Similar diseases
You can select the most appropriate treatment tactics if you know the diagnosis accurately. For this purpose, differential diagnosis of pancreatitis is carried out. It is important to be able to distinguish this disease from a number of others with similar symptoms. Such diseases include:
- pancreas cancer;
- peptic ulcer (perforated ulcers);
It is usually possible to determine which problem is causing certain symptoms only in the hospital. Doctors must know the characteristic signs of all diseases in order to accurately diagnose.
Differential diagnosis
The tumor can be detected in 85% of cases using computed tomography. But it is best to differentiate between cancer and pancreatitis using ERCP - endoscopic retrograde cholangiopancreatography.
Pancreatitis can be distinguished from a perforated ulcer by the patient’s behavior. In the first case, he will try to take one position and not move. With pancreatitis, patients are restless. In addition to pain, they experience vomiting.
You can figure out what exactly is bothering a person using an ultrasound. This study makes it possible to diagnose cholecystitis. With this disease, patients complain of pain on the right side, which extends to the corresponding shoulder. An inflammatory process is visible on ultrasound with cholecystitis.
Intestinal obstruction manifests itself in the same way as pancreatitis. These diseases can be distinguished by blood tests. This is why pancreatitis is diagnosed. Tests will show diastasis and increased chloride levels due to inflammation of the pancreas.
Classification of pancreatitis
To understand how inflammation of the pancreas manifests itself, you need to understand that it can be acute or chronic. In the first case, the symptoms are pronounced, and it is easy for the doctor to understand that the patient has acute pancreatitis. Diagnosis is mandatory, and only after confirming the doctor’s assumptions (using ultrasound and tests) is treatment prescribed.
Chronic pancreatitis is characterized by alternating periods of slight improvement/deterioration of the condition. In this case, the inflammatory process is sluggish. But it leads to atrophy of gland tissue.
Characteristics of acute inflammation
Laboratory diagnosis of pancreatitis is necessary to determine the severity of the disease. Acute inflammation can occur in a mild form. In this case, organs and systems are minimally affected. The disease is expressed in swelling of the gland. This type of pancreatitis is easy to treat, and patients recover quickly.
In severe forms of acute inflammatory process in the pancreas, pronounced disturbances are observed in various organs and tissues. In addition, the severe form may be accompanied by the following complications:
- pancreatic abscess (pus accumulates in the pancreas or surrounding tissues);
- acute false cyst - occurs 4 or more weeks after an attack of pancreatitis, characterized by the accumulation of pancreatic juice;
- pancreatic necrosis (tissue infection is also possible);
- acute accumulation of fluid in the peripancreatic space or in the gland itself.
This must be taken into account when diagnosing. Pancreatitis, in which tissue necrosis begins, can cause death. This usually occurs with the development of a purulent form of the disease.
Classification of acute pancreatitis
Clinicians share the classification of acute pancreatitis according to certain characteristics.
Also read on our website: Acute and chronic pancreatitis - differences
According to the severity of the disease:
- Easy.
- Average.
- Severe form.
With a mild course of the disease , short exacerbations may occur 1-2 times a year. Painful symptoms can be relieved with painkillers.
With moderate severity, exacerbations can occur 3 to 4 times a year. Note that signs of exacerbation can occur with a typical long-term pain syndrome. In a patient with moderate severity, pancreatic hyperfermentemia, creatorrhoea, amenorrhea, and steatorrhea are noted.
In severe cases , signs of exacerbation often occur, which are characterized by a long course. The pain syndrome has a pronounced course, the patient experiences diarrhea, a sharp loss of body weight, and disturbances in the exocrine function of the pancreas occur.
Clinicians share the classification of acute pancreatitis according to certain characteristics
If you do not provide assistance to the patient in a timely manner, there is a risk of serious complications. For example: partial stenosis of the duodenum occurs due to an enlargement of the head of the pancreas, obstruction of the common bile duct is noted, and pseudocysts are formed.
Recommendations from Elena Malysheva in the special issue “Live Healthy!” on how to overcome pacreatitis using the healing effects of natural remedies.
Additionally, acute pancreatitis is divided by scale, as well as by the nature of the lesion. 5 types in total :
- Edema acute.
- Sterile pencreatic necrosis.
- Infected course of the disease.
- Formation of pancreatogenic abscess.
