Ultrasound diagnosis of thickening of the stomach walls
Wall thickening can also be detected using x-rays, but ultrasound has several advantages.
The examination allows you to study the organ in different projections, it is safe and does not have a harmful effect on the body. During the examination, the Doctor can see changes in each layer. On ultrasound, the wall looks like a thin line consisting of three layers - hyperechoic inside and hypoechoic on the sides. The mucous membrane has folds that smooth out when the sensor is pressed. Normally, movements (peristalsis) can also be observed.
An increase in thickness occurs due to any of the layers. Thus, with interstitial tumors, changes in the size of the submucosal or muscular layer in a certain area are often detected. An increase in the mucous layer occurs during inflammatory processes and hypertrophy. Also, benign (polyps) and malignant (adenocarcinoma) neoplasms often form in this layer. Doppler examination allows one to differentiate malignant neoplasms, which can detect increased blood flow in this area.
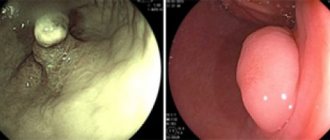
Endoscopic signs of polypoid hyperplastic gastritis
The presence of polyp-like formations on a broad base on the thickened walls. The color above them does not differ from the surrounding mucosa. Sizes from 0.3 to 0.5 cm. Most often multiple, less often single. It can be diffuse and focal. Most often on the anterior and posterior walls of the body, less often on the antrum.
With true polyps, the relief of the mucous membrane is not changed, but with hyperplastic gastritis it is changed due to thickened convoluted folds. For all types of hyperplastic gastritis, targeted biopsy must be used to exclude a malignant process.
[48], [49], [50]
Symptoms
Gastric atrophy has main signs and symptoms that are almost the same in all patients.
Among them:
- nausea;
- aching pain with an uncertain location, which noticeably intensifies after eating;
- copious amounts of saliva;
- frequent belching with a bitter, rotten taste;
- bloating and rumbling in the stomach;
- feeling of heaviness in the stomach;
- an unpleasant white coating on the tongue;
- stool instability, in which constipation is replaced by diarrhea;
- dystrophic syndrome;
- clinic of iron and vitamin D-, B12-, C-deficiency anemia - dizziness, fatigue, shortness of breath, weakness, brittle hair and nails, bleeding gums, pale skin, decreased visual acuity, seizures and pustular skin lesions.
Thickening of the mucosa as a symptom of stomach cancer
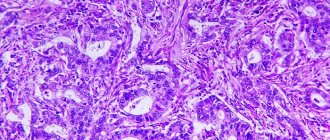
In serious cases, this pathology is a symptom of cancer. A biopsy performed during FGDS will help to accurately establish this fact. The specialist also determines the stage of the disease: stomach cancer develops gradually, at the zero stage there are no symptoms, at the first stage a slight malaise is detected.
The treatment method is determined according to the nature of the disease.
The following drugs are recommended:
- immunoglobulins “recognize” foreign cells and activate natural immunity to fight them;
- Enzyme inhibitors penetrate into cancer cells, destroying them from the inside.
Radiation and chemotherapy are also used. In critical situations, surgical treatment is recommended: the walls of the stomach or the entire organ are excised.
To reduce harm to the body, you need to seek treatment immediately after detecting a pathology.
Thickening of the stomach wall occurs from oncology of the digestive system, Ménétrier's disease, and infectious lesions. It comes in two types: limited and widespread. If the wall thickness is not within 50-60 mm, then there is pathology in the gastrointestinal tract. Ultrasound and endoscopic ultrasound (EUS), which gives the most accurate results, will help determine the exact picture. According to it, doctors prescribe individual treatment.
EUS for thickening of the stomach
The main diagnostic method is endoscopic ultrasound. It involves the use of an echoendoscope, at the end of which there is a miniature sensor and a special optical device that allow you to carefully study the relief of the stomach. Modern equipment has a high resolution, up to 1 mm. Such accuracy is not available with other methods. The effectiveness of the examination is also guaranteed by the use of high-frequency ultrasound, which penetrates into the deepest layers of the mucosa.
Fibrogastroduodenoscopy
This type of endoscopic examination is another one of the most popular. It allows the doctor to visually examine the walls of the stomach and identify possible pathologies. To carry out the procedure, a special device is used - a gastroscope. It consists of a tube with a diameter of 8-11 mm and a length of approximately 100 cm. The front tip is movable and can rotate 180 degrees. There is also a light and camera for easy inspection.
The probe is used not only for visual diagnosis, but also for biopsy. Microscopic forceps are inserted through the probe to help remove the material.
This procedure is performed if there is a suspicion that the thickening of the walls is associated with cancer. The advantage of fibrogastroduodenoscopy is that it is targeted, and only the area of interest to the specialist can be affected. The removed sample is sent for diagnostics, during which the exact cause of the pathology is determined.
