Study of the content (activity) of pancreatic enzymes in blood and urine
Determination of amylase and isoenzymes in blood and urine
Determination of amylase levels in blood and urine is the most common diagnostic test. The low sensitivity of amylase determination in blood and urine is associated with the short duration of hyperamylasemia and hyperamylasuria in pancreatitis. Thus, the level of blood amylase begins to increase after 2-12 hours from the onset of exacerbation of the disease, reaches a maximum after 20-30 hours, and normalizes after 2-4 days with a favorable course of the disease. The amylase content in the urine begins to increase 4-6 hours after the onset of the disease, and after 8-10 hours, according to some reports 3 days, it can already return to normal. In severe exacerbation of CP, amylase activity can be “depleted” to normal and subnormal values.
Determining amylase levels in urine is more informative than in blood, since hyperamylasuria is more persistent than hyperamylasemia. The availability of urine allows the study to be repeated many times and therefore even a slight increase in the indicator can be detected. More sensitive than the amylazuric test is the calculation of uroamylase flow rates, when urine collected at certain periods of time before and after a food load is examined.
The sensitivity of these flow rates for HP is 49-73%.
- To increase the sensitivity of studying the level of amylase in the blood and urine of A.I. Khazanov recommends studying them on the first day of hospital stay for patients with chronic pancreatitis (CP), then at least twice after instrumental studies, as well as at the time of intensification of abdominal pain.
At the same time, in his opinion, the sensitivity of the test increases from 40 to 75-85%.
There is no level of amylase in the blood that is pathognomonic for pancreatitis. Due to the significant reserve of the enzyme in acinar cells, any violation of their integrity or the slightest difficulty in the outflow of pancreatic secretions can lead to a significant release of amylase into the blood, even with mild pancreatitis. On the contrary, with severe destruction of the organ parenchyma, hyperamylasemia may not be detected. Thus, in some cases there is no direct connection between the severity of pancreatitis and amylasemia.
- To increase the specificity of the study of amylase in the blood, it is necessary to determine not the total content of the enzyme, but pancreatic isoamylase.
In healthy people, p-amylase accounts for up to 40% of total serum amylase, the remaining 60% is represented by salivary isoamylase. In chronic pancreatitis, this ratio changes: pancreatic isoamylase accounts for 75-80% of total blood amylase.
- Determination of pancreatic isoamylase activity is especially important in CP in patients with normal levels of total amylase.
- An increase in the indicator indicates an exacerbation of CP, and a decrease indicates exocrine pancreatic insufficiency.
In general, the specificity of determining pancreatic amylase in CP does not exceed 88.6% with a sensitivity of 40-96.9%.
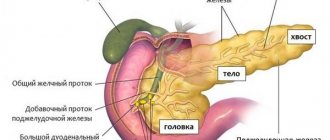
Surgical treatment of chronic pancreatitis
Surgical intervention for chronic pancreatitis is indicated in two situations:
- If conservative treatment is ineffective (unbearable pain, disease progression, total or subtotal pancreatic necrosis);
- If complications arise.
All surgical interventions can be divided into 2 types: radical and palliative.
In radical surgery, total (complete), subtotal (part) or lobar (lobular) removal of the pancreas is performed. In this case, anesthetized (dead, non-functioning) areas of the organ are removed. Most often, such intervention is carried out urgently, for health reasons. This prolongs the patient’s life, slows down the further development of the disease, and relieves the effects of intoxication in the body. However, after such an operation, the patient is required to undergo lifelong enzyme replacement therapy, and serious complications also occur quite often.
Serum lipase
The method for determining serum lipase is also not sensitive and informative enough. Data on the duration of hyperenzymemia. It is impossible to determine the severity of the current exacerbation of pancreatitis and the immediate prognosis based on serum lipase levels. Hyperlipasemia is recorded in 60% of patients with diseases of the hepatobiliary system, intestinal obstruction, renal failure, prostate cancer and other non-pancreatic diseases.
- More specific is a decrease in the level of lipase in the blood in relation to pancreatic fibrosis, as an outcome of CP and cystic fibrosis.