- Formation of pseudocysts in acute pancreatitis.
The classification of the acute course of the disease is extensive. Therefore, doctors further divide into causal classification . For example:
- Nutritional reason.
- Biliary.
- Gastrogenic and also ischemic.
- Infectious or toxic-allergic cause of acute pancreatitis.
- Traumatic.
- Congenital.
As for the clinical form of acute pancreatitis, it is distinguished into interstitial, in which swelling of the pancreas occurs, and the tissue often swells. The second clinical form is necrotic, the disease occurs with severe inflammation, and complications often occur.
Variants of chronic inflammation
Experts distinguish two subtypes of chronic pancreatitis. It can be primary or secondary. In the first case, inflammation begins directly in the pancreas. Secondary chronic pancreatitis develops against the background of other diseases of the digestive system. It is a complication.
With this disease, inflammation can either decrease or begin to develop with renewed vigor. But this is not as harmless as it might seem at first glance. A competent diagnosis of chronic pancreatitis is necessary, because it can lead to tissue atrophy, the pancreas calcifies over time, and its normal tissues are replaced by scars.
Classification of chronic pancreatitis
According to statistical data, it was noted that the chronic course of the disease most often occurs in patients. The disease has a specific clinical picture, which can subside and reappear.
Chronic pancreatitis is a fairly common disease, which is manifested by constant or periodic pain and signs of exocrine and endocrine insufficiency.
Based on morphological characteristics, doctors distinguish several trends:
- Interstitial, the second name for the edematous type of pancreatitis. In this case, swelling of the intercellular lobes in the pancreas occurs. At this stage, no pronounced destruction occurs. But, if assistance is not provided in a timely manner, this can lead to necrosis.
- Indurative chronic , most often develops after an “experienced” exacerbation. With this course of the disease, fibrosis is formed, and in rare cases, calcification of the pancreas is observed. The main symptom that indicates the presence of indurative pancreatitis is parenchymal damage, which is detected through a diagnostic examination.
- Chronic parenchymal , for which the character is wavy. For example: remissions can give way to exacerbations, and then the patient experiences tissue scarring. Against this background, the patient’s patency of the ducts is impaired, thereby changing not only the endocrine, but also the secretory function. If help is not provided in a timely manner, insulin synthesis is disrupted, and serious problems with the entire digestive process may occur.
- Cystic chronic. With this course, the patient experiences a disturbance in the outflow of pancreatic juice, and a cicatricial narrowing of the ducts also occurs. In severe cases, there is dilatation of the main pancreatic duct itself.
- Pseudotumorous. It is characterized by hypertrophy of the parenchyma, and an increase in the size of the affected organ is also observed. The clinical picture is pronounced, the patient has signs of jaundice, and dyspeptic symptoms are noted. Pseudotumorous pancreatitis is detected using ultrasound or CT.
Also read on our website: Reactive pancreatitis in children: symptoms and treatment
At this stage, the classification of chronic pancreatitis does not end. Additionally, several stages of remission and exacerbations . For example:
- There are sudden or frequent relapses of the disease.
- There are constant signs of the disease, in medicine it is called persistent chronic pancreatitis.
As for the clinical picture of this disease, a certain classification is also noted here.
- Pronounced pain syndrome.
- A pathological process occurs in which the activity of the stomach is disrupted (hyposecretory syndrome).
- Emotional and mental disorders - hypochondriacal syndrome.
Additionally, doctors note latent and combined signs of chronic disease. In the latent form, the patient does not have a pronounced pain syndrome, but dyspeptic disorders are noted, for example: nausea appears, the patient belches the food he has eaten. With a latent symptom, feces take on a mushy form. At the time of diagnostic laboratory examination, a violation is detected not only externally, but also in the intrasecretory function of the pancreas.
Symptoms of acute pancreatitis
You can figure out when you need to see a doctor if you know the signs of the onset of an active inflammatory process. These include severe pain symptoms. Most patients point to the epigastric region (left hypochondrium). The pain is girdling and can radiate to the area of the left shoulder blade. Lying on your back only intensifies it. The condition worsens after drinking alcohol, fatty, fried or spicy foods.