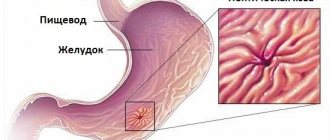
Endoscopic signs of rigid antral gastritis
The outlet section of the stomach is affected in isolation, which, due to hypertrophic changes, edema and spastic contractions of the muscles, is deformed, turning into a narrow tube-like canal with dense walls. This lesion is based on a chronic inflammatory process that affects all layers of the stomach wall, including the serous one. Characterized by persistent dyspepsia and achlorhydria. An endoscopic examination reveals a narrowing of the antrum, its cavity looks like a tube, does not expand with air at all, and peristalsis is sharply weakened. The mucous membrane is sharply edematous, swollen, with areas of severe hyperemia and deposits of mucus. As the disease progresses, motor-evacuation activity is impaired (a sharp weakening of peristalsis), sclerosis of the submucosal and muscular layers develops, and a persistent rigid deformity develops with a significant shortening of the antrum of the stomach.
[55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65]
Anatomy
The stomach in the human body is the primary organ of the digestive system. It is located between the esophagus and the small intestine, or rather the duodenum.
The organ consists of several parts:
- The cardinal section is the uppermost part. Here the transition from the esophagus to the stomach itself takes place.
- The more convex part is the arch or bottom.
- The continuation of the vault is the body of the stomach. It is divided into greater and lesser curvature.
- The final part is the antrum. Here the organ narrows, takes the form of a tube and passes into the duodenum.
Digestion processes take place in any part of the organ, therefore atrophy can form in different parts.
The wall of an organ consists of several layers or membranes. The most superficial is serous, the thickest, serving as a frame and protection for the organ from aggressive influences.
This is followed by the muscle layer, consisting of a number of muscle fibers involved in the processes of digestion and peristalsis
The submucosa serves as a transition to the innermost and most important wall - the mucosa
In the gastric mucosa there are a number of cells that synthesize and secrete various substances; parietal cells produce hydrochloric acid, which is involved in the chemical processing of the bolus.
Endocrine cells secrete the hormone gastrin, which is necessary for normal digestion. Additional elements synthesize mucus; it is a protective component of the mucous membrane from its own hydrochloric acid.
When there is little mucus, damaging self-digestion processes are launched. Chief cells produce the enzyme pepsin.
The gastric mucosa has a number of functions:
- Digestive: produces substances that facilitate all digestive processes.
- Secretory: participates in the release of secretory active compounds.
- Hematopoietic: produces vitamins and blood clotting factors.
Thickness standards
Despite a person’s age and gender, the thickness of the stomach wall is constant. If its size is 50-60 mm over the area of the entire digestive organ, then the compaction indicators are normal. If this figure increases in at least one of the areas, you should look for the causes of the pathology. The thickness of the organ wall does not vary according to various indicators, and an increase in its density above 0.6 cm indicates an abnormal compaction. If the thickening area is more than 3 cm long and the wall changes its relief, this indicates limited thickening. The organ is deformed, the volume decreases, thickening is present virtually throughout the stomach - this is a common compaction.
General information
Thickening of the walls of the stomach is any deviation upward from the above figures.
The area of damage may vary; there are two types of this phenomenon:
- limited: the wall of the organ is thickened in a small area, up to 3 cm long. Often accompanied by a change in the relief of the mucous membrane, its rigidity, deterioration of peristalsis up to complete absence;
- widespread: a significant part of the stomach wall or the entire surface is covered. Associated symptoms: organ deformation, volume reduction, limited displacement, cessation of peristalsis.
The presence of even small thickenings is an alarming sign that requires detailed diagnosis. It is difficult to name the exact cause of their appearance: they are symptoms of a variety of diseases, including cancer, benign or malignant. The exact cause and nature of the disease can be determined after examination and biopsy.
Indications
The procedure is recommended for thickening of the gastric mucosa of various types, including cancer.
However, unlike conventional ultrasound, endoscopic examination has a number of contraindications:
- bleeding disorders;
- general serious condition;
- threat of depression of respiratory and cardiac activity.
Indications for ultrasound examination may include frequent epigastric pain, belching, vomiting, heartburn and flatulence.
Similar symptoms can be caused by diseases such as:
- gastritis;
- erosion, stomach ulcer;
- suspicion of polyps;
- malignant formations (stomach cancer);
- loss of elasticity of the stomach walls (pyloric stenosis);
- obstruction of the intestines or esophagus;
- developmental anomalies (both acquired and congenital).
Human stomach (on the cut all layers of the wall are visible)
The child may be examined (in addition to the listed gastrointestinal symptoms):
- with frequent relapses of bronchitis;
- with frequent regurgitation (infants);
- for asthma, dry cough.
Ultrasound is a diagnostic method at an early stage of detecting a problem; the data obtained serve to determine a further set of diagnostic methods and select further therapy.
How to prepare for an ultrasound of the stomach? Advice for preparing for the study is mandatory, since the accuracy of the test result directly depends on them.
