Clinical signs of inflammation of the pancreas are difficult to distinguish from other diseases of the digestive tract; they all cause similar symptoms: abdominal pain, dyspepsia. In this case, blood tests for pancreatitis play a major role. Other tests, for example, examination of stool, saliva, and urine, determine the form of pancreatitis - acute or chronic. For a doctor treating pancreatitis, you need to know exactly whether you are dealing with an acute form of the disease or an exacerbation of a chronic inflammatory process in the gland.
blood test for pancreatitis
Methods for determining chronic pancreatitis
The pancreas produces enzymes that break down proteins, fats and carbohydrates, and also synthesizes the hormone insulin, which delivers glucose to the body's cells. Diagnosis of pancreatitis involves determining the concentration of digestive enzymes and gland hormones in the bloodstream.
- Amylase – is involved in the processing of carbohydrate foods (breaks down starch); A distinction is made between pancreatic amylase and general α-amylase (diastase).
- Trypsin and elastase – ensure the digestion of proteins.
- Lipase - breaks down fats; its deficiency is detected by an increase in cholesterol in tests.
Lack of insulin leads to increased sugar in the bloodstream.
tests for pancreatitis
Pancreatic enzymes normally become active only in the intestines. If the movement of pancreatic juice through the ducts to the intestines is difficult, some enzymes are activated in the organ itself, “digesting” it - an inflammatory process occurs. It can be sluggish and occur without pain, but is accompanied by degeneration of organ tissues that are deprived of secretory activity. Tests for chronic pancreatitis reveal pathological processes and functional insufficiency of the pancreas. If chronic pancreatitis is suspected, diagnosis includes the following laboratory tests;
- Complete blood count (CBC) – detects inflammation in the body;
- Biochemical analysis - the most important diagnostic test for pancreatitis - provides information on the content of digestive enzymes, as well as glucose and cholesterol in the blood.
- Urine analysis for diastase - may show a slight but prolonged excess of amylase in the urine - a sign of chronic pancreatitis; a decrease in amylase compared to the norm indicates degeneration of the gland tissue.
- Stool analysis: fatty grayish stool with undigested food remains indicates a dysfunction of the pancreas.
- Testing saliva for amylase levels will help differentiate acute from chronic inflammation.
Treatment of the chronic form consists of organizing proper nutrition and taking medications that correct secretory insufficiency of the organ. Sick people quickly understand whether they can eat spicy, fatty, salty foods. As soon as you break your diet for pancreatitis, after a few hours a painful attack begins, which must be distinguished from an acute form of inflammation of the pancreas.
What tests are taken for pancreatitis?
- General clinical blood test;
- Blood chemistry;
- Stool analysis;
- Urine analysis for amylase content.
These tests for pancreatitis are aimed at identifying inflammation, detecting the level and concentration of enzymes released by the pancreas into the blood, urine, and also determining two main functions that can be impaired to varying degrees: the production of enzymes for breaking down food and the production of hormones for carbohydrate metabolism - insulin and glucagon.
Diagnosis of acute pancreatitis
In acute inflammation, intensive destruction of the gland tissue by its own enzymes occurs, which is accompanied by poisoning and deterioration of the general condition of the body. Diagnosis of pancreatitis in its acute form begins with taking into account clinical manifestations. The main symptom is pancreatic colic - acute pain in the epigastric region, which can be so severe that the patient loses consciousness.
vomiting attack
The pain syndrome is aggravated by attacks of vomiting that do not bring relief. In such a situation, doctors prescribe tests that are necessary to establish the fact of inflammation in the body and assess the extent of damage to the gland. Standard tests for pancreatitis are marked “cito!”, and should be done as quickly as possible:
- complete blood count (CBC);
- blood biochemistry - characterized by a sharp increase in amylase content in the blood, since with such a pathology it is activated not in the intestines, but in the pancreas itself and enters the bloodstream;
- biochemical analysis of urine shows an increase in diastase sometimes by 200-250 times; to monitor the dynamics of acute inflammation, urine should be taken every three hours;
- A stool analysis in acute pancreatitis may indicate that the process of digesting food is disrupted.
increase in amylase
An increase in amylase in the blood is also characteristic of pathologies such as cholecystitis, diabetes mellitus, and pain syndrome of the “acute abdomen” type may indicate appendicitis, perforation of an ulcer and other diseases of the abdominal cavity. To clarify pancreatitis, differential diagnosis is necessary. Before recognizing acute inflammation, the pancreas is examined by other diagnostic methods. Ultrasound, MRI, radiography - determine the localization of the pathology, its nature (inflammation, cyst, tumor).
How to identify pancreatitis by symptoms?