In addition to pain, there are other signs that indicate that acute pancreatitis has begun. Diagnosis and treatment must be carried out in a hospital inpatient setting. This will allow you to establish the diagnosis as accurately as possible and reduce the time required to restore your health. Symptoms of this disease are:
- vomiting that does not bring relief (may be uncontrollable);
- moderate yellowness of the sclera, in some patients the skin may look yellowish;
- hemorrhages in the navel area, bluish spots on the body;
- bloating, flatulence.
The disease is also indicated by abnormal bowel movements, the appearance of excessive fatigue, decreased blood pressure, pallor of the skin and increased sweating. Patients often complain of dry mouth; upon examination, a white coating is visible on the tongue.
Signs of chronic inflammation
You can understand that you have problems with your pancreas not only by uncontrollable vomiting and severe pain. Some people may suffer for years and not realize that they have chronic pancreatitis. Diagnosis and treatment will be complete if the patient goes to the hospital in a timely manner.
The development of chronic pancreatitis is indicated by:
- periodic pain localized in the left hypochondrium, often radiating to the back area;
- periodic feeling of nausea;
- diarrhea, which causes a characteristic odor;
- sudden weight loss;
- deterioration in health after eating fatty, fried, smoked foods.
If pancreatitis is not treated, the patient will experience weakness and dizziness. Some may even develop type 2 diabetes, memory deterioration becomes noticeable, and breathing problems appear.
Patient's complaints
With this disease, the patient complains of intense pain. The symptom occurs approximately 30 minutes after eating fried food or drinking alcohol.
The pain is usually localized in the epigastric region or in the left hypochondrium. In acute pancreatitis, they are localized in the upper half of the abdomen and are often encircling in nature.
The pain may radiate to the lumbar region or to the shoulder blade. Note that the pain symptoms are long-lasting, so it cannot be relieved with simple analgesics.
The patient begins to complain of belching, vomiting, and frequent loose stools. Since with pancreatitis the entire digestive system is disrupted, the patient experiences the above-described symptoms against the background of duodenal atony.
Due to the backflow of pancreatic juice, the patient experiences an unpleasant bitter taste in the oral cavity.
Additional complaints:
- Weakness appears.
- There is a loss of body weight.
- Avitaminosis.
Such signs in a patient occur against the background of enzyme deficiency. Therefore, at the time of diagnostic examination, a thorough analysis of pancreatic enzymes is carried out in order to further correct this process.
Laboratory diagnostic methods
When patients are admitted with suspected pancreatitis, they are prescribed a comprehensive examination. First of all, a biochemical blood test is done. It allows you to determine the type of disease, thanks to this test a more accurate diagnosis of pancreatitis is carried out. Analyzes make it possible to clearly present the picture of the disease.
With inflammation of the pancreas, the level of alpha-amylase and lipase increases, and the activity of C-reactive protein increases sharply. If the disease is accompanied by a malfunction of the kidneys, then the level of urea in the blood increases. At the same time, you can see a decrease in the amount of proteins, including albumin. The amount of insulin also noticeably decreases, causing glucose levels to rise.
Water and electrolytic analysis allows you to determine how much the composition of the blood has changed. A decrease in fluid levels can cause blood clots and blockage of small vessels. This analysis also allows you to determine the concentration of minerals: potassium, sodium, calcium. They are responsible for the normal functioning of the heart and blood vessels.
A general blood test gives an idea of the nature of the disease. Pay attention to the level of leukocytes and erythrocytes. Without this examination, a full diagnosis cannot be carried out.
Pancreatitis is also diagnosed by urine analysis. In this disease, the level of alpha-amylase deviates significantly from normal. But this is observed only in the initial stages of the disease. As pancreatitis progresses, red blood cells, white blood cells and other components may be found in the urine.
Types of diagnostics
Various methods will help identify this disease.
Among them:
- Blood analysis. This procedure is carried out in the morning, blood is taken from a finger prick to differentiate the white blood cell count and erythrocyte sedimentation rate (ESR).
- Analysis of urine. Urine collection must be carried out in the morning in a glass or plastic container, having previously carried out hygienic procedures for the external genitalia. To detect chronic pancreatitis, urine samples should be taken over a period of several days to a week.
- Bacteriological research. Pancreatitis is indicated by bacteria containing alpha-amylase, lipase, trypsin, bilirubin and other contents. In addition, an increase in glucose also indicates the development of this disease.
