Treatment of gastritis and pancreatitis can be prescribed simultaneously, since these diseases indirectly depend on each other. The first is inflammation of the gastric mucosa, the second is a disruption of the functioning of the pancreas. But it is she who is largely responsible for the production of enzymes that contribute to the normal digestion of food.
If they are deficient, the digestion process is disrupted, which subsequently provokes gastritis, and in chronic cases, gastric and duodenal ulcers. So how can you overcome gastritis and pancreatitis and what can traditional medicine offer in this regard?
Etiology of simultaneous manifestations of gastritis and pancreatitis
Gastritis and pancreatitis are pathologies of the gastrointestinal tract, the symbiosis of which occurs very often in the life of a modern person. The development of the disease is accompanied by many factors, such as irrational nutrition, overeating or undereating, mid-flight seizures, dryness, stress and anxiety, as well as infection with fungal bacteria due to non-compliance with hygiene rules.
Doctors have proven that both of these diseases do not develop simultaneously, however, they can manifest themselves together as a result of several reasons.
First of all, if accompanying indicators are present, gastritis develops, which, with improper treatment or its complete absence, degenerates into a chronic form. Sometimes a person who suffers from gastritis does not even know that he has it. There is the so-called chronic antral gastritis, which is dangerous because its course may not initially cause serious discomfort to a person. It arises due to infection of the stomach by harmful pathogens and evolves in the antrum of the stomach, located between it and the duodenum.
Over a period of time, the acidity in the section of the stomach infected with the rod is disrupted, as a result of which food is not fully digested. Then it begins to rot in the duodenum, from which the contents, due to improper digestion, are released into the pancreas and pancreatitis develops. The danger lies in the fact that the course of antral gastritis is sometimes not accompanied by severe pain or serious discomfort, and not every person pays attention to minor manifestations of the disease in the form of feeling unwell after eating. Against the background of these events, the patient learns about the diseases already when he has fully developed chronic gastritis, chronic pancreatitis, and their manifestations are acute.
And also the source of the genesis of two diseases at the same time can be the patient’s inappropriate attitude towards his health, ignoring gastritis in its manifestations, as a result of which pancreatitis, which is characterized by inflammation of the pancreas, also progresses.
As a result, pancreatitis most often manifests itself against the background of advanced chronic gastritis of various origins.
Causes of diseases of the gastrointestinal tract
The main cause of gastrointestinal diseases is poor nutrition. The frantic rhythm does not allow you to eat often and healthily. Preparing the right food takes a lot of time, snacks and quick meals are the way out of the situation for every third person.
Nervous tension, constant stress, overwork, fears can cause disturbances in normal digestion.
Pancreatitis and gastritis are common diseases that can take even children by surprise, so nutritional culture should be instilled in early childhood.
Signs of parallel manifestations of pancreatitis and gastritis
Synchronous inflammation of the stomach and pancreas is very dangerous for human health. Diseases can be identified by some common symptoms, however, it would be advisable to consult a doctor to make a diagnosis and prescribe the correct treatment. The attending physician must be told about all the signs and manifestations of the disease, as well as undergo a special examination so that he can make an accurate diagnosis.
Signs of inflammation of the stomach and pancreas are:
- Severe pain in the stomach area, which can alternate with sharp pain radiating to the lumbar region.
- Alternating dry mouth with strong salivation.
- Prolonged apathy, against the background of which nervousness and causeless anxiety appear.
- Loss of strength and weakness with frequent manifestations of drowsiness and dizziness.
- Constipation alternating with loose, foul-smelling stools.
- Nausea, which often progresses to vomiting.
If these diseases are ignored, self-destruction of organs can occur, which will lead to the death of a person, therefore it is important to diagnose the disease in time and immediately begin rational treatment.
How to distinguish the symptoms of two diseases
The simultaneous course of pancreatitis and gastritis poses a great danger to the patient. In advanced forms of these diseases, self-destruction of the stomach and pancreas is observed, leading to death.
