of the probe, a fairly large volume of air enters the stomach. In the case of a perforated ulcer, this can cause increased pain due to the entry of this air into the stomach and further through the perforated hole into the abdominal space, which also indicates the presence of a perforation. After which, the presence of gas is detected by repeated x-ray examination.
Perforation of the intestine from below, behind
Duodenal contents infect the retroperitoneal tissue. The main symptom is unexpected, sharp pain in the pit of the stomach that radiates to the back. Over time, the pain subsides. An acute inflammatory purulent process develops in the retroperitoneal tissue of the retroperitoneum. The period is characterized by the development of fever with chills. A swelling forms at the 10-12 thoracic vertebrae, which hurts on palpation. When listening to its area, you can hear a characteristic crunching sound - crepitus. X-ray shows increased gas formation in this area.
Diagnostics
- Blood test. Leukocytosis with a shift of equality to the left, increased ESR, and granularity of neutrophils are detected.
- Urine examination. An excess of protein content is detected.
- Biochemistry. There is an excess of bilirubin, globulin, alanine aminotransferase, and urea.
- ECG. Dystrophic diffuse changes in the myocardium and arrhythmia are detected.
- X-ray of the peritoneum. Increased crescent-shaped gas formation on the right under the diaphragm is detected.
- Ultrasound. An inflammatory infiltrate is detected.
Principles of treatment
For such an acute disease as a perforated gastric ulcer, treatment should be surgical. Conservative treatment is used only in extreme cases.
At the prehospital stage, if perforation of a duodenal ulcer is suspected, the primary task is to hospitalize the patient in a surgical hospital.
If the patient is in an extremely serious condition, infusion therapy is urgently prescribed and oxygen inhalations are given. The patient should not be given analgesics, especially narcotics - they can blur the picture of the disease and confuse doctors.
Surgery
To treat perforation of a duodenal ulcer, laparotomy is performed. The operation is performed under general anesthesia. A longitudinal incision is made into the muscles of the abdominal wall. When the layers of the peritoneum are dissected, a small amount of air with a characteristic sound may escape from the cavity. A certain amount of greenish turbid fluid is found in the abdominal cavity. The exudate is removed from the cavity using electric suction.
On the wall of the duodenum you can find an infiltrated white area with a diameter of up to 3 centimeters. In the center of the infiltrate you can find a small round hole with a diameter of up to 0.5 cm with smooth edges. If there is a pronounced adhesive process in the abdominal cavity, searching for the site of perforation becomes very difficult. If a visual assessment of the surgical site is not possible, the surgeon performs a digital assessment of the duodenum and locates the site of perforation.
Operation method
The method of surgical intervention is selected by the surgeon depending on the location and size of the perforation, age and general condition of the patient. The presence and severity of peritonitis and the presence of concomitant diseases are taken into account. In most cases, we are talking about suturing a perforated ulcer.
Suturing the ulcer
Indications for suturing a perforated ulcer are diffuse peritonitis, a high degree of risk during surgery, and the presence of a stress ulcer in a young man without a long history of ulcers.
In young people, suturing the ulcer and carrying out a postoperative course of treatment leads to the fact that the ulcer heals well and does not recur. The prognosis is favorable, the relapse rate is minimal. In elderly patients, ulcers are often prone to malignancy, and gastric resection is advisable.
The duodenal ulcer is sutured with a single-row suture in the transverse direction, without involving the mucous membrane. This suturing method will prevent intestinal stenosis. If the tissues of the duodenum are loose and cut through during suturing, the adjacent sheets of the omentum or ligament are used.
Symptoms and signs
A perforated gastric ulcer is a dangerous condition that threatens not only the health, but also the life of the patient, so it is important to know by what signs this pathology is diagnosed and what is done to successfully treat it. One of the diagnostic methods is MRI of the stomach. Experts list several symptoms indicating that a person is suffering from a perforated ulcer:
1. Pain. If in the early stages of the pathology, when the size of the damage is minimal, there may be no discomfort, then a perforated ulcer is always accompanied by unpleasant sensations. Moreover, they are localized in the central part of the abdomen and are cutting or stabbing in nature.
2. Metallic taste in the mouth. This sign indicates the presence of bleeding. The symptom is associated with the content of hemoglobin, which is an iron compound, in this biological fluid.
3. Heartburn and burning sensation. These symptoms of a perforated ulcer are characteristic of the early stages of the disease, but if the muscular layer of the stomach is damaged, they become unbearable.
4. Nausea. Vomiting is also characteristic of the initial stages of gastric ulcer. This is a kind of defense of the human body, since intense secretion of hydrochloric acid, which destroys the walls of the gastrointestinal tract, begins after the intake of food.
5. Increased body temperature. Particular attention should be paid to this sign, since its cause is usually the spread of inflammation throughout the entire cavity of the stomach and its exit beyond the organ.