- Analysis of duodenal contents. It is determined by studying the duodenum on an empty stomach. This occurs by inserting a probe into the intestinal cavity: after some time, the contents are collected. It is necessary to make 6 fences in 10 minutes. Based on the results of the procedure, a diagnostic analysis is carried out, duodenal juice is studied, and an accurate diagnosis of the disease is made.
- Coprogram. An effective procedure for detecting chronic pancreatitis. If the disease is present, then the following indicators indicate it:
- ointment-like consistency;
- undigested fiber;
- high nitrogen content;
- steatorrhea;
- increased starch content.
Feces must be collected in a clean container in the morning. Before going through the coprogram itself, you should stop eating meat and vegetables for 3 days.
Instrumental diagnostics
Methods for diagnosing pancreatitis are quite diverse. In addition to examining biological fluids, the doctor needs to see exactly how the pancreas has changed. It is also necessary to establish whether its inflammation has affected surrounding organs and tissues.
Ultrasound diagnostics is considered the most accurate and effective. It allows you to visualize the gland, see whether there are inflammatory processes, whether the tissues of this organ have become smaller. Diagnosis of chronic pancreatitis can also be done using ultrasound. This disease can be detected even in the asymptomatic period. Ultrasound also allows you to examine the bile ducts, determine the beginning of purulent abscesses and see the fluid.
Laparoscopy allows you to simultaneously diagnose and treat pancreatitis. In some cases, during this mini-operation it is possible to minimize the negative impact of inflammation on other organs. But laparoscopy is used only in extremely severe cases.
Diagnosis can also be made using a CT scan. Pancreatitis can be diagnosed by characteristic signs: increased size of the pancreas, the presence of inflammatory processes and dead tissue.
Endoscopy allows you to see all changes in both the pancreas and duodenum. To do this, an endoscope with a camera installed on it is inserted into the esophagus.
Differential diagnosis of pancreatitis allows us to confirm the development of this particular disease and exclude the presence of other ailments of the digestive system with similar signs and conditions. To obtain more extensive information about the disease present in pancreatology, laboratory and instrumental diagnostic methods are used.
Patients with parenchymal pancreas would like to know what clinical condition requires differential diagnosis, as well as its features and with which diseases a comparative analysis is performed.
Diagnostics
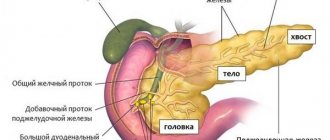
Diagnosis is based on history and confirmed by imaging studies and laboratory tests assessing the structure and function of the pancreas (Figs. 2, 3) [9].
Serum amylase and lipase may be normal or slightly elevated. In 5-10% of patients with chronic pancreatitis, compression of the distal common bile duct leads to increases in serum bilirubin and alkaline phosphatase. Malabsorption of fat leads to increased excretion in feces (more than 7 grams per day). Detection of pancreatic calcifications by radiography, ultrasound or computed tomography is a diagnostic criterion for chronic pancreatitis. These calcifications are found in approximately 25-60% of all cases of chronic alcoholic pancreatitis and in 35-80% of patients with pancreatitis of other etiologies. Computed tomography may also reveal local enlargement of the pancreas, pancreatic atrophy, dilatation of the pancreatic duct, or pseudocyst. RCPG is the most sensitive and specific imaging test in the diagnosis of chronic pancreatitis (Fig. 3).
Due to the risk of developing pancreatitis as a result of ERCP, this diagnostic procedure should be used only when non-invasive studies are of little information. New, more modern types of examinations, such as nuclear resonance cholangiopancreatography and endoscopic ultrasound, are becoming increasingly popular. If all these imaging studies fail to confirm the diagnosis, then pancreatic function testing with secretin stimulation or CC may be performed [10]. The diagnostic algorithm is shown in Figure 4.
Why is a differential analysis of pancreatitis needed?
The use of differential diagnosis of pancreatic disease allows us to finally determine the initial diagnosis of acute or chronic pancreatitis, because the symptoms of this disease are in many ways similar to the signs of other severe pathologies of the gastrointestinal tract.
Differentiation allows you to select the most effective treatment regimen for pathological abnormalities in the pancreas, which will help prevent the development of serious complications:
- Necrosis of parenchymal tissues.
- Complete loss of pancreatic function.
- Death.
Pancreatic disease is considered a rather severe pathology, therefore, if its presence is suspected, it is important to promptly differentiate pancreatitis or another disease.