Etiology
A common cause is alcohol abuse and the presence of gallstones or other gallbladder pathologies.
Other provoking factors that can cause inflammation of the pancreas include:
- parenchymal pancreatitis with a chronic course, observed in metabolic disorders;
- hormonal imbalance;
- vascular pathologies;
- injuries or other injuries in the abdominal area;
- diseases of the digestive system (for example, duodenitis or peptic ulcer);
- taking pharmacological agents (Furosemide, antibiotics, hormonal or sulfonamide drugs);
- surgical treatment in which surgery was performed on the stomach or biliary tract;
- infectious diseases (for example, mumps);
- viral hepatitis;
- ascariasis and other helminthic infestations;
- anatomical abnormalities.
It is worth noting that in some cases, hereditary predisposition plays a role. Sometimes the cause of chronic pancreatitis cannot be determined. At the same time, it is more difficult to determine how and with what to treat patients.
Serum elastase 1
The activity of this enzyme in the blood increases in chronic pancreatitis earlier than the level of other enzymes and lasts longer.
- Determination of elastase 1 activity is considered the “latest” sensitive test for diagnosing exacerbations of CP, since elevated blood levels persist for 8-10 days after the attack. During this period, the activity of elastase 1 in the blood was increased in 100% of patients, the level of lipase in 85%, pancreatic isoamylase in 43%, and total α-amylase in 23% of patients.
However, there is an opinion that the specificity of hyperelastasemia does not correspond to the degree of destruction of pancreatic tissue and does not have much diagnostic value for functional failure in patients with long-term CP.
Intoxication psychosis
Intoxication psychosis is typical for people who abuse alcohol. Expressed in uncontrolled behavior, hallucinations, hyperthermia.
There is a risk of developing vascular thrombosis from the breakdown products of pancreatic tissue.
Late complications occur 15–20 days a week from the onset of the disease and are caused by the addition of an infection.
Purulent pancreatitis, parapancreatitis, peritonitis. Characterized by high body temperature, fever and excessive sweating. There is a risk of developing sepsis, abscesses and phlegmon of the abdominal cavity, as well as cysts and fistulas of the stomach or pancreas.
Pneumonia and pleurisy (most often left-sided). Symptoms:
- difficult shallow breathing;
- dyspnea;
- chest pain and wheezing;
- bluishness of the skin.
Assessment of exocrine pancreatic function
Tests to assess exocrine pancreatic function may be required to support the diagnosis of CP. They are almost always combined with ultrasound, x-ray and other studies, but can also be used independently for diagnostic purposes.
They can be divided into two groups: tests that require the insertion of an intestinal tube, and non-invasive tests without tubes. The latter have clear advantages in terms of patient comfort and risk and are also less expensive than probe tests. Unfortunately, there is no probeless test that has been successfully used as a standard method; all of them have both insufficient sensitivity and specificity. Almost all of these tests are based on determining the reduced secretion of pancreatic enzymes, however, due to low sensitivity, they are effective only with a very significant decrease in enzymatic secretion.
Carrying out probe and probe-free methods for determining the exocrine function of the pancreas is not mandatory for every gastroenterology department; in a particular case the necessary choice must be made. At present, it is probably reasonable to strive for a range of imaging tests, together with the Lund test and one non-invasive study. In such cases, imaging tests should be performed first, followed by functional tests in patients with suspected but not confirmed CP.
Probe methods
Direct probe method - secretin-pancreozymin (secretin-cholecystokinin) test.
In general, if all necessary technical conditions are met, the diagnostic accuracy of the method is extremely high; The sensitivity and specificity of the method are more than 90%. Most scientists recognize the role of this test as the gold standard for determining disorders of the exocrine function of the pancreas; some of them believe that the direct probe method is mandatory when diagnosing CP. Using the test, it is impossible to carry out differential diagnosis with other diseases of the pancreas, since with pancreatic cancer, cystic fibrosis and other diseases of the pancreas, pathological results of this test are recorded in 75-90% of cases.