6. Pale skin. Anemia is typical for patients diagnosed with internal bleeding due to a perforated ulcer. This is due to a strong drop in the level of hemoglobin, a complex responsible for saturating all organs and tissues with oxygen.
Stomach ulcers are a dangerous condition that can sometimes lead to death. For this reason, when characteristic symptoms develop, it is necessary to urgently take measures aimed at treatment. Cases of death of patients with this pathology are associated with the fact that at a certain stage all unpleasant symptoms weaken. The person’s well-being improves, and he often refuses medical care. Doing this is prohibited, because the absence of discomfort is provoked only by the destruction of the nerve receptors responsible for the perception of pain. Within a few hours the situation will change dramatically, and the patient will begin to suffer from fever, weakness, fever and gastrointestinal upset.
Urgent Care
Every person should know that the best solution if you suspect a perforated ulcer is to consult a specialist. The patient is immediately hospitalized and further treatment is carried out under the strict supervision of doctors. However, first aid to the victim must be provided even before the ambulance arrives.
Until doctors arrive, it is important to ensure that the person suffering from a perforated ulcer is completely rested. It is better if he takes a horizontal or semi-sitting position. This will help you maintain your strength.
Experts warn that you should not take any medications until doctors arrive. Any analgesics are extremely undesirable due to their effect on receptors. The pain of a stomach ulcer is intense, so it is difficult to get rid of it at home. A tablet of Baralgin or any of its analogues based on metamizole sodium can dull the discomfort, but this will distort the overall clinical picture. As a result, diagnosing the pathology becomes difficult, and treatment begins only when the doctor is completely sure that the patient has a perforated ulcer.
Treatment at the prehospital stage involves maintaining all vital functions of the body. If the condition is severe, then you need to monitor your blood pressure, which often decreases. After hospitalization, the doctor will assess the patient’s well-being and determine further treatment tactics. The perforated form of the disease requires surgery. It is impossible to cure it with conservative methods.
Treatment methods
A perforated ulcer is the formation of a through hole in one of the sections of the gastric wall. Taking medications will not help treat the pathology. The tablets are intended to only partially alleviate its symptoms, but it is possible to restore the integrity of the mucous membranes and muscle layer only during surgery.
There are 2 options for surgical intervention that is designed to cure the disease. If the size of the hole is small, then during the operation only the damaged fragment of the wall is excised, and then the free edges are sutured. If this is not possible, then the surgeon decides to remove the part of the stomach that has undergone pathological changes. Experts call this type of operation resection. This method has several advantages, primarily related to the low likelihood of relapse. If during the manipulation the ulcer is excised directly, then there remains a chance of a secondary perforation in the same area.
Regardless of the method, surgery is always performed under general anesthesia and with artificial ventilation. This means that the early postoperative period begins, requiring special attention to the patient. If necessary, the attending physician will select safe non-narcotic analgesics designed to reduce the intensity of pain after removal of a stomach ulcer.
Postoperative period
In the postoperative period, the patient is prescribed a strict diet. In order for the body to fully recover, it is necessary to follow all the instructions of the attending physician. Dietary nutrition must be followed for at least 4 months. The diet may gradually become more complex.
When following a diet, you must adhere to the following rules:
- Meals should include at least 5 meals per day. Portions should be small.
- All foods included in the diet must be liquid or pureed.
- It is better to cook food by steaming or boiling.
- It is imperative to reduce the amount of salt consumed to a minimum.
- It is better to completely exclude simple carbohydrates (chocolate and other sweets) from the diet.
2 days after the operation, you can include mineral water without gases, weak tea and fruit jelly in your diet.
After 3 days, the diet allows a decoction of rose hips, pureed soups or porridges. In addition, you can eat boiled eggs, pureed cottage cheese and pureed vegetable soups.
On the tenth day after surgery, the diet consists of boiled vegetables, steamed cutlets, lean meats and boiled fish. You can include cheesecakes and cottage cheese casseroles in your diet. Cottage cheese and other fresh dairy products are allowed to be consumed in small quantities.
After 1 month, flour products such as dryers and crackers are allowed on the diet. After 2 months, you can eat fresh sour cream and fermented milk products (kefir, yogurt).
As you recover, the diet becomes less strict, but all canned, smoked foods and dishes with a lot of spices are prohibited.
Consequences and possible complications
In the absence of timely treatment or violation of medical instructions, the following complications of peptic ulcer disease may develop:
- Stenosis is a narrowing of the pylorus (the area between the stomach and duodenum). This complicates the movement of food through the digestive tract, which provokes its accumulation in the stomach cavity. As a result, the person suffers from constant nausea and vomiting. The main symptoms of this phenomenon are loss of appetite, a feeling of heaviness in the abdomen (especially in the upper part), bloating and heartburn. As the pathological process progresses, the patient begins to lose weight, and the amount of vitamins and macroelements in the body decreases. The problem can only be eliminated through surgery. Conservative treatment brings the desired effect only in very rare cases.
