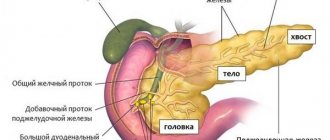
Pancreatitis is a disease that develops against the background of pancreatic dysfunction. The reason for this is the penetration of bacteria into the organ from the duodenum, blood, bile ducts, and also as a result of the negative influence of provoking factors from the outside. One of the common types of pathology is parenchymal pancreatitis. This is a chronic form of the disease, the development of which is caused by damage to the organ parenchyma with progressive factors, which, if left untreated, leads to its atrophy.
Parenchymal form of pancreatitis - what is it?
This form of the disease is characterized by a sluggish inflammatory process, the cause of which is a disruption in the synthesis of enzymes produced by the pancreas. Excessive enzyme concentration provokes self-digestion of parenchyma tissues, followed by scarring and wrinkling.
As a result, diffuse changes in the organ occur. This is expressed in the gradual replacement of the affected areas of tissue with connecting segments, followed by loss of functionality of the pancreas. As a result, the synthesis of digestive enzymes in the body decreases.
In medicine, there are two types of inflammatory process of the parenchyma:
- diffuse (extensive) - affects most of the area;
- limited - the head or tail is partially affected.
The danger of parenchymal pancreatitis is that it is difficult to diagnose at the initial stage of development. This is due to the fact that the disease does not have pronounced symptoms and only sometimes manifests itself in minor periods of exacerbation. As a result, the disease gradually progresses and, in the absence of adequate therapy, can lead to pancreatic atrophy.
Biliary-dependent pancreatitis: symptoms of the acute form of the disease
This disease develops slowly, sometimes over the course of a whole year. But under the influence of one factor or another, the disease can worsen.
In such cases, very characteristic symptoms arise:
- Severe nausea.
- Vomiting that is almost impossible to stop.
- Increased body temperature.
- Sharp pain localized in the right hypochondrium (sometimes of a girdling nature).
- Stool disorders (both severe diarrhea and constipation are possible).
- Yellowness of the skin.
Basic forms
Parenchymal pancreatitis is divided into three main forms. Each of them is characterized by certain clinical signs and the course of the pathological process:
- Edema. This form develops due to excessive accumulation of fluid in the tissues of the organ. The provoking factor is dietary errors, which is aggravated by alcohol. In rare cases, the edematous form develops as a complication of pathologies of the digestive tract. Clinical signs are expressed due to severe intoxication. Treatment does not require surgery and has a favorable prognosis.
- Sclerosing. It develops against the background of blockage of the glandular ducts, less often due to concomitant diseases of the digestive system. This form is characterized by the formation of sclerotic changes in the organ, which leads to a significant expansion of its ducts. Common symptoms of damage: pain in the left hypochondrium, the presence of glucose in the urine, frequent urge to urinate, thirst. 5% of diagnosed cases develop completely asymptomatically. Traditional treatment methods are used for treatment.
- Calculous. It is characterized by the deposition of insoluble calcium salts in the glandular ducts, which can cause complete blockage of the lumen. This form progresses significantly and can provoke the formation of a malignant tumor.
Possible complications
Chronic biliary-dependent pancreatitis is a dangerous disease that, if left untreated or if therapy is started too late, can lead to the development of a host of dangerous complications:
- Cysts may form in the pancreatic tissue.
- The disease sometimes leads to the development of an abscess (a collection of pus).
- The list of dangerous complications includes diabetes mellitus, since the pancreas is also responsible for the production of insulin.
- In some patients, pancreatitis is associated with obstructive jaundice.
- In severe cases, as a result of inflammation, sclerosis (proliferation of non-functional tissues) or necrosis (death of cells) of the gland develops.
Subtype with exocrine insufficiency
In addition to the morphological forms of the disease, experts distinguish two subtypes. Each of them is characterized by certain pathological changes that lead to partial or complete loss of pancreatic functionality.
The diagnosis of “parenchymal pancreatitis with exocrine insufficiency” is established when the synthesis of digestive enzymes decreases. As a result of damage, the organ is not able to produce the necessary enzymes in sufficient quantities. This provokes their deficiency in the body, which negatively affects the functioning of the digestive organs.
Laboratory and instrumental tests, which are confirmed by the patient’s complaints, help to identify the subtype of pathology.
Symptoms and signs of pathology
Like any other pathological process in the human body that has a chronic course, the parenchymal form of pancreatic lesions of the pancreas occurs in cyclical periods: moments of exacerbation are followed by remissions and in the reverse order.