An incorrect diagnosis can be fatal for the patient, so the use of differential diagnosis is considered a necessary measure for gastroenterological disorders.
Under what condition should pancreatitis be verified?
So, what clinical signs indicating possible abnormalities in the pancreas require differentiation?
Acute pancreatitis is characterized by typical symptoms, which belong to a special group of clinical manifestations under the general name “acute abdomen”. If acute inflammation of the pancreas is suspected, a comparison is made with other diseases of the body’s organs, which also occur in an acute form and have similar symptoms. These include a number of diseases:
- Myocardial infarction.
- Cholecystitis.
- Perforated ulcer.
- Intestinal obstruction.
- Appendicitis.
- Thrombosis of mesenteric vessels.
- Food intoxication.
- Lower lobe pleuropneumonia.
- Ulcer of the stomach and duodenum.
- Abdominal aortic aneurysm.
Differential diagnosis of chronic pancreatitis is carried out according to the following chronic diseases:
- Intestinal tuberculosis.
- Chronic colitis.
- Cholelithiasis.
- Neoplasm in the pancreas.
- Solarite.
- Pancreatitis is a painless type.
- Ulcer of the stomach and duodenum.
- Ischemic abdominal syndrome.
The results of other diagnostic techniques, including laboratory and instrumental ones, are necessarily added to the differential analysis.
Features of differential analysis in acute pancreatitis
Differential diagnosis of acute pancreatitis is carried out by studying the symptoms that appear and comparing them with the manifestations of certain diseases of the organs of some body systems.
The main differences between the symptoms of some common acute diseases and acute pancreatitis are shown in the table.
Acute pathologies
Perhaps the lion's share of patient complaints are complaints of severe pain in the upper abdomen, radiating to the back. Practice shows that such symptoms, coupled with an increased amount of alpha-amylase, become the basis for a diagnosis of pancreatitis.
Blood and urine tests that determine the amount of diastase help to choose the right diagnostic methods if the doctor suggests that acute pancreatitis is present. It is impossible to make an unambiguous diagnosis, relying solely on the stated indicator, since changes in the amount of the enzyme have a different nature: alpha-amylase can change after taking tetracycline drugs, with alcohol poisoning, with other diseases of the abdominal cavity, for example, cholecystitis, peritonitis. Differential diagnosis of chronic pancreatitis facilitates the task of correct diagnosis.
The diagnosis of pancreatitis is established after obtaining a complete clinical picture of the disease and collecting laboratory data. The differential diagnosis of chronic pancreatitis is made by excluding diseases similar to the disease, alcohol and drug intoxication.
Acute pancreatitis. Differential diagnosis
Differential diagnosis is carried out in two stages. At the first stage, acute pancreatitis must be differentiated from other diseases of the abdominal organs that require urgent surgical intervention:
perforation of a gastric or duodenal ulcer, acute intestinal obstruction, destructive cholecystitis, acute occlusion of arteries or veins of the mesenteric basin, as well as myocardial infarction.
For perforation of gastric or duodenal ulcers
In contrast to pancreatic necrosis, the sudden appearance of “dagger” pain is characteristic. At the same time, patients try to lie still, and with pancreatitis they become restless. Unlike pancreatitis, in which repeated vomiting is noted, vomiting is not typical for perforation. Diagnostic doubts can be resolved when free gas is detected under the dome of the diaphragm using plain radiography of the abdominal cavity. Acute pancreatitis is difficult to differentiate from a perforated ulcer of the posterior wall of the stomach, when its contents enter the omental bursa, or in cases of perforation of ulcers of the lesser curvature into the thickness of the lesser omentum. It should be noted that the determination of amylase in the blood or urine is not significant in case of a perforated ulcer, when amylase in excess amounts with the contents of the duodenum enters the abdominal cavity and then enters the blood. A definitive diagnosis can be made by ultrasound and laparoscopy.
The clinical picture of acute pancreatitis can be simulated by the penetration of a stomach or duodenal ulcer
. In these cases, you should always attach importance to the symptoms of exacerbation of peptic ulcer disease. However, with an increase in amylase activity in the blood or urine and symptoms of acute pancreatitis, it is practically impossible to exclude it.