The transabdominal method does not have any contraindications. The endoscopic method is used less frequently, due to a number of prohibitions associated with the introduction of part of the apparatus into the body. EndoUS is prohibited:
- with inflammation (acute or chronic) in the oral cavity or pharynx;
- for burns, injuries of the esophagus;
- with stenosis of the esophagus resulting from the development of scar tissue or a tumor;
- for diseases affecting blood clotting;
- in the presence of mental disorders;
- with aortic aneurysm.
Ultrasound of the stomach is a quick way to initially diagnose diseases of this organ. Based on the information obtained during the examination, the doctor will prescribe clarifying methods for determining the disease, and then select treatment taking into account the individual characteristics of the patient. This method is also indispensable for monitoring the organ during therapy - due to the absence of contraindications, it can be used as often as the situation requires. Preventive examinations using ultrasound allow you to monitor the condition of the stomach and respond in time to negative changes in it.
When a person has complaints of pain in the upper abdomen, heartburn, nausea and vomiting, belching, it is necessary to examine the esophagus and stomach with an ultrasound. This is a simple diagnostic procedure that will help quickly establish a diagnosis.
Indications for ultrasound examination in adults:
- Gastritis.
- Gastroesophageal reflux.
- Stomach ulcer.
- Duodenal ulcer.
- Narrowing of the pylorus (stenosis).
- Suspicion of neoplasms.
- Abnormalities of stomach development.
- Impaired patency.
There are no absolute contraindications to performing transabdominal ultrasound. Relative contraindications are the impossibility of contact with a person due to a mental disorder, damage to the abdominal skin from burns, wounds, or an infectious process.
There are a number of contraindications for endoscopic examination. This is due to the fact that the device is inserted internally and can damage organs. Contraindications to gastroscopy:
- inflammatory process of the oral cavity, pharynx;
- traumatic injuries of the esophagus, including burns;
- narrowing of the lumen of the esophagus;
- aortic aneurysm;
- disorders of the blood coagulation system;
- difficult contact with a person due to mental disorders;
- severe course of bronchial asthma.
Thickening as a symptom of stomach inflammation
With the modern rhythm of life, constant stress and poor nutrition, a large part of the population suffers from digestive disorders.
In addition to the above factors, this disease is also affected by:
- frequent drinking;
- drug use;
- infection;
- taking painkillers from the group of non-steroidal anti-inflammatory drugs (NSAIDs);
- autoimmune infection.
In the latter case, inflammation often occurs against the background of other autoimmune diseases, for example, type I diabetes.
Inflammation is manifested by severe nausea, vomiting, aching pain and heaviness after eating. When these symptoms appear, immediate diagnosis and treatment are required. In the absence of therapy, the disease can provoke a number of complications, one of which is an increase in the walls of the organ, which increases the risk of cancer.
Ménétrier's disease: causes and symptoms
This pathology is sometimes the cause of thickening of the stomach walls. It is quite rare, the etiology has not been fully established. A characteristic sign of Ménétrier's disease is the formation of folds on the mucous membrane, the thickness of which can reach 2-3 cm. The disease is diagnosed after a series of procedures: a blood test, fibrogastroscopy, and sometimes radiography.
Although the exact causes of the disease are unknown, doctors name negative factors that can worsen the pathology:
- errors in nutrition;
- avitaminosis;
- alcoholism;
- infectious diseases.
Also, folds on the walls of the stomach may appear due to a benign formation, anomaly or genetic predisposition. A specific factor is chronic lead intoxication.
Against their background, the following may develop:
- epigastric pain;
- heaviness in the stomach;
- increased pain after eating;
- vomit;
- diarrhea;
- stomach bleeding;
- sudden weight loss of up to 20 kg;
- decreased appetite.
Service cost
You can get a high-quality ultrasound of the stomach at any public or commercial medical institution that provides ultrasound diagnostic services. It is advisable to choose a gastroenterological profile of the institution. The cost of a transabdominal ultrasound starts from 500 rubles, and gastroscopy will cost at least 2,500 rubles.
It is impossible to say which research option is better or worse. Each method has its pros and cons.
Tell us about your familiarity with gastrointestinal tract examinations, how useful they are for diagnosis, whether they are painful or not. Share the article on social networks. Be healthy.
How to treat the disease
https://youtube.com/watch?v=yGI2wDtRP_U
Atrophy can be completely cured only in the earliest stages. Most patients do not even know what form of gastritis they have, so they rarely turn to doctors and diagnose the form of pathology late.
In advanced stages, it is not possible to completely restore damaged glands, since they are replaced by scar connective tissue.
In this case, they resort to drug replacement therapy. In order to properly treat the atrophy processes and restore the gastric mucosa, you must consult a doctor and follow all his recommendations.
The treatment will be complex and consists of the following parts:
- Maintaining a daily routine.
- A careful and strict diet.
- Full course of taking medications.
Diet for atrophy of the gastric mucosa
The diet should be compiled by a gastroenterologist or nutritionist depending on the degree, volume and stage of the process.