During periods of remission, the patient feels complete comfort within himself, and the pathology does not continue to progress. But, over time, a period of exacerbation begins, accompanied by a whole complex of pathological signs. Symptoms of chronic parenchymal pancreatitis manifest themselves as follows:
- sharp painful sensations appear in the epigastric region with a characteristic encircling character,
- disorders of the dyspeptic system of organs begin to develop, expressed by the formation of a feeling of nausea and the discharge of intense vomit, as well as the development of constipation or diarrhea,
- active loss of body weight against the background of impaired absorption of nutrients and fear of the occurrence of painful symptoms after eating, against the background of which the patient loses appetite,
- a concomitant pathology begins to develop against the background of reduced insulin levels, called diabetes mellitus.
The chronic nature of the course of this disease during the initial examination of the patient will be indicated by the facts that the manifestation of the above symptomatic signs occurs periodically, after certain periods of time.
And, only the results of an ultrasound examination will indicate the development of the parenchymal form of pancreatic lesions of the pancreas.
During periods of exacerbation of pathology, excretory functional insufficiency of the gland may manifest itself with the following symptoms:
- heaviness in the abdominal area,
- lack of appetite,
- unpleasant smell of feces and the content of undigested food in them.
With exocrine pancreatic insufficiency, the patient progresses to the development of malabsorption against the background of a pathological disorder in the breakdown of food into necessary elements.
Chronic parenchymal biliary-dependent pancreatitis - what is it?
Another common subtype is biliary-dependent, which needs close attention. It accounts for 50% of detected cases of pancreatitis. The development of parenchymal biliary-dependent pancreatitis is a consequence of hepatobiliary disorders of various types.
The disease is closely related to low-grade inflammation of the pancreas, which develops against the background of congenital and acquired pathologies of the organ.
Chronic parenchymal biliary-dependent pancreatitis - what is it? This disease is characterized by a partial or complete decrease in the efficiency of the gland to produce digestive enzymes and hormones.
With biliary-dependent pancreatitis, the outflow of bile from the duodenum occurs back into the pancreatic ducts. This ultimately leads to a change in tissue structure. This subtype is characterized by constant relapses, which threaten serious health complications. A characteristic sign of pathology is a constant or frequent feeling of bitterness in the mouth.
Possible complications due to the development of parenchymal biliary-dependent pancreatitis:
- blockage of the bile ducts;
- diabetes;
- further spread of the inflammatory process to adjacent organs and tissues;
- enzyme deficiency, which leads to malfunction of all digestive organs.
With biliary-dependent pancreatitis, a critical decrease in the functionality of the pancreas of up to 70% is possible.
What is biliary pancreatitis
This type of pancreatic lesion of the pancreas, which has a code according to ICD 10 K85.1, is a secondary disease that has an inflammatory nature and forms against the background of an already occurring primary disease. Primary pathologies are localized mainly in the area of the liver, gallbladder or bile ducts.
A long period of primary pathologies helps to maximize the likelihood of developing a disease such as chronic biliary-dependent pancreatitis, and in most cases, the development of this disease is facilitated by cholelithiasis with the presence of small stones in the gallbladder ducts.
Features of the disease
The development of the biliary form of pancreatic damage to a parenchymal organ begins from the moment when bile fluid is released into the cavity of the pancreatic ducts and the activation of the inflammatory process, which is evidence of a malfunction in the functioning of the gallbladder.
In a healthy body, the pressure level in the bile ducts is less than the pressure in the cavity of the pancreatic ducts, which completely eliminates the possibility of bile entering the pancreatic duct. An increased level of pressure in the biliary tract indicates the formation of some kind of obstacle in the cavity of the bile ducts or in the area of the papilla of Vater, in the form of a stone, tumor-like formation, or helminthic infestation that does not allow bile to pass into the intestinal cavity. This leads to the reflux of bile into the cavity of the pancreatic ducts and the development of biliary pancreatic disease.
Causes and mechanisms of disease development
The main reasons contributing to the development of chronic biliary-dependent pancreatitis are the development of the following primary pathological diseases:
- cholelithiasis, as well as biliary sludge, characterized as thickening of bile with the formation of sediment in the form of microscopic calcifications,
- congenital anomaly of the bile duct,
- progression of chronic cholecystitis,
- hepatic exocrine insufficiency,
- the occurrence of dyskinesia of the bile ducts or gallbladder,
- cystic lesion of the bile duct (choledochus), which facilitates the removal of bile from the cavity of the gallbladder and hepatic duct,
- progression of cholangitis,
- congestive cholestasis, characterized as stagnation of bile,
- formation of liver cirrhosis,
- pathological impairment of the functionality of the nipple of Vater, which ensures the entry of bile into the cavity of the duodenum.