Signs of pancreatitis most often appear after the pancreas is overloaded with abundant fatty and meat foods, spicy dishes, and alcoholic drinks. As a rule, pancreatitis in adults is accompanied or preceded by problems with bile secretion caused by cholelithiasis, cholecystitis, and bile duct dyskinesia. The connection is explained by the anatomical location of a single outlet in the duodenum. Symptoms of acute and chronic disease differ in intensity.
Manifestations of acute form
In acute pancreatitis or during an exacerbation of chronic pancreatitis, the main signs of inflammation are:
- Intense pain in the epigastric region radiating to the back, along the lower ribs, to the scapula, and chest. The pain is constant and is not relieved by painkillers and antispasmodics. Patients are excited, screaming, and in severe cases, shock with loss of consciousness is possible.
- Vomiting is repeated and painful, does not provide relief to the patient, and increases weakness.
- Bloating, difficulty passing gas and stool.
- Patients have a characteristic appearance: sunken eyes, pale face, bluish lips, and possible blue-red spots on the skin of the buttocks.
- An increase in temperature indicates an infected form of acute pancreatitis. It usually stays at 38 degrees, against this background a weak pulse and pronounced tachycardia are determined. Sharp “jumps” and drops in temperature indicate a purulent infection in neighboring tissues, peritonitis.
- Patients have a tendency to fluctuate blood pressure.
There may be complaints of dry mouth (lack of saliva), a pronounced white coating on the tongue.
Surgeons on duty in the hospital usually expect patients to arrive in the evening and at night on holidays
Symptoms of the chronic form
The chronic course of the disease causes digestive disorders. It reflects damage to the function of the pancreas and manifests itself:
- typical diarrhea, in which the mass of feces is increased, it is covered with a film of undigested fat, has a gray color and a foul odor;
- losing weight;
- abdominal pain that occurs periodically after a diet violation, does not have a clear localization, can be girdling in nature, and in some patients is absent;
- periodic nausea, single vomiting.
In chronically ill patients, there may be signs of disruption of the endocrine function of the gland (fluctuations of glucose in the blood), which is why tremors in the body, dizziness, feelings of hunger and thirst, and cramps in the muscles of the limbs appear. The symptoms of pancreatitis are very similar to other diseases of the abdominal cavity.
It is necessary to diagnose pancreatitis as early as possible, since the course progressively worsens the condition of the pancreas, leading to widespread necrosis and tissue melting, and damage to other organs. Differential diagnosis requires knowledge of the distinctive features of diseases with a similar clinical course.
The proximity of the pancreas to other organs and the solar plexus creates the effect of girdling pain during inflammation
Blood tests
Informative tests for pancreatitis are a blood test: blood is taken from a finger for a general analysis; from a vein - for biochemical.
General analysis
Data from a general analysis show the presence of an inflammatory process in the body. In acute pancreatitis, the blood formula changes significantly.
- The number of leukocytes sometimes increases tens of times. Normally, the leukocyte content is no more than 9∙109/l.
- The erythrocyte sedimentation rate (ESR) increases, its normal value is 15-20 mm/h.
- The hematocrit (the ratio of the volume of red blood cells and plasma) increases, the blood becomes thick due to an imbalance of water-salt balance and fluid loss. The normal hematocrit is 46-48%.
complete blood count for pancreatitis
With chronic inflammation of the pancreas, the following changes are noted in a blood test:
- the number of white blood cells sometimes even decreases, but usually there is a slight increase over a long period of time;
- ESR slows down;
- there is a decrease in hemoglobin levels - which indicates developing anemia against the background of exhaustion of the body. Normal hemoglobin level is 120-160 g/l
Blood biochemistry
During a biochemical blood test for pancreatitis, attention is paid to the following data:
blood chemistry
- the level of enzymes produced by the pancreas: diastase, lipase, trypsin;
- glucose content;
- the amount of proteins of the acute phase of inflammation (globulins, C-reactive protein);
- total protein concentration.
Complications in the development of pancreatitis are indicated in a blood test by low calcium levels, the appearance of tumor markers, and an increase in glycosylated hemoglobin.
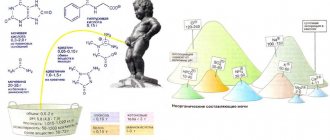
Pancreatic enzymes
When the pancreas becomes inflamed, its cells are destroyed, the enzymes that were in them enter the blood - their level increases sharply, which indicates the activity of the inflammatory process.