Meals should be selected as complete and fractional ones.
The body must receive all the necessary energy and nutrients in sufficient quantities. You need to eat once every three hours, the last meal before bed 2-3 hours.
- All food products must be finely chopped, twisted, and ground to avoid mechanical injury to the stomach wall.
- You need to eat slowly, chewing the pieces thoroughly.
- Dishes should be at optimal room temperature, not hot, but not cold.
What should be included in the diet
Doctors have calculated that patients with this form of pathology need to receive per day:
- About 350-400 grams of carbohydrates.
- Vegetable proteins 50 grams, animal proteins - no more than 100 grams.
- Vegetable fats only, no more than 100 grams.
- Table salt – 10 grams.
- The menu must include fruits, vegetables, and a full supply of multivitamins.
- You should drink 1300-1500 ml of liquid (in total per day).
What should be completely excluded:
- Fatty, smoked, fried, salted.
- Scrambled eggs.
- Beans, peas, beans.
- Spicy seasonings, raw garlic and onions.
- Baking.
- Fast food, seeds, nuts.
- Carbonated drinks, juices, alcohol, coffee.
What is allowed for use:
- Soups cooked without meat and not in fatty broth. Most often these are cream soups.
- Boiled poultry, fish.
- Boiled and stewed vegetables. It is useful to eat potatoes, carrots, zucchini. Best in crushed form.
- Omelettes with milk.
- Porridge from semolina, rice, buckwheat. In the early stages, boil in water.
- Berries, fruits, exclude citrus fruits.
- Cottage cheese, sour cream, low-fat milk.
- Honey, compote, soufflé.
Sample diet for the day:
- Rice porridge for breakfast, chamomile tea, soft-boiled egg.
- For lunch, rice soup without meat, boiled chicken breast, jelly or still mineral water.
- In the afternoon you can eat an apple or light yogurt.
- Dinner - boiled vegetables, fish, casserole, salad of herbs and cucumbers, weak tea.
- A couple of hours before bedtime, cottage cheese, kefir, banana.
Drug treatment
Treatment for atrophy of the gastric mucosa can only be prescribed by a doctor; all dosages, medications and duration of the course are determined only by him, the outcome of therapy, restoration of the mucosa and recovery will depend on this.
Groups of drugs that are used to treat the disease:
- In later stages, replacement therapy is used. It is prescribed to consume natural gastric juice an hour before meals; in case of intolerance, enzymatic drugs are prescribed: Creon, Mezim, Pangrol.
- If the process is not extensive, then agents that stimulate the production of hydrochloric acid by the stomach itself will help. The group of drugs includes: Plantaglucide, relieves the inflammatory process and activates the activity of parietal cells.
- B vitamins, especially B12. Can be taken either orally or intramuscularly.
- Antispasmodics to eliminate severity and pain: Drotaverine, No-shpa, Platifilin.
- Antiemetics: Metoclopramide.
If you follow the diet, daily regimen, drug therapy and all the doctor’s recommendations, the health prognosis is favorable, relapses are rare.
Source
Ménétrier's disease: treatment
Since the pathology affects the digestive tract, the patient must be prescribed a gentle diet. Its main component is protein. It is required to remove fried and spicy foods from the menu, and also not to eat hot or cold foods.
Drug therapy consists of taking:
- enveloping, astringent drugs that protect the walls of the stomach from negative influences;
- drugs to compensate for the deficiency of acid-forming function;
- atropine, which reduces protein loss and improves well-being.
If the disease is severe: with bleeding, severe pain, surgical treatment will be required.
A gastrectomy is performed, that is, removal of the stomach. After this procedure, the patient is constantly monitored by a doctor and visits an FGDS every six months.
Thickening of the gastric mucosa with gastritis
Gastritis is a rather dangerous disease, as it can cause changes in the structure of the stomach and affect the condition of its walls.
As a rule, when gastritis passes into dangerous conditions, the walls of the stomach become deformed, become thicker or thinner, and also have integrity problems over the entire surface. Thickening of the stomach walls with gastritis is a very common phenomenon.
Read the next article about in what cases thin stomach walls occur with gastritis and what to do if the stomach wall is enlarged.
Thickening of the stomach wall with gastritis (hypertrophic gastritis)
Gastritis is a disease of the stomach, characterized by inflammatory processes in the mucous membrane of the organ and its further degenerative changes. This disease can affect people at any age. Acute or chronic course is typical. When an irritating substance enters the stomach, the mucous membrane is damaged and acute gastritis develops.
In most cases, chronic gastritis occurs when the acute course of the disease becomes chronic. It is characterized by the gradual formation of dystrophic changes in the wall of the stomach.
According to the form of damage to the walls of the stomach, gastritis is divided into:
- atrophic gastritis: cellular atrophy is noted in the mucous membrane;
- hypertrophic gastritis: the stomach wall thickens and grows;
- polypous astritis: endoscopic examination reveals polypous growths on the wall.