The negative impact of the development of the above pathologies during the formation of the biliary pancreatic process in the parenchymal gland provokes the development of the following pathological disorders:
- the occurrence of an inflammatory process,
- violation of the integrity and functioning of the glandular structure of the pancreas,
- activation of degenerative processes,
- development of connective tissue proliferation.
Symptoms and manifestations of biliary pancreatitis
This pathological process in the pancreatic cavity can have two forms of development - chronic and acute. Acute biliary pancreatitis has a similar clinical picture to exacerbation of chronic biliary pancreatitis, and has common pancreatic manifestations, including:
- painful sensations localized in the left hypochondrium with a characteristic girdling character,
- regular feeling of nausea with intense vomiting,
- increase in body temperature to subfebrile limits and above,
- icteric rashes on the skin,
- the appearance of constipation, diarrhea and the development of gas formation.
Chronic biliary pancreatitis with unstable remission also has a range of typical symptomatic signs:
- loss of appetite,
- the occurrence of nausea,
- discharge of vomit against the background of pain that occurs when the diet is violated,
- chronic form of constipation or diarrhea,
- weight loss,
- temperature rise to subfebrile limits.
But, despite the many similarities between biliary pancreatitis and other varieties of this disease, this pathology has its own characteristic features:
- The occurrence of a feeling of pain in the abdominal area is caused by the use of medications with a choleretic spectrum of action, as well as food products that have the same effect.
- Attacks of pain last much longer than with other forms of gland disease.
- The biliary form of the disease is characterized by the fact that during its development, in most cases, paresis occurs in the intestinal area, that is, constipation develops, while other types of the disease provoke the development of diarrhea.
- Pain is mainly manifested by symptomatic signs characteristic of the development of biliary colic, manifesting itself in the hypochondrium on the right, and not on the left.
- It is the biliary form of pancreatic disease that often occurs in combination with the development of jaundice.
- Quite often, patient complaints include the regular occurrence of belching with a bitter taste, as well as the appearance of bitterness in the mouth.
Alarming symptoms
Pathological signs of the disease are often quite difficult to recognize, since they are similar to many diseases of the digestive tract. At the same time, the symptoms are not bright, which many people simply do not pay attention to.
Symptoms of parenchymal pancreatitis:
- Dull pain in the left hypochondrium with radiation to the back, most often felt after eating spicy and fatty foods, alcohol and as a result of overeating.
- Nausea with frequent bouts of vomiting.
- Stool disorder, with constipation alternating with diarrhea, stools are characterized by a fetid odor, have a mushy consistency and undigested food residues.
- Excessive flatulence.
- Constant drowsiness, absent-mindedness, which makes it impossible to concentrate on work.
- Significant weight loss, which occurs as a result of a lack of digestive enzymes, so many nutrients are not able to be absorbed by the body and pass through in transit to the exit.
- Increased dryness of the skin, red spots in the abdominal area, which is caused by hypertrophic changes in the subcutaneous fat layer.
The appearance of two or more pathological signs is a reason to consult a doctor and undergo an examination. You should not immediately invent a diagnosis for yourself, since these symptoms are characteristic of many pathologies. And only an experienced specialist is able to identify the reasons for their appearance.
Symptoms of parenchymal pancreatitis
Symptoms of the disease are very diverse. How chronic parenchymal pancreatitis will manifest itself in each specific case depends on the general condition of the body, its immune forces and concomitant pathologies, the presence or absence of a violation of the exocrine function of the pancreas.
The symptoms of inflammation of the pancreas in different forms of pathologies are largely similar, but there are still differences between them. In general, chronic parenchymal pancreatitis can be suspected in the presence of conditions such as:
- Pain syndromes (Mayo-Robson symptom). The pain is dull, aching, predominantly localized in the left hypochondrium, radiating to the back. Their manifestation increases with overeating, eating hot, spicy and fatty foods or after drinking alcohol.
- Nausea, vomiting and stool upset. Diarrhea alternates with constipation, stools are mushy, with a greasy sheen (steatorrhea), foul odor and food residues. This is a classic sign of enzyme deficiency.