Common signs of gastritis and pancreatitis are:
- pain in the abdomen;
- flatulence;
- nausea;
- vomit;
- bloating;
- loss of appetite;
- heartburn;
- sour belching;
- stool disorders;
- general weakness;
- sweating;
- pallor of the skin.
Bloating is one of the reasons for the simultaneous occurrence of pancreatitis and gastritis in the body.
The question often arises about whether it is possible to determine the specific manifestations of pancreatitis and gastritis. An experienced specialist, having examined the symptoms of diseases and carried out a full diagnosis, can easily determine how these pathologies manifested themselves and differentiate them.
The main differences in the development of gastritis and pancreatitis are associated with abdominal pain. In chronic gastritis, they often manifest themselves in the solar plexus area in the form of colic or spasms. With pancreatitis, the pain syndrome is quite well expressed. The pain is of a cramping, encircling nature, starting from the navel, radiating to the back area.
With gastritis, pain begins immediately after any violations in the diet. Vomiting brings tangible relief to a person. With inflammation of the pancreas, errors in nutrition do not appear immediately, but with a slight delay. Exhausting vomiting does not bring relief.
Methods of combating diseases
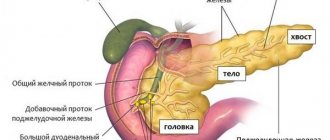
The technology for treating gastritis and pancreatitis with their parallel exacerbation depends on certain factors that are based on the etiology and development of the diseases. Treatment tactics vary depending on whether the acidity in the stomach is increased or decreased, as well as taking into account the stage of damage to the pancreas. Pancreatitis can be at the initial stage, when the gland is inflamed, however, there are no irreversible processes. The stage of the disease is considered more serious when the pancreas, due to abnormal functioning, begins to digest itself.
Most often, when diagnosing these diseases, treatment is prescribed, which has two key areas: medications and adherence to a proper diet.
In addition to official methods of treating the digestive tract, folk remedies are also used, which are often prescribed or recommended by doctors. Traditional treatment of pancreatitis is very popular and often gives positive dynamics for recovery when combined with official methods. Even pharmacies today sell special herbal tinctures, as well as herbal teas recommended for the treatment of the digestive tract. Popular treatment components include propolis, rose hips, wormwood, decoctions of St. John's wort, chamomile, calendula and golden mustache, which are found in a variety of traditional medicine recipes.
Doctors often prescribe Monastic Tea, which has anti-inflammatory, sedative and antispasmodic effects and is indicated for pancreatitis and gastritis of various etiologies. However, doctors do not recommend abusing “grandmother’s” recipes, since not all traditional medicine recipes are safe; their use and overdose can cause not only a relapse of the disease, but also death.
General rules for patients with gastritis and pancreatitis
Regardless of the stage of the disease, as well as their course, there are common requirements for patients, the fulfillment of which accompanies recovery:
- Quitting bad habits, such as alcohol and smoking, which have a detrimental effect on the condition of the human body, including the organs of the digestive system.
- Exclusion from the diet of spicy, sour and fatty foods, during an exacerbation, adherence to a specific strict diet prescribed by medical professionals.
- Eating in small portions, with an increase in the number of meals from five to eight times a day.
- Increasing fluid intake in the form of water or tea to one and a half liters per day, which must be consumed in small portions throughout the day.
- On the first day of exacerbation of the disease, completely stop eating, leaving only warm tea and water in the diet, which should be drunk in small doses slowly. Thus, the load on the stomach and pancreas is relieved, which is accompanied by a reduction in pain symptoms.
A proper diet for inflammation of the digestive system is one of the main aspects in the treatment of diseases. It is worth noting that patients with chronic manifestations of diseases will have to adhere to a diet throughout their lives in order to avoid relapses. For the first week, a strict special diet is followed, which is called “Therapeutic Table No. 1”. Then the patient can switch to an expanded menu, which contains dishes from approved products for illnesses. In addition to the therapeutic diet, the patient is prescribed medications.