With hypertrophic gastritis, a significant thickening of the folds of the gastric mucosa appears, between which a large amount of secreted mucus accumulates.
With hypertrophic gastritis, a significant thickening of the folds of the gastric mucosa appears between which a large amount of secreted mucus accumulates
A feature of this gastritis is the formation of multiple cystic processes and adenomas on the gastric mucosa. In this regard, thickening of the folds of the mucous membrane occurs. Protein deficiency gradually develops and the amount of gastric juice secreted decreases. In some cases, the disease leads to hypoproteinemia.
Diagnosis of hypertrophic gastritis includes fluoroscopy, which makes it possible to detect a noticeable increase and deformation of the folds of the gastric mucosa.
Next, gastrophoboscopy is performed with a targeted biopsy, which helps to establish an accurate diagnosis.
The examination results reveal hypertrophy and hyperplasia of the mucosa with an increase in the number of mucus-forming cells and a decrease in digestive cells.
Treatment of hypertrophic gastritis
Nutritionists treat non-severe hypertrophic gastritis with conservative methods - chemical, biological, physical.
They mainly use gentle nutrition with a high content of proteins and vitamins. Compliance with the rules of the diet for hypertrophic gastritis is crucial.
Simple cooking recipes are used. Products must be fresh, carefully processed thermally. The complicated form of hypertrophic gastritis (incessant bleeding, pain, swelling) is eliminated through surgery. The overgrown tissue is removed, and the patient is monitored during the recovery period. Less often, if there is a threat to the patient’s life, a complete or partial “gastrectomy” is used - excision of the stomach.
Gastritis of thin stomach walls (atrophic gastritis)
There are forms of gastritis that, without proper attention, can lead to the degeneration of cells in the walls of the stomach into cancerous tumors. A typical example of this type of disease is atrophic gastritis. So what is atrophic gastritis? This is a chronic disease that can lead to the disappearance of parietal cells of the stomach, a decrease in the secretion of hydrochloric acid, vitamin B12 deficiency and megaloblastic anemia. With atrophic gastritis, the gastric mucosa sharply thins and the glands atrophy.
With atrophic gastritis, the gastric mucosa is the most affected - this is a thin layer of cells covering the organ from the inside. It comes into contact with food and hydrochloric acid, protects other tissues from self-digestion, secreting a thick layer of thick protective mucus. This is a chronic and long-term disease that develops over several decades. But the changes that occur in the gastric wall are often irreversible.
As a result, the stomach turns into a practically non-functioning pouch with very thin walls, into which food enters, but is not properly processed there.
With atrophic gastritis, the gastric mucosa sharply thins and the glands atrophy
Therefore, digestive problems arise - proteins, fats, and many vitamins and minerals are poorly absorbed. Plus, due to the fact that there is almost no acid left in the stomach, dangerous microbes that enter with food are not neutralized. This increases the risk of various intestinal damage, poisoning and diarrhea.
Treatment of atrophic gastritis
First of all, as soon as the doctor finds out the causes of atrophic gastritis, it is necessary to prescribe proper nutrition. Establish a diet that will be beneficial for the body as a whole, but will not negatively affect the functioning of the stomach. The diet is aimed at preventing mechanical trauma to the gastric mucosa, so food should be thoroughly crushed and taken warm.
Fatty meats and fish, meat broths, mushrooms, spices and foods that irritate the lining of the stomach should be excluded from the diet - sour, fried, spicy, pickled, smoked, pickles are also removed. In addition, it is not recommended to eat carbonated drinks, coffee, alcohol, and easily digestible carbohydrates (chocolate, candy, cakes, baked goods).
Since the most common cause of any gastritis is the bacterium Helicobacter pylori, it is necessary to direct all efforts to its destruction. There are many drugs available today for this purpose. But any of them should be used only after consulting a doctor.
If atrophic gastritis is advanced and your own hydrochloric acid and enzymes cannot cope, then you need to use natural substitutes to help them. They are also prescribed by a doctor. For severe pain, your doctor may prescribe a pain reliever. Medicines are also sometimes prescribed to stimulate the stomach muscles. Atrophic gastritis can be completely cured. But only under the supervision of doctors and with strict adherence to the treatment they prescribed.
Thickening of the stomach wall on ultrasound: what are the causes, diagnostic features
In case of stomach diseases, one of the most informative and safe examinations for the patient is ultrasound diagnostics. When performing it, you can study the structure of the organ and peristalsis in real time. This is a hollow muscular organ and a sign such as thickening of the stomach wall indicates pathological changes in it.
Thickening of the stomach wall
The stomach performs several important functions in the body. It breaks down food products under the influence of hydrochloric acid and enzymes that are produced by glands located in the thickness of the mucosa. In addition, under the action of peristalsis - muscle contractions - food masses in the stomach are mixed, crushed, and moved into the intestines.