- Lack of appetite and weight loss. This is due to poor absorption of nutrients due to a sharp decrease in enzyme production. Many vital substances that make up food (proteins, fats and others) pass through in transit and are not absorbed by the body.
Along with the listed signs, the patient in this situation has skin hyperesthesia (Kach's symptom) and hypotrophic changes in the subcutaneous fatty tissue.
Detection of such conditions is a reason to contact a specialist. To make an accurate diagnosis, the patient needs a complete examination, which is possible only in a specialized institution.
The main, most important symptoms for diagnosing pancreatitis are:
- Moye-Robson symptom: sharp pain in the left corner between the ribs and spine;
- Kach's symptom: pain on palpation in the area of the spinous processes of the thoracic vertebrae (9-11 on the right and 8-9 tears);
- Grotta's symptom is hypotrophy of subcutaneous fat to the left of the navel in the area of the projection of the pancreas.
The general clinical picture can consist of any combination of the following symptoms:
- the appearance of pain: if the head of the gland is affected - in the epigastric or right hypochondrium, the body - in the epigastrium, more on the left, the tail - in the left hypochondrium;
- vomiting, nausea, loose stools (may alternate with constipation in particularly severe cases);
- the foul odor of feces is a consequence of a violation of the exocrine function of the gland;
- increased salivation;
- sudden weight loss;
- Diabetes mellitus may develop against the background of the disease (in this case, increased appetite and thirst will occur);
- aversion to fatty foods;
- hemorrhagic rashes on the skin (look like bloody drops with a diameter of up to 5 mm).
Reasons for development
Chronic parenchymal pancreatitis develops under the influence of certain provoking factors.
The most common of them are:
- cholecystitis, as a result of excessive deposition of cholesterol on the walls, the gallbladder becomes inflamed and swollen, which leads to a decrease in the outflow of acid and its reflux into the bile ducts;
- urolithiasis, as a result of which the acid outflow pathways are partially or completely blocked;
- formation of tumors of benign and malignant properties;
- decreased motility of the biliary tract;
- excessive consumption of alcohol, as well as fatty and salty foods;
- deficiency in the diet of proteins and vitamins;
- regular stress;
- failure of thyroid function;
- uncontrolled use of medications;
- regular frostbite or heatstroke;
- organ injury;
- chronic diseases of the digestive system.
In some cases, parenchymal pancreatitis develops as a complication after suffering from influenza, scarlet fever, or tonsillitis.
The main causes of the development of the disease. List of primary diseases
As already mentioned, biliary-dependent pancreatitis is not an independent disease.
Inflammation and damage to gland tissue is directly related to the development of certain pathologies.
- Gallstone disease (formed stones can disrupt the flow of bile).
- Violation of the contractile activity of the gallbladder often leads to reverse reflux of bile.
- Congenital anomalies in the structure of the bile ducts.
- Inflammation of the gallbladder, including its chronic forms.
- Papillitis is an inflammation of the papilla through which bile enters the cavity of the duodenum.
- Persistent spasm of the muscles of the papilla.
- Cirrhosis and some other liver diseases.
- Blockage of the duodenal papilla by a tumor, stone, cyst or parasite bodies (for example, roundworms).
Diagnostics
To identify pathology, the doctor first conducts a survey of the patient for the presence of characteristic signs. In addition, examination with palpation and percussion is used, which makes it possible to identify a painful area in the left hypochondrium.
To confirm the diagnosis, the following types of tests and studies are prescribed:
- blood test to determine the level of red blood cells, white blood cells, enzyme concentrations, as well as to determine the level of calcium, sodium and potassium;
- examination of stool for the content of certain enzymes and fragments of undigested food;
- urine analysis to detect microhematuria, proteinuria, cylindruria;
- Ultrasound is the most informative method for identifying diffuse changes in the pancreas;
- CT with contrast pigment allows you to accurately determine the presence of stones in the bile ducts.
Diagnostic criteria for pancreatitis
Diagnosis of pancreatitis begins with a survey, as well as a comprehensive examination in a clinic. Let's look at the changes specific to pancreatitis:
- Stool analysis for scatology - stool analysis reveals undigested food fibers, as well as the presence of fatty droplets;
- Biochemical blood test - increased amylase levels;
- Urinalysis for amylase – level increases several times;
- Ultrasound examination of the abdominal organs (ultrasound examination of the abdominal organs) reveals diffuse changes in the pancreatic parenchyma. In biliary-dependent pancreatitis, chronic inflammation of the gallbladder, its ducts and possibly stones is also detected.