Interpretation of the results of a probe study , identification of pathological types of pancreatic secretion (according to N.A. Skuya):
- Hyposecretory – decreased production of enzymes and bicarbonates with a normal volume of secretion. This type is characteristic of diffuse fibrosis of the pancreas (late stages of CP), cystic fibrosis, and is less commonly detected in pancreatic cancer.
- Hypersecretory - normal or increased volumes of secretion and bicarbonate flow, increased enzyme activity. This type is characteristic of initial inflammatory processes in the pancreas without signs of acinar cell atrophy and severe fibrosis. It is observed in the initial stages of CP, with a short-term and slight delay in the outflow of pancreatic secretions (with duodenal ulcer, short-term spasm of the sphincter of Oddi, etc.).
- The obstructive type is divided into 2 subtypes:
- lower block - a decrease in the volume of secretion at a normal concentration of bicarbonates and enzymes, which leads to a decrease in their flow rate. Characteristic of pancreatitis that has developed as a result of processes that impede the outflow of pancreatic secretions (persistent spasm of the sphincter of Oddi, papillitis, tumors of the Vater's papilla or head of the pancreas, obstruction of the gastrointestinal tract with a calculus);
- upper block - decreased secretion volume, increased enzyme concentration (but their flow rate is still reduced), normal bicarbonate content. This option indicates swelling of the pancreas and is characteristic of edematous pancreatitis (AP, exacerbation of CP).
Ductular - decreased secretion volume, normal enzyme production, sharp increase in bicarbonate concentration. Perhaps such changes are associated with inflammation of the ducts and impaired bicarbonate reabsorption.
The disadvantages of the method include the need for duodenal intubation, which is burdensome for the patient, the large amount of work of the laboratory assistant, the high cost and low availability of pancreatic stimulants. Thus, the cost of the secretin-pancreozymine test in the USA is $610, which is comparable in cost to CT and MRI.
Treatment of chronic pancreatitis during exacerbation
During the period of exacerbation, treatment of chronic pancreatitis pursues the following goals:
- Relief of pain syndrome.
- Decreased pressure in the pancreatic ducts.
- Correction of water and electrolyte disorders.
- Decreased secretory activity of the pancreas.
- Stimulation of intestinal motility.
Anesthesia
To reduce pain, the patient is advised to fast in the first days of an exacerbation. Then a gentle diet is prescribed (table No. 5). First of all, foods that increase the enzymatic activity of the gland are excluded from the diet. This is spicy, fried, salty, fatty food. It is better to eat 5 times a day, the emphasis is on protein foods (lean meats and fish, dairy products). To make food easier to digest, it is served in small portions, warm but not hot, in a liquid or semi-liquid state.
Important! Patients who follow all the principles of a gentle diet experience exacerbations 3 times less often, undergo surgical interventions less frequently, and recover faster.
If the pain syndrome is not relieved in the first days, non-steroidal anti-inflammatory drugs (paracetamol, diclofenac, etc.) and antihistamines (suprastin, diphenhydramine, pipolfen, etc.) are added to the treatment. This combination of drugs relieves inflammation and pain, reduces the toxic effect of inflammatory agents on the human body.
For persistent pain syndrome, narcotic analgesics (trimeperidine or octreotide) are added to treatment. As an alternative method of pain treatment, blockade of nerve trunks and plexuses is possible.
Decreased intraductal pressure
With timely treatment of hypertension, pain and inflammation go away faster, which means the acute phase of pancreatitis passes. Removing congestion in the pancreatic ducts is possible only by relaxing the sphincter of Oddi (it is located between the main duct and the cavity of the duodenum). Antispasmodics (no-spa, papaverine, baralgin, atropine, platiphylline, metacin) are used to treat and relieve spasms.
Indirect probe method (Lund test)
The fact that the Lund test, developed in 1960, is still used in most gastroenterological laboratories indicates its general acceptance; it has been around longer than any functional test designed to routinely assess RV function. The sensitivity of this test is 90% in patients with CP. Individual false-positive results may be detected in patients with small intestinal malabsorption, ciliacia, gastrostomy, and diabetes mellitus. However, depending on the degree of exocrine pancreatic insufficiency in CP, the sensitivity of the test ranges from 66-94%.