Drug treatment of pancreatitis and gastritis
It is strictly forbidden to self-prescribe medications for the treatment of diseases such as gastritis and pancreatitis, since their prescription varies depending on the development of the pathology. Improper use of medications may not only fail to alleviate the patient’s condition, but may also lead to even greater irritation of the mucous membranes of the walls of the digestive organs, which will increase inflammation. Irrational treatment can cause the development of ulcers, as well as stomach or pancreatic cancer, which can be fatal.
Remember, there are no universal drugs for the treatment of gastritis and pancreatitis; each patient needs an individual approach and prescription of therapy according to the established diagnosis based on medical research.
For the treatment of gastritis and pancreatitis in acute forms, doctors often prescribe antibiotic therapy, which helps reduce intoxication in the gastrointestinal tract. At the same time, antispasmodics or analgesics are prescribed to reduce pain syndromes.
For gastritis with high acidity, complex treatment includes drugs that block or reduce the release of hydrochloric acid, which accompanies the restoration of microflora, as well as an antacid group that neutralizes its effect. Ranitidine is a frequently prescribed drug for patients with gastritis with high acidity, which helps reduce hydrochloric acid and the level of inflammatory processes in the digestive organs.
With reduced gastric secretion, it is recommended to take drugs that enhance the production of hydrochloric acid, which stabilize acidity and help improve the digestion process. Frequently prescribed drugs are Pancreatin or Festal.
To reduce pain syndromes in periodic manifestations, you can take the drug No-shpa, which relieves spasms in the shortest possible time and also helps reduce inflammatory processes. The drug is commercially available, has few contraindications and is considered the safest among antispasmodics. However, doctors recommend taking it in rare cases; in situations with systematic recurrence of exacerbations, contact a medical institution where the attending physician can prescribe rational treatment.
Pancreatin in complex therapy of gastritis and pancreatitis
Pancreatin is a relatively safe medical drug, the formulation of which includes extracts from the pancreas of animals. Taking the drug "Pancreatin" makes it easier for the stomach and pancreas to handle food that is difficult to digest and assimilate.
Pancreatin is prescribed in the following cases:
- for chronic pancreatitis;
- in complex therapy of chronic gastritis;
- before eating junk food;
- for constipation, indigestion, frequent belching and abdominal discomfort;
- to improve digestive function for preventive purposes.
The product is indicated for use both in chronic gastritis with low and high acidity. Its properties help improve digestion, which allows its use even as a preventive measure before grandiose feasts.
Treatment
To eliminate the symptoms that occur with pancreatitis and gastritis, special medications will help not only to eliminate the symptoms, but also to determine the cause of the disease.
- Nausea and vomiting can be stopped with the help of special medications. For example, it could be Cerucal and Motilium.
- The following drugs Pancreatin, Panzinorm or Mezim will help to start the functioning of the organ during pancreatitis.
- In order to eliminate the cause of gastritis, you need to take a course of antibiotics Pilobact, Klacid, Losek and Ampicillin.
- You can drink Papaverine and No-shpa to eliminate painful sensations.
There are also medications that need to be taken for high acidity. There are medications that are needed to protect against damage and the harmful effects of hydrochloric acid on the walls of the stomach.
These drugs are Ranitidine and Cimetidine. Drugs such as Pantoprazole and Omeprazole will help stop acid production. Almagel, Maalox, De-nol will protect the gastric mucosa.
It helps with problems with the pancreas to take tablets such as Pancreatin. They contain an enzyme that helps break down food.
The action of this drug is aimed at producing juice. The components that are included in Pancreatin help improve the functioning of the stomach, pancreas, intestines and liver.
Pancreatin is used after meals if a large amount of fatty food was consumed during the meal. Additionally, Pancreatin is prescribed for a sedentary lifestyle and pregnancy.