- Blood test for glucose - quite often, with parenchymal damage to the pancreas, its secretory apparatus is also affected. Thus, insufficient insulin production develops and type 2 diabetes develops.
In a clinical analysis of blood and urine, as a rule, there are no changes specific to pancreatitis.
How to treat?
Treatment of chronic parenchymal pancreatitis is carried out in accordance with the identified stage of the pathology. At the initial stage, it is enough to carry out the prescribed course of drug therapy and subsequently adhere to a certain diet in order to fully restore health.
If the pathology is advanced, which has led to irreversible consequences for the pancreas, surgery is prescribed to cut off the affected area in order to prevent further deterioration of the situation.
Treatment
Parenchymal pancreatitis is a pathology that can occur without symptoms and worsen, so treatment is most often aimed at preventing recurrence. If the patient has frequent exacerbations, then it is imperative to adhere to a diet. In the chronic form of pancreatitis, there are a number of rules and features of therapy that must be followed both during exacerbation and during remission, for the purpose of prevention.
The patient must follow the doctor’s recommendations:
- do not drink alcohol;
- remove fats from the diet as much as possible;
- reduce the calorie content of foods by reducing fat;
- separate meals;
- to drink a lot of water;
- moderate the consumption of salty, spicy and fried foods, or better yet, exclude such foods from the diet altogether.
Nutritional rules for restoring the pancreas
All products should be chosen as gentle on the stomach as possible, without spices, seasonings or large amounts of salt. It is better to eat boiled, stewed and steamed food. It is undesirable to use:
- yeast products;
- sweets;
- eggs;
- figs;
- dates;
- bananas;
- mushrooms;
- legumes
During the remission stage, the patient also needs to undergo sanatorium-resort treatment. During such therapy, the patient needs to do the following procedures:
- drink a lot of mineral water;
- stick to a diet;
- psychotherapeutic treatment.
At the time of exacerbation, the patient’s diet becomes more restrictive. In the first few days of relapse, it is better for the patient to completely abstain from food and only drink water. From the moment your condition improves, you can gradually begin to eat familiar foods, but in a lighter version and in small portions. Foods should contain a lot of protein.
Chronic pancreatitis cannot be cured or alleviated without medication. Therefore, during the period of repeated inflammation, the doctor prescribes drug therapy to the patient.
During this treatment, a person is prescribed:
- proton pump blockers;
- H2-histamine receptor blockers;
- antispasmodics;
- anti-inflammatory;
- enzyme preparations.
All these medications are aimed at relieving inflammation and reducing pain attacks, and enzymatic preparations help digest the food eaten.
To treat a disease surgically, the doctor needs to have strong arguments. For example, drug treatment was ineffective or complications appeared. In this case, prompt assistance may be involved. During surgery, the doctor removes the affected part of the organ.
Treatment with herbs and other folk remedies can be used only after consultation with a doctor, especially at the stage of exacerbation. The following remedies can be used as part of home therapy:
- rosehip decoction;
- potato juice;
- buckwheat;
- various herbs.
Drug treatment
The selection of necessary medications is carried out by the attending physician based on the severity of the identified pathology. Their dosage and course of administration are prescribed taking into account the individual characteristics of the patient.
The main types of medications that are used to treat parenchymal pancreatitis:
- drugs that reduce the production of gastric juice (Omeprazole, Ezameprazole);
- antispasmodics for pain relief (“No-Shpa”, “Papaverine”);
- prokinetics that improve intestinal motility and promote the rapid passage of food bolus (Domperidone, Metoclopravid);
- replacement drugs that replenish the resulting enzyme deficiency.
Biliary-dependent pancreatitis: treatment with medications
The treatment regimen is drawn up individually, as it depends on the general condition of the patient, the form of pancreatitis and the reasons for its development.
Treatment methods may be:
- During exacerbations, the patient is administered nutrient solutions, since eating normal food is contraindicated.
- Since acute pancreatitis is accompanied by severe pain and vomiting, the patient is prescribed analgesics and antiemetic drugs.
- Antisecretory medications are used to reduce the production of gastric juice.
- Antibiotics are prescribed to prevent infectious diseases.
- It is also important to monitor the patient's condition during therapy, adjusting blood sugar levels as necessary.
- Outside of exacerbation, replacement therapy is carried out - patients take drugs that contain artificial enzymes. This helps normalize digestion processes.