Amylase
The most characteristic sign of pancreatitis is a jump in amylase in the blood. At the very beginning of acute pancreatitis and in the first hours of relapses of a chronic disease, a rapid increase in pancreatic amylase in the bloodstream begins. This indicator reaches its maximum value by the end of the first day, then it decreases, and on the 4th-5th day it gradually normalizes.
amylase in the blood
It should be noted that the value of total amylase (diastase) does not always indicate the development of pancreatitis. This enzyme is produced by both the pancreas (P-type) and the salivary glands (S-type). An increase in α-amylase with normal P-type levels is not a sign of pancreatitis. In the chronic form of the disease, sometimes there is even a decrease in the enzyme in the blood, which may indicate deep damage to the gland cells that produce this secretion.
Lipase
As part of pancreatic juice, lipase enters the intestine, where it promotes the breakdown of dietary fats. Its content in the blood should be 20 thousand times less than in pancreatic juice. An increase in the level of lipase in the bloodstream - hyperlipasemia - means that fatty foods in the intestines are not completely digested, this leads to increased cholesterol in the blood, as well as changes in stool. Both of these signs, combined with an increase in lipase in the blood, make it possible to diagnose pancreatitis and other pathologies of the pancreas. The level of lipase in acute pancreatitis begins to increase on the second day from the onset of inflammation and remains at a height of 1.5-2 weeks, exceeding the norm by 5-10 times.
Currently, a radioimmunological method has been developed for the determination of trypsin and phospholipase in blood serum. With exacerbation of pancreatitis, phospholipase activation increases tens and even hundreds of times (at a norm of 2-7.9 ng/l, it reaches 400 ng/l). A low level of lipase indicates damage to gland cells that synthesize enzymes.
Proteases: trypsin and elastase
Proteases break down protein foods in the intestines; when the pancreatic ducts are disrupted, they enter the bloodstream instead of the digestive tract.
- The content of trypsin in the blood in acute forms of pancreatitis increases compared to the norm by 12-70 times - on the first day of illness, and then quickly decreases to normal levels. The chronic course of the disease is accompanied by a low level of trypsin (2-10 times lower than normal), which is an indicator of the death of gland cells that secrete enzymes.
- Elastase is an enzyme that, in acute pancreatitis, remains at a high level for 7-10 days of the disease. At this time, in many patients, the content of lipase and amylase already returns to normal, but the amount of elastase remains significant in 100% of patients with pancreatitis. The higher the concentration of elastase in the blood, the more iron is affected by inflammation, the larger the area of necrosis and the worse the prognosis of the disease. In chronic pancreatitis, diagnosis is carried out by the elastase content in the stool; its low content indicates a weakened ability of the gland to synthesize digestive enzymes.
Glucose level
If inflammation engulfs the endocrine cells of the gland that synthesize insulin, against the background of its deficiency, an increase in blood sugar occurs. Without insulin, glucose cannot be absorbed by the body's cells. The glucose level is very important, since diabetes is one of the common complications of pancreatitis. A more accurate indicator is glycated (glucose-bound) hemoglobin, which gives an idea of the blood sugar level over three months.
glucose level
Protein content
With pancreatitis, the protein content in the blood changes.
- The amount of acute phase proteins (C-reactive protein, fibrinogen) increases - they appear in the blood during any inflammatory processes. With successful relief of inflammation, their number decreases.
- The concentration of total protein and albumin decreases - this is associated with digestive disorders: food entering the intestines is not completely digested due to a lack of enzymes, is not absorbed into the blood, but leaves the body with fecal residues. This indicator is especially characteristic for chronic pancreatitis.
Other indicators
In some cases, other indicators are used to diagnose pancreatitis.
- With inflammation of the pancreas, the concentration of the enzymes ALT (alanine aminotransferase) and AST (aspartate aminotransferase) increases. Normally, these compounds are inside cells, participating in protein metabolism. With pathological destruction of cells, enzymes enter the bloodstream. An increase in ALT and AST in the blood is a sign not only of pancreatitis, it also accompanies diseases of the liver, heart, and severe muscle injuries. In combination with other symptoms of pancreatic pathology, ALT and AST indicators are used to clarify the diagnosis. In acute pancreatitis, the concentration of AST exceeds the norm by 2-5 times, and the ALT enzyme - by 6-10 times.
- Determination of tumor markers in the blood is prescribed to exclude a serious complication of pancreatitis - pancreatic cancer. Specific proteins for gland pathology are CA 19-9 and CEA (carcinoembryonic antigen), which are produced by degenerated cells. An increase in C 19-9 by three times and CEA by two times is a sign of pancreatitis; if these indicators are exceeded, they indicate the possible development of a malignant tumor in the gland. In some cases, a positive result for tumor markers indicates diseases of the liver, stomach, and not the pancreas.
- An increase in bilirubin is observed in the case of an increase in the size of the inflamed pancreas, which impedes the outflow of enzymes from the gallbladder.