It also performs a protective function, disinfects food, destroying pathogenic microbes that come with it, and protects the abdominal cavity from the aggressive action of gastric juice.
All this is ensured by the special structure of the walls of the organ, therefore, if any changes are detected in them on ultrasound, this may give the diagnostician a reason to suspect the development of a number of diseases, including such a dangerous pathology as cancer. Let's consider what thickening of the walls of the stomach indicates, what it is, and what diagnostic value does this indicator have?
What should be the normal thickness of the stomach wall?
The stomach wall consists of three main layers, each of which has a specific function. They are clearly distinguishable during ultrasound examination:
- Slimy. Contains glands that produce hydrochloric acid, pepsinogen and other enzymes. On ultrasound it appears hypoechoic (dark line). It contains the mucosa itself and the submucosa, in which glands and blood vessels are located.
- Muscular. Consists of several rows of multidirectional muscle fibers. Their contraction provides peristalsis. Appears as a hyperechoic thin line.
- Serous. The subserous and serous layers are also distinguished; their density on ultrasound relative to the muscular layer is low, that is, the serous membrane looks hypoechoic.
What does thickening of the stomach walls mean?
When examining the stomach, the diagnostician pays attention not only to the thickness of the walls and its changes in different parts, but also to their rigidity, lack of peristalsis in a certain area, and smoothing of the relief of the folds. The detection of such signs may be the first symptom of a developing pathology, even with normal thickness
The physiological causes of thickening of the stomach wall on ultrasound are:
- inflammatory reaction causing tissue infiltration and swelling;
- benign, malignant neoplasms with exophytic growth into the gastric cavity at an early stage;
- interstitial tumors growing along the muscle layer.
Causes of thickening of the stomach walls
The main reasons leading to thickening of the stomach walls are as follows:
- gastritis, in which swelling of the mucous membrane and hypertrophy occur as a result of the inflammatory process;
- traumatic injuries cause inflammation with subsequent sclerosis of the damaged area;
- peptic ulcer, thickening caused by the formation of connective tissue (scar) around the lesion;
- Ménétrier's disease, a chronic disease characterized by hypertrophy of the mucosa with the formation of cysts and adenomas;
- benign formations (polyps), at an early stage they slightly rise above the mucous membrane, causing a feeling of thickening of the wall;
- malignant tumors of the stomach (adenocarcinoma, sarcoma, rhabdomyoma);
- tissue infiltration during specific infections (syphilis, tuberculosis, actinomycosis).
Changes that occur in the wall of the stomach and are detected on ultrasound are called hollow organ syndrome.
What are the benefits of undergoing an ultrasound of the stomach can be found in this video.
Ultrasound diagnosis of thickening of the stomach walls
Wall thickening can also be detected using x-rays, but ultrasound has several advantages. The examination allows you to study the organ in different projections, it is safe and does not have a harmful effect on the body. During the examination, the Doctor can see changes in each layer.
On ultrasound, the wall looks like a thin line consisting of three layers - hyperechoic inside and hypoechoic on the sides. The mucous membrane has folds that smooth out when the sensor is pressed. Normally, movements (peristalsis) can also be observed.
An increase in thickness occurs due to any of the layers. Thus, with interstitial tumors, changes in the size of the submucosal or muscular layer in a certain area are often detected. An increase in the mucous layer occurs during inflammatory processes and hypertrophy.
Causes, symptoms and treatment of gastric stenosis
Gastric stenosis is a complication of peptic ulcer disease, in which the normal lumen in the pyloric area narrows, which connects the stomach and intestines. Because of this, food simply cannot move normally through the digestive tract, which causes a whole host of side painful syndromes of the gastrointestinal tract, ranging from gastritis to relapse of ulcers (due to the prolonged presence of food in the stomach cavity). This often leads to a total disruption of hemostasis.
Symptoms
The symptoms of stenosis are quite vague and are described by a dozen painful sensations and discomfort in the stomach area. To simplify the diagnosis, doctors divided the symptoms into 3 stages, which differ in the degree of narrowing of the lumen for the passage of food.
- Stage 1 - slight narrowing. The patient mostly complains of frequent belching and an acidic taste in the mouth. Even after eating a small amount of food, he feels full in his stomach.
- Stage 2 - medium narrowing. The patient feels constant stomach fullness. After eating, he vomits, after which the discomfort decreases. Often all this is accompanied by painful sensations, as during ordinary gastritis.
- Stage 3 - severe narrowing. The disease progresses rapidly, and inducing vomiting does not help improve the patient’s well-being. Vomit has a strong stench because it contains food that has remained in the stomach for many days. Severe dehydration and weight loss are diagnosed.
Stenosis of the pylorus of the stomach can lead to hypertrophy of the organ, its stretching, and the appearance of esophageal hernias with compression of the diaphragm. The tissue around the pylorus becomes inflamed, pathogenic microflora develops there, which can provoke a recurrent ulcer.