Special diet
How to treat chronic parenchymal pancreatitis with diet? It will not be possible to get rid of pathology without appropriate adjustments to the diet. Therefore, it is recommended to adhere to the following dietary rules:
- Avoid alcohol, smoking, as well as fatty, salty, smoked, fried and spicy foods.
- Minimize your intake of sugar and salt.
- All food should be boiled and steamed, and it should be crushed to the consistency of puree.
- During an exacerbation, it is recommended to drink more jelly and compotes.
- Porridge should be cooked in water.
- Food should not be cold or hot.
- Almost all fruits can be consumed, but they should not be sour.
- It is forbidden to eat fresh bread. It is better to replace it with crackers, bread, crackers.
- Meat and fish should be lean. They should be boiled.
- Dairy products must have a fat content of less than 2%; the consumption of curd mass with a high sugar content and palm oil is not allowed.
- It is recommended to adhere to fractional nutrition, eating small portions 5-6 times a day.
- Dishes should be prepared from a small number of ingredients.
A strict diet for parenchymal pancreatitis should be followed for 1-2 months after the course of drug therapy.
Instrumental diagnostic methods
Test results can tell a specialist a lot. But it is impossible to make an accurate diagnosis without instrumental examination.
These methods include:
- Ultrasound is by far the most accessible diagnostic method. During the procedure, the doctor can determine the size of the pancreas, identify the presence of altered tissues, gallstones, and abnormalities in the structure of the bile ducts.
- Transabdominal ultrasonography. This is a non-invasive procedure that allows you to assess the condition of the pancreas and duodenal papilla (for example, during the study, its spasm or blockage can be detected).
- Endoscopic ultrasonography. It is carried out to assess the condition of the pancreas and duodenum. In this case, the probe is inserted directly into the stomach, which makes it possible to more closely examine the affected areas of the digestive tract.
- One of the most informative methods is magnetic resonance imaging. With the help of images, the doctor can carefully examine the pancreas, assess the condition of the liver, gallbladder and duct.
- During intravenous cholangiocholecystography, a specialist can carefully examine the structure and condition of the bile ducts. A special contract substance is injected into the patient's body, after which X-ray images are taken.
Sometimes additional studies are carried out to help study the functioning of the vessels that supply the abdominal organs.
Herbal therapy
Herbal medicine is also an effective method of treating this disease. Medicinal herbs are used during the period of remission to prevent relapses of the pathology. It is impossible to cure the pathology with purely medicinal preparations, since they are not capable of replacing the main treatment.
You can purchase ready-made mixtures of medicinal herbs at the pharmacy. But you can also prepare them yourself if necessary. To do this, you will need to mix the components in equal proportions.
Acceptable options for medicinal fees:
- wormwood, motherwort, St. John's wort, mint;
- cudweed, wormwood, St. John's wort, chamomile, yarrow;
- dill, mint, immortelle, hawthorn, chamomile;
- St. John's wort, wormwood, sage, elecampane, burdock root, calendula, horsetail.
To prepare the decoction, add 30 g of herbal mixture to 250 ml of boiling water. Leave for 40 minutes, peel. Drink the drink in equal portions throughout the day. Full course - 3 weeks.
Physical exercise to prevent exacerbations
Physical therapy also helps a person forget about pathology and return to their usual lifestyle. The most effective exercises are prescribed by the attending physician in accordance with the individual characteristics of the patient.
But there are several recommendations that should be followed:
- More physical activity, so it is better to give preference to walking, an exercise bike, and simple physical exercises.
- Do not use breath-holding exercises: squats, leg presses.
- It is prohibited to use compression belts during training.
- Eat food 60-90 minutes before starting exercise.
Symptoms
The chronic form of the disease involves a sluggish process, followed by acute attacks. Remission (apparent improvement of the condition), in which parenchymal pancreatitis practically does not manifest itself, is replaced by:
- Pain in the hypochondrium, most often on the left side or around the costal arches. Aching pain makes itself felt after overeating, eating fatty, spicy, salty foods. An overdose of alcohol can lead to the same consequences.
- Malabsorption. A lack of enzymes produced by the pancreas results in insufficient digestion of food. Weakness and lethargy are observed. The patient begins to lose weight.
- Dyspepsia. Appetite decreases. Stool becomes frequent. Nausea is felt, which may be accompanied by vomiting with a sour taste and smell.
- Symptoms characteristic of diabetes (feelings of thirst and hunger, dry skin, excessive sweating, etc.). The pancreas, which is the source of insulin, cannot cope with its duties, which leads to an increase in blood sugar.