Pancreatin is used to prepare the gastrointestinal tract for diagnostics. There is also a disturbance in the functioning of the liver, stomach, intestines and gall bladder.
With gastritis, there is a violation of the gastric mucosa. If you take Pancreatin for this disease, it helps to quickly overcome the exacerbation process.
In a chronic state, pancreatitis and gastritis require constant replenishment of missing enzymes. You need to take Pancreatin both for a certain period of time to relieve symptoms, and to take it continuously.
In order to cure diseases, you need to take Pancreatin. The diet also helps to improve pancreatitis and stomach disorders.
Treatment must be taken systematically to see the desired result.
Let's sum it up
The synchronous manifestation of diseases such as pancreatitis and chronic gastritis is not uncommon today. However, it is almost impossible to identify diseases and make a diagnosis only by symptoms at home, since the diseases have similar manifestations and similar localization of pain.
For rational treatment of diseases, it is better to immediately contact specialists who can make the correct diagnosis and prescribe effective treatment. Gastritis and pancreatitis are diseases that are dangerous even in their individual manifestations. In symbiosis, if left untreated, they can even cause death. Don't put off going to the doctor until tomorrow.
Gastritis
With gastritis, symptoms such as vomiting, stomach pain, and nausea often appear. They may indicate the presence of an inflammatory process in the walls of the stomach.
Sometimes the disease occurs on its own, sometimes due to other diseases.
The acute inflammatory process goes away unexpectedly. There may be intense pain, as well as an increase in temperature to 37.2 or 37.5 degrees.
If not treated promptly, the disease may become chronic. In a chronic condition, a period of remission alternates with a period of exacerbations.
Treatment should be carried out by the patient regardless of the stage.
Treatment of gastritis is prescribed depending on the level of acidity: high or low.
Causes of pancreatitis
As a rule, pancreatitis occurs in adults, since they drink alcohol, have an unbalanced diet and have any concomitant diseases. Triggering factors for the onset of inflammation in men and women are different:
- In men, problems with the gland are provoked by poor diet (fatty foods and frozen ready-made foods, fast food) + alcoholic beverages, as well as cholelithiasis.
- In women, the disease is provoked by fasting, unbalanced nutrition due to dieting, cholelithiasis, hormonal imbalances due to contraceptive drugs, pregnancy, menopause.
The reactive form in adults occurs against the background of problems with the gastrointestinal tract, operations, and injuries. For example, gastritis, cholelithiasis, intestinal infections, and cirrhosis can provoke reactive pancreatitis.
Since children, as a rule, are not fond of alcohol and fatty foods, the causes of their symptoms may be injuries, surgeries, a history of mumps, cystic fibrosis, or food allergies.
Basic principles of patient nutrition
It is necessary to eat more protein foods and at the same time exclude fatty and carbohydrate foods. First of all, the advice concerns sugar, fried foods containing coarse fiber. If possible, start taking vitamin supplements. You should eat in small portions, at least 5-6 times a day.
General characteristics of the products consumed
The nutrition that is prescribed at the stage of extinction is that the consumption of proteins is increased to the level necessary for the full functioning of the patient’s body. Lipids and carbohydrate substances are presented in the form of all kinds of cereals. Complex sugars, honey, and confectionery products are excluded from the menu, and salt consumption is reduced.
Nutrition for chronic pancreatitis involves the absolute exclusion from the diet of foods that irritate the walls of the esophagus. This includes: alcoholic beverages, acetic, citric acid and other seasonings.
Basics of use and composition of servings
Food is prepared by boiling, stewing, baking, and steaming. It is advisable to eat foods that have been previously ground in a blender or rubbed through a culinary sieve. Nutrition is carried out at equal intervals, every 3-4 hours. Food is offered warm; eating too hot food is unacceptable. The main daily menu items should include: total protein - 120 g, lipid mass - 90 g, carbohydrate substances - 350 g, and have an energy value of no more than 2700 Kcal.