- The Lund test is less sensitive in the early stages of exocrine pancreatic insufficiency.
The Lund test is cheaper, easier to perform, and more convenient for the patient. The disadvantages of the method include the need for duodenal intubation, the inability to determine the volume of secretion and concentration of bicarbonates, the influence on the test results of intraduodenal acidity and endogenous secretion of hormones from the duodenum.
Tubeless methods for diagnosing exocrine pancreatic insufficiency
Indirect methods without duodenal intubation are based on the oral administration of specific substrates for pancreatic enzymes. After the interaction of the latter with pancreatic enzymes, cleavage products are determined in urine and/or blood serum, the quantity of which is used to judge exocrine pancreatic insufficiency.
Causes
The main cause of chronic pancreatitis is poor metabolism (i.e., the result of chemical reactions in the body) due to diseases and so on. factors.
The disease can occur due to the following pathological processes in humans:
- intraductal obstruction by tumors or stones;
- toxic metabolites that release cytokines (from pancreatic acinar cells);
- necrosis, fibrosis of the pancreas;
- oxidative stress;
- ischemia;
- chronic alcoholism;
- autoimmune disorders;
- hyperlipidemia, hypercalcemia;
- obstruction (blockage) of the main pancreatic duct (can be congenital or acquired).
Hereditary pancreatitis is an autosomal dominant disease, accounting for 1% of cases. Cystic fibrosis, an autosomal recessive disease, accounts for a small number of cases of chronic pancreatitis.
Chronic autoimmune pancreatitis has clinical features such as an enlarged pancreas, narrowed pancreatic duct, circulating gamma globulin and the presence of autoantibodies. The causes of the disease in almost 30% of cases are idiopathic (independent).
Blunt abdominal trauma resulting from an accident leads to acquired obstructive chronic pancreatitis .
Necrotizing inflammation in the pancreas is a typical response to injury . Extracellular matrix deposition and fibroblast proliferation in the pancreas involve a complex interaction of a group of hormone-like proteins such as cytokines, growth factors and chemokines.
When the pancreas is damaged , a protein that controls proliferation (transforming growth factor beta) is released and its local expression stimulates the growth of mesenchymal cells and increases the synthesis of extracellular matrix proteins such as fibronectin, proteoglycans and collagens.
There is evidence that chemokines, a family of small cytokines, are involved in the onset and progression of chronic pancreatitis.
Provoking factors of chronic pancreatitis
alcohol abuse comes to the fore , and therefore the number of diseases is growing rapidly. This applies to both males and women, who often like to sip.
Bentiramide test (NBT-PABA test)
This probeless test is based on the fact that N-benzoyl-L-tyrosyl-p-aminobenzoic acid (NBT), which is essentially a synthetic, chymotrypsin-specific tripeptide, is hydrolyzed by this enzyme to form p-aminobenzoic acid (PABA). The isolated PABA is absorbed, conjugated in the liver and excreted in the urine, where it is determined. The actual estimate of PABA in urine reflects the amount of chymotrypsin excreted by the pancreas.
The sensitivity of the method is 83%, and the specificity is 89%. False-positive results were observed in a quarter of patients with diseases of the small intestine, renal failure, gastric resection, celiac disease, Crohn's disease, impaired liver function, renal failure, and diabetes mellitus.
- The fundamental disadvantage of non-invasive methods is the weakening of their sensitivity in cases of moderately severe exocrine pancreatic insufficiency.
Despite these limitations, the NBT/PABA test can claim the greatest significance and stability among indirect methods.
Qualitative scatological research
A qualitative scatological study is carried out while patients follow a standard diet (for example, the Schmidt diet, including 105 g of protein, 135 g of fat, 180 g of carbohydrates) provided that multienzyme drugs are not used during this period of time.
- The criteria for exocrine insufficiency are an increased content of neutral fat and soap in the feces with a slightly changed content of fatty acids. An increased content of muscle fibers indicates the presence of creatorrhoea.