Analysis of urine
Analysis of urine
A biochemical urine test is informative in diagnosing pancreatitis. The color of urine becomes a sign of the disease: the light yellow color changes with inflammation to dark yellow or brown. In urine analysis, an increase in diastase is observed. The more active the inflammatory process, the sharper the level of total amylase in the urine rises. This indicator is characteristic not only of acute pancreatitis; amylase in the urine also increases in diabetes mellitus. Severe inflammation is accompanied by ketone bodies, leukocytes and red blood cells present in the urine. Protein is found in urine when its absorption in the intestine is impaired. In the acute course of the disease, urine must be taken repeatedly to monitor the dynamics of amylase in the body.
Urinalysis in chronic gland disease shows a decrease in the level of α-amylase, which is associated with a weakening of the secretory functions of the gland during long-term pathology.
What other tests can be prescribed?
As mentioned above, it is necessary to undergo a comprehensive laboratory examination.
Additionally, the tests determine immunoreactive trypsin for pancreatitis. But it should be noted that if the indicator is positive, this does not always indicate pancreatitis. A positive result additionally indicates cholecystitis or, for example, persistent renal failure.
To identify not only pancreatitis and other diseases, including disorders, it is necessary to determine trypsinogen in a urine test. The examination is expensive, but it also allows us to make an accurate diagnosis with a fairly high guarantee.
It is mandatory to undergo a stool test, which helps determine the exact functional level of the pancreas. When important enzymes decrease, the patient’s entire fat digestion process begins to suffer.
Main characteristics of feces during inflammation of the pancreas:
- Fat is clearly visible in stool analysis.
- Undigested food remains may be detected.
- Light-colored feces indicate blockage of the bile ducts.
Violation of exocrine function can be determined independently. In this case, feces are poorly washed off the walls of the toilet, have a fairly shiny surface and have a persistent, unpleasant odor. Often at the initial stage of pancreatitis there is loose and frequent stool. Such signs should alert a person and they should immediately consult a doctor.
Also read on our website: Treatment of chronic pancreatitis at home
Now you know why you need to take tests and what they mean for making a diagnosis. Remember, the sooner you detect the first signs of the disease, undergo laboratory testing, a variety of instrumental methods and appropriate treatment, the greater the chance of avoiding health complications.
Stool analysis
stool analysis
If you have symptoms of inflammation of the pancreas, you need to submit your stool for examination to clarify the diagnosis. To get reliable results, take tests after a dietary meal. You need to consume 105 g of protein food, 180 g of carbohydrate food, 135 g of fat. Stool analysis for pancreatitis provides information about functional disorders of the pancreas.
- The increased fat content makes the stool shiny, with a pasty consistency and high in fatty acids - evidence of a lack of the lipase enzyme in the intestines.
- Changes in stool also affect its color: with pancreatitis, it acquires a grayish tint.
- The presence of undigested residues indicates a general lack of enzymes in the intestines.
- A decrease in the level of elastase-1 in the feces shows how much the secretory function of the pancreas is reduced. In severe cases, fecal elastase levels drop below 100 mcg/g.
Interpretation of biochemical analysis
The final formulation of the diagnosis is made on the basis of research: laboratory and instrumental. When diagnosing inflammation of the pancreas, the main thing is a blood test for pancreatitis; it gives indicators of abnormalities in pancreatic enzymes:
- the level of pancreatic amylase in the blood should not exceed 54 units; with pancreatitis, it increases sharply on the first day of the disease;
- normal lipase content is up to 1.60 units/l, with acute pancreatitis it increases 5-20 times;
- The normal trypsin content is 10-60 μg/l, an increase indicates acute inflammation, a decrease indicates a chronic process.
- The upper limit of normal elastase in the bloodstream is 4 ng/ml; the higher its excess, the more severe the form of the disease.
Laboratory examination provides other informative indicators.
- The sugar content in the bloodstream should not exceed 5.5 mmol/l; with pancreatitis it increases.
- The total protein content in healthy people is 64 g/l; its decrease indicates pathology of the pancreas, lack of nutrition or intestinal diseases.
- Protein norm CA 19-9 – up to 34 units/l; exceeding the level is a sign of pancreatitis, a significant increase is a suspicion of oncology.
- The normal level of cholesterol in the blood is 6.7 mmol/l; in men its level is higher than in women. With diabetes mellitus and pancreatitis, cholesterol levels increase.
- AST and ALT enzymes are normally up to 41 mmol/l; if the level is elevated, there is reason to diagnose pancreatitis.
With a variety of diagnostic methods and indicators, the value of pancreatic amylase on the first day of the disease and the determination of lipase and elastase in subsequent days are informative for the attending physician.