- Bleeding is the most common and dangerous complication of perforation of a duodenal ulcer, the symptoms of which most often appear in advanced forms of the disease at a young age. The main signs are blood inclusions in the stool. As a result, not only significant blood loss occurs, but also the penetration of pathogenic microorganisms into the circulatory system.
- Malignization is the degeneration of affected cells into malignant neoplasms. The main symptom of this complication is severe pain in the abdominal area, which appears regardless of food intake. In most cases, this pathological process develops in elderly patients, but it is quite difficult to identify. Most often, complex therapy is used to treat the disease, including surgery and the use of medications.
- Penetration is one of the most dangerous forms of complications of peptic ulcer disease. The main danger is that the lesion can affect not only the stomach or duodenum, but also other internal organs. To eliminate a pathological process of this nature, urgent surgical intervention is required.
It should be remembered that even after successful treatment of the disease, a serious complication can develop. Therefore, it is very important in the postoperative period to follow all the doctor’s instructions (diet, proper nutrition, taking certain medications). This will help completely restore the body and prevent relapses.
Causes
The formation of a hole in the wall of the stomach is associated primarily with a complication of a previously existing problem - a chronic or acute ulcer. Perforation occurs when the layers of tissue that make up the stomach wall are completely separated. Sometimes the cause of the development of this pathological condition is the actions of the patient himself. This is ignoring doctor's orders and violating the established diet.
The causes of a neglected stomach condition and exacerbation of an existing ulcer are:
- Strengthening the aggressive influence on an already damaged area of the organ wall. An increase in acidity directly affects the rate of hole formation.
- A sudden jump in intra-abdominal pressure can occur with severe stress.
- Ignoring dietary instructions: drinking alcohol, prohibited foods, salty foods.
- State of chemical poisoning.
- Due to the negative effects of non-steroidal anti-inflammatory drugs.
- A state of strong emotional tension.
- Heredity, cases of a similar disease in the family history.
- Additional infection with the bacterial microorganism Helicobacter pylori.
- State of overeating.
- Performing complex physical exercises with phases of strong tension.
The impact of the above negative factors is a prerequisite for initial damage to the walls of the gastrointestinal tract, which subsequently develops into more severe forms.
Problems with complications of peptic ulcer disease are found in 10% of cases with any gastrointestinal tract diseases. The most common age group for those suffering from this disease is 20-50 years. In addition, men are more susceptible to this complication, since the presence of estrogen in women acts as a powerful limiter on the level of acidity of gastric secretions.
If the integrity of the wall of the stomach or the lower part of the gastrointestinal tract is violated, secretions enter the abdominal cavity. Particles of consumed foods, microorganisms, large quantities of gastric juice and a little bile leak through the through hole. The diameter of the breakthrough can reach 5 mm, but does not exceed it.
The consequences of exposure to acidic juice are chemical burns of important organs of the peritoneum. The contact of even a small amount of juice on the surface of any other organ is accompanied by severe pain, which easily puts the patient into a state of painful shock.
Infection of the body with stomach secretions can cause a serious spread of infectious microorganisms. Delaying first aid can lead to serious complications and even death of the patient.
Forecast
Surgery significantly reduces the risk of death due to the disease
99% of deaths occur within the first week of illness in the absence of surgery. Mortality rate is 5-8% during surgery. Postoperative mortality depends on the consequences that occur, the severity of the condition, the age group and underlying diseases of the patient.
The risks of mortality in the postoperative period are summarized in the table.
There is a possibility of death after surgery for peptic ulcer disease.
Prevention
Necessary measures to prevent ulcer perforation:
- maintaining a proper diet;
- correctly selected diet;
- maintaining a healthy lifestyle;
- quitting smoking, alcohol;
- constant examination by a gastroenterologist.
List of references: https://ru.wikipedia.org/wiki/Perforated_ulcer https://www.mgzt.ru/content/probodnaya-yazva-stereotipy-kotorye-nam-meshayut-0 https://www.10gkb.by /informatsiya/stati/probodnaya-yazva-zheludka-i-12-perstnoj-kishki https://www.aptekar76.ru/bolezni/detail/Probodnaya_yazva_zheludka_i_dvenadcatiperstnoj_kishki/ https://www.mediasphera.ru/issues/khirurgiya-zhurnal- im-ni-pirogova/2015/11/downloads/ru/440023-12072015115 Valdanova M.E., Zhdanova A.V. Perforated ulcer of the stomach and duodenum in patients of the older age group // Smolensk Medical Almanac. 2021. No. 1. https://medi.ru/klinicheskie-rekomendatsii/probodnaya-yazva-u-vzroslykh_14206/ Notes from the author of the article, based on personal experience. This material is purely subjective and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/18/2020