Quantitative determination of fat in feces
Normally, after taking 100g of fat with food, up to 7g of neutral fat and fatty acids are released per day. An increase in the amount of fat indicates disorders of the digestion and absorption of fat, most often of pancreatic origin. Determining the severity of steatorrhea is used as a simple and reliable indicator of severe exocrine pancreatic insufficiency. This test is widely used. Its reliability decreases with incomplete (incorrect) stool collection and against the background of an inadequate diet, especially in outpatients. The test is nonspecific for a number of diseases, which does not allow it to be used to determine the pancreatic nature of steatorrhea. The test data almost always does not fit into normal values in cases of damage to the ileum and bacterial contamination of the small intestine.
Determination of fecal elastase 1
Over the past decade, the enzyme immunoassay method for determining elastase 1 in the stool of patients with CP has become widespread. The sensitivity of the elastase test in patients with severe and moderate exocrine pancreatic insufficiency is close to that of the secretin-pancreozymin test, and according to most foreign researchers it is 90-100%, and in mild cases - 63%, specificity - 96%.
This method is simple, fast and inexpensive, has no restrictions in application, and allows us to determine the state of the exocrine function of the pancreas at earlier stages than before.
- The method in many cases provides diagnostic sensitivity and specificity close to those of direct methods for assessing the exocrine function of the pancreas.
Tumor markers
An increase in the level of tumor markers (CA19-9, CEA) above the value acceptable for inflammation is an indirect sign of the transformation of CP into pancreatic cancer. These tests are used for the differential diagnosis of pseudotumor forms of pancreatitis. Patients with pancreatic cancer have high levels of carcinoembryonic antigen (CEA), but its standard measurement lacks specificity; positive results are observed with other tumors and with exacerbation of CP. The sensitivity and specificity of determining CA19-9 in the diagnosis of pancreatic cancer ranges from 70-95% and 72-90%, respectively. Although most pancreatic cancers cause elevated serum levels of CA19-9, the specificity of this tumor marker never approaches 100%.
Irreversible changes in the gastrointestinal tract
Under the influence of constant exacerbations of the inflammatory process and destruction of pancreatic cells, the dead areas of the organ are replaced with connective tissue (scarring, fibrosis or sclerosis of the pancreas) - this is an irreversible change in the anatomy and physiology of the gland. Such areas are no longer useful in terms of performing exocrine or endocrine functions.
Pathological changes gradually develop in other organs of the digestive tract. The mucous membranes of the stomach, duodenum, gallbladder, bile ducts, and esophagus are subject to inflammatory changes. In the stomach and esophagus, erosions appear on the walls and, as a result, sclerosis of the walls, strictures (narrowing of the lumen) of the hollow organ. Inflammation of the gallbladder (cholecystitis) contributes to stagnation of bile and the formation of stones in the bladder. Damage to liver cells causes liver lipomatosis (replacement of dead hepatocytes with adipose tissue). The inflammatory process in the walls of the small intestine is dangerous due to the formation of intestinal obstruction.
The course of the disease is protracted, and pathology gradually develops. There are three forms of development:
- Mild - when the ducts remain unchanged, there is a slight increase in the organ, a slight change in structure.
- Moderate - the presence of cysts less than 10 mm, unevenness of the gland duct, infiltration (penetration of substances into the organ by one third), uneven edges and contours, thickening of the walls.
- Severe – the presence of cysts more than 10 mm, an unevenly dilated duct, a complete change in the structure and enlargement of the gland.
Clinical blood test
With an exacerbation of CP, a general blood test may reveal leukocytosis, a shift of the formula to the left, neutrophilia, and accelerated ESR syndrome. During treatment, there is a rapid, clear reduction in leukocytosis; somewhat later, ESR numbers normalize, which is one of the favorable clinical signs.
- Long-lasting leukocytosis with a shift to the left and elevated ESR numbers can serve as one of the nonspecific markers of the development of complications.
In patients with CP with exocrine insufficiency, leukocytosis is rarely detected. Moreover, moderate leukopenia is characteristic, indicating the presence of trophological deficiency. In this case, long-term indicators of accelerated ESR may be observed, which is most often due to dysproteinemia. In patients with severe forms of malabsorption syndrome, signs of iron deficiency, B6-, B12- and folate deficiency, and more often, mixed anemia may be observed.