Acute intestinal obstruction
, like pancreatic necrosis, is characterized by an acute onset, intense pain, and repeated vomiting. With destructive pancreatitis and involvement of the mesentery of the small and transverse colon in the necrotic process, clinical symptoms are similar to those with the development of mechanical intestinal obstruction. However, unlike pancreatitis, with mechanical intestinal obstruction, the pain is cramping in nature, accompanied by ringing and resonating intestinal peristalsis (pancreatitis is accompanied by extinction of peristalsis). However, with intestinal obstruction, amylasuria occurs, so this laboratory test is not decisive. Diagnosis is possible by performing a plain radiography of the abdominal organs (multiple levels of fluid in the intestines with obstruction). Acute pancreatitis is characterized by pneumatization of the colon and the absence of Kloiber cups.
The most difficult point in the differential diagnosis of acute pancreatitis (interstitial, limited “capitate” pancreatic necrosis) with acute appendicitis
— the initial stages of the disease, when the symptoms are not yet sufficiently expressed or the appendix is located posteriorly (in the lumbar region or near the gallbladder). The key points of differential diagnosis in these situations are laboratory diagnostics, ultrasound and laparoscopy.
Acute destructive cholecystitis
causes serious problems in differential diagnosis with acute pancreatitis with the development of symptoms of widespread peritonitis. In this situation, acute destructive cholecystitis is supported by the predominant localization of pain in the right hypochondrium with irradiation to the right scapula and shoulder, a painful and enlarged gallbladder on palpation, and the absence of indications of the girdle nature of the pain. It must be remembered that pancreatic necrosis may be accompanied by the development of acute enzymatic cholecystitis. Diagnostic problems are resolved by studying enzyme activity, ultrasound and laparoscopy.
When a stone is strangulated in the distal common bile duct
clinical manifestations correspond to the picture of acute cholecystopancreatitis (“cry of papilla”): the patient rushes about and groans in pain, cannot find a place for himself, pain occurs suddenly in the upper abdomen, is strong, has a girdling nature, is accompanied by repeated vomiting, chills, jaundice, cholangitis and dynamic intestinal obstruction. At the same time, muscle tension and the Shchetkin-Blumberg symptom in the upper abdomen are determined. The optimal algorithm for differential diagnosis: determination of the concentration of bilirubin and its fractions in the blood, the activity of amylase, lipase, alkaline phosphatase, alanine and aspartic aminotransferases, ultrasound, emergency endoscopic retrograde cholangiography, papillotomy with stone extraction.
Acute occlusion
(thrombosis, embolism)
of mesenteric vessels
, in contrast to acute pancreatitis, occurs more often in elderly patients suffering from cardiovascular diseases and atrial fibrillation. In this case, abdominal pain increases quickly, as with perforation of a gastric or duodenal ulcer. Pain and tension in the muscles of the anterior abdominal wall may be diffuse. Leukocytosis is characteristic (20-30x10 9 /l). Sometimes there is blood in the stool. Amylasuria and increased LDH activity have little differential diagnostic value, since the activity of these enzymes increases with intestinal necrosis. Diagnostic doubts are resolved by laparoscopic or angiographic examination.
Ruptured abdominal aortic aneurysm
in contrast to acute pancreatitis, it is characterized by an acute onset, accompanied by symptoms of intra-abdominal or retroperitoneal bleeding and hemorrhagic shock, loss of consciousness, dizziness, persistent hypotension, and acute anemia. A large pulsating formation is palpated in the abdominal cavity, over which a systolic murmur is heard. The same noises are heard on the femoral arteries. Diagnostic doubts are resolved by performing ultrasound of the aorta and abdominal organs, laparoscopy, and aortography.
Differential diagnosis with myocardial infarction
and acute pancreatitis (pancreatic necrosis) should be carried out on the basis of ECG analysis, studies of biochemical markers of acute myocardial damage (creatinine phosphokinase, troponin test), amylase activity in the blood and urine, lipase. It should be remembered that in severe forms of pancreatic necrosis, changes in the ECG may be observed (T segment depression in leads II and III, biphasic T waves in leads I and III), which reflect functional changes in the heart muscle. If diagnostic doubts are not resolved, it is advisable to resort to ultrasound and laparoscopy.
Pancreatitis or perforated ulcer?
Perforated ulcer is a common diagnosis. The symptoms of the disease are thoroughly known to every