There is also such a thing as congenital gastric stenosis, which develops specifically in newborns. Statistics indicate that pathology is much more common in boys than in girls. Accompanied by very rapid loss of body weight, vomiting, constant restlessness of the baby, lack of stool and urination. An extremely dangerous disease. If an accurate diagnosis is not made in a timely manner, the likelihood of death will be extremely high.
In the most severe cases, stenosis leads to bleeding in the stomach, disruption of the outflow of bile and liver function. If food does not enter the intestines within a few days after eating it, the natural process of rotting begins, releasing large amounts of gas. It is because of this that a distinct and sharp “aroma” of acetone, one of the decomposition products, is felt from the patient’s mouth.
Causes
There are two main causes of pyloric stenosis:
- a previous stomach or duodenal ulcer;
- congenital pathology.
Does stenosis occur in those who have not previously been diagnosed with an ulcer? This phenomenon also occurs, but is extremely rare (with the exception of newborns, of course). The reasons for its appearance: chronic gastritis, constant irritation of the gastric mucosa, as well as dysfunction of the sphincter, which separates the duodenum and the esophageal cavity. The disease also occurs in obese people with too much body weight. But in them the cause of stenosis is pressure on the esophagus and the pyloric area by fatty masses.
Another reason is the preference for fast food and the complete lack of a normal diet. At the same time, the mucous membrane and the walls of the stomach themselves atrophy and become inflamed due to excessive load from indigestible food. The free cavity of the esophagus decreases, hernias appear. As a consequence, there is a decrease in the natural gap of the pylorus, which turns into the most common barrier for food.
Treatment
If stenosis is diagnosed at the first, “mild” stage of its development, then treatment includes taking medications that help relieve inflammation and optimize the functioning of the entire gastrointestinal tract. Naturally, the patient will have to adhere to a strict diet for some time, which includes mainly products of plant origin (vegetables, fruits, cereals). Meat, eggs, milk are strictly contraindicated. In this situation, the likelihood of self-healing of the stomach, if the doctor’s recommendations are followed, is high.
If stenosis is detected already in the chronic stage, then the only correct radical treatment method is surgical intervention and removal of the damaged section of the esophagus (pylorus).
Often the operation involves drainage - the removal of slag masses that literally clog the passage into the duodenum. This disorder is more common among lovers of too spicy food and those who abuse strong alcoholic beverages.
Signs of improvement in the patient’s well-being occur immediately after the operation. The risk of relapse remains quite high. After eliminating the cause of the disease, the patient will need long-term restorative therapy and diet aimed at regenerating the beneficial microflora of the digestive tract. Doctors also recommend that during this period you cleanse your body of toxins and stop eating meat for a while (with the exception of fish and poultry).
The risk of surgical treatment of stenosis is very high. It is mostly associated with possible complications due to disturbances in the mineral-salt balance in the blood (due to severe dehydration). It is because of this that the surgeon may require artificially introducing nutritional serums into the patient’s body for several days, and only after that he will undertake the operation.
The folds of the mucous membrane in each part of the digestive canal have their own direction and thickness. With hypertrophy and inflammatory swelling of the mucosa, thickening of its folds may be observed. When an ulcer forms, a contrast agent penetrates into it, and then a “spot” appears against the background of the folds of the mucous membrane; it is called the “relief niche” (Fig. 186.2). When a small tumor appears, the folds of the mucous membrane move apart and seem to bypass the tumor. On the contrary, infiltration of the mucous membrane by a cancerous tumor leads to the disappearance of normal relief and breakage of folds
Chronic gastritis causes a syndrome of pathological changes in the gastric mucosa. They can only be identified on targeted images of the stomach (Fig. 195), taken with pressure on the anterior abdominal wall. On such radiographs, the folds of the mucous membrane seem to be crushed, but an image of small rounded elevations on the mucous membrane - the gastric fields - is achieved. Uniform distribution of gastric fields with a diameter of 1-3 mm over the mucous membrane indicates superficial gastritis. With deep gastritis, the relief of the mucous membrane becomes “grainy” - the areolas reach a diameter of 3-5 mm. With atrophic gastritis, the gastric fields are even larger and are unevenly distributed throughout the mucous membrane. In differential diagnosis, one must keep in mind erosions that resemble gastric fields. But erosion
Inflammatory changes accompanying the ulcer cause an increase in the number of folds of the mucous membrane, their thickening and tortuosity. When the ulcer scars, convergence (convergence) of the folds towards the ulcerative defect is noted. Thus, an ulcer can also cause a syndrome of pathological changes in the mucous membrane. But the leading one, as a rule, is the syndrome of limited expansion of the stomach in the form of niche formation. The same syndrome can be caused by an ulcerative form of stomach cancer. But with ulcerated cancer, the niche does not completely or does not protrude at all beyond the contour of the shadow of the stomach, sometimes it has an irregular shape and uneven contours. For many malignant ulcers, a flat shape is typical: their diameter (size of the base) is much greater than the length (depth of the ulcer). In all unclear cases, gastroscopy with gastrobiopsy is indicated. Sometimes only this research method allows us to resolve the question of the nature of ulceration.
Benign tumors of the stomach - polyps of various natures, leiomyomas, fibromas, etc. - cause pathological changes in the relief of the mucous membrane. Against the background of folds of the mucous membrane, a rounded defect (clearance) with smooth outlines is determined. The folds of the mucous membrane are not interrupted, but are moved apart and bypass the neoplasm. With “tight” filling, a benign tumor can hide behind the shadow of a contrast mass. To identify a tumor, targeted compression images are taken: on them, the tumor causes a round or oval filling defect with clear, sometimes finely wavy contours. Peristalsis is preserved.
Asked by: Ekaterina, Ust-Labinsk
Gender: Male
Age: 5
Chronic diseases: No.
Hello, good afternoon! I decided to examine my son so as not to miss any illness (we had a norovirus infection and vomiting, I was afraid that there were problems with the stomach). They did an ultrasound and found indirect signs of gastritis. The walls, while the norm is 6 mm, are 12 mm (that’s what the ultrasound doctor said). She said the stomach “glows” like a Christmas tree (suggested Helicobacter). A lot of mucus (because of this we were told there may be poor appetite, rapid satiety). In general, the child feels fine, there are no complaints and never have been about the stomach or gastrointestinal tract. With all this, we went to the pediatrician, got tested for roundworm, Helicobacter, Toxocar, toxoplasma, Giardia - nothing. Nevertheless, there are elevated eosinophils in the blood - the doctor said that the norm is 0.1, we have 14 (or 0.14, she did not specify). For the stomach, she prescribed Omez (1 capsule on an empty stomach, Acipol 3 times a day, Pancreatin - 0.5 tablets 3 times a day after meals.) We did all this, he also has no complaints, his appetite is bad, that’s it. It has always been difficult to force him to eat, but now, through persuasion and the fear of the hospital, I am trying to force him to eat little by little, often. At 5 years old he weighs 15.5 kg. Height is 107 cm. Tell me your opinion - were we prescribed adequate treatment? I know that it would be good to do a gastroscopy, but I know that I won’t force my son to do it on a good chance. (We donate blood from a finger - we keep it together with my husband, I myself can’t hold him), but I don’t want anesthesia. Could this change in the stomach be due to antibiotics? This year we have already been in bed three times (after kindergarten), three times we have received courses of antibiotics (once for 10 days, second time for 10 days, third time for 5 days). He never had allergies, neither did my husband or I, even in our immediate family there are no allergy sufferers. Why then are eosinophils elevated? And what are the prognoses for our stomach? I don’t want to feed me medications, but most of all I’m afraid of losing time and leading to a chronic condition. Thank you in advance!
How is the research conducted?
Examination of the stomach can be divided into abdominal ultrasound and gastroscopy. Gastroscopy is a research method in which a person swallows a special probe with a light bulb and a video camera.
To examine the stomach without swallowing a probe with a light bulb, you can do a regular ultrasound of the stomach through the anterior abdominal wall. But gastroscopy is all the better because the doctor can examine the internal organs from the inside. Therefore, these two methods should complement each other.
Classic ultrasound examination is performed through the skin of the abdomen, i.e. transabdominally. There are several varieties:
- Ultrasound examination of the stomach is first performed on an empty stomach in the usual way. The person lies on his back and frees his stomach from clothes. Then the doctor conducts an examination using an ultrasound machine. A thorough examination of all the walls of the stomach allows examination in different positions: lying on your back, on your side, standing.
- To determine the contractility of the organ, ultrasound of the stomach is combined with a water-siphon test. To do this, a person drinks a glass of tea without sugar. After a few minutes, a series of repeated tests are carried out to determine how quickly the liquid leaves the stomach. The norm is up to 25 minutes. If the delay is more than 40 minutes, they speak of slow motility of the organ or changes in the sphincter (narrowing, dysfunction, scar deformation).
- To see a stomach or duodenal ulcer on ultrasound or pathological formations, an ultrasound scan of the stomach and duodenum with contrast is performed. The person drinks a solution with a contrast agent, after which a second examination is performed. This improves visualization, since the contrast agent fills folds, wall defects, and improves the visibility of the contour of neoplasms.
The person is placed on his side and a special mouthpiece is inserted into the mouth, which prevents the teeth from accidentally closing. At the request of the person, local anesthesia can be performed. Then the person needs to swallow the so-called “hose”. This is a flexible sensor with a camera and a light bulb. When the sensor is swallowed, the doctor begins to examine all the walls of the stomach and duodenum.
Gastroscopy allows you to conduct additional examinations: measuring the pH of gastric juice, biopsy, removal of polyps.
- The pH of gastric juice is measured to determine acidity.
- A biopsy is performed to exclude oncology - a piece of tissue is taken to examine the cellular composition under a microscope.
- If there are tumors, you can remove them during the procedure and then send them to the laboratory for examination.