Dangerous phenomena of acute pancreatitis
The danger of the acute form of the disease begins with attacks that can develop instantly and last from several hours to several days. Moreover, the more severely the gland is affected, the longer the attack lasts.
Often during an attack, constant vomiting develops, with bile particles, pain is localized in the upper abdomen, and dehydration occurs. The pain is so intense that it can lead to the development of pain shock in the patient.
Changes in the skin of the abdomen and navel and complexion appear. The tongue is predominantly white, but in severe cases it is brown. The pupils dilate, bloating occurs, the urine darkens, and the stool becomes lighter.
To reduce the risk of severe complications and danger to life, immediate medical attention is required. Treatment is carried out in a hospital.
Types of acute pancreatitis:
Edema is swelling of a diseased organ with small areas of necrosis in the adipose tissue nearby.
Necrotic is extensive necrosis of the organ itself with hemorrhages, including around it in the fatty tissues.
Under certain factors, for example, excess fat deposits around the organ (obesity), edematous pancreatitis easily turns into necrotizing.
Blood chemistry
A reduced level of total blood protein, albumin, transthyretin, transferrin, ferritin and other proteins characterizing the visceral pool of proteins and the degree of trophological deficiency may be observed. Dysproteinemia is recorded, characterized by a decrease in the albumin-globulin ratio and a relative increase in α1-α2-globulins.
Elevated levels of blood transaminases, gammaglutamyltransferase, and lactate dehydrogenase are often recorded.
- An increase in bilirubin, mainly direct bilirubin, cholesterol and alkaline phosphatase is characteristic of the developed cholestasis syndrome, which may be due to a block of the common bile duct and the development of reactive hepatitis.
In patients with alcoholic CP, an increase in liver function tests in the blood may be due to independent liver pathology (toxic hepatitis, liver cirrhosis). Hypocalcemia is often observed, the degree of which can serve as one of the criteria for the severity of the disease. Hypercalcemia suggests the presence of hyperparathyroidism as a causative factor of CP.
© I.V. Maev, A.N. Kazyulin, A.A. Samsonov, Yu.A. Kucheryavyi. Chronic pancreatitis: (Algorithm for diagnosis and treatment tactics). A manual for general practitioners, therapists, gastroenterologists: A textbook. – M.: GOU VUNMTs MH and SR RF, 2006. – p.
The educational and methodological manual was developed by the staff of the Department of Propaedeutics of Internal Diseases of the Faculty of Medicine and Gastroenterology of the Moscow State Medical University (head of the department - Doctor of Medical Sciences, Professor I.V. Maev): Doctor of Medical Sciences, Prof. I.V. Mayev, Doctor of Medical Sciences, Prof. A.N. Kazyulin, Doctor of Medical Sciences, Prof. A.A. Samsonov, Ph.D., Yu.A. Curly. Edited by prof. I.V. Maeva.
Disease prevention
To eliminate the risk of developing the consequences of pancreatitis, it is necessary to promptly consult a specialist for diagnosis and timely treatment of the disease. The following will also help avoid possible complications:
- balanced diet;
- reducing alcohol consumption;
- fractional meals (frequent meals of small portions of food);
- sufficient physical activity.
Taking medications wisely (do not overuse them) and avoiding stress will also help keep your pancreas healthy.
Sources: https://gastrotract.ru/bolezn/pankreatit/chem-opasen-pankreatit.html https://pankreatit03.ru/posledstviya.html gastrolekar.ru/pankreatit/chem-opasen.html netpankreatitu.ru/o-zabolevanii /opasnye-oslozhneniya.html https://ponosov.net/opasnye-posledstviya-pankreatita.html zhktok.ru/bolezn/pankreatit/oslozhneniya-hronicheskogo-pankreatita-i-ego-posledstviya.html https://peptic.ru/ pankreatit/vidy-i-prichiny-2/posledstviya-pankreatita.html This material is exclusively subjective and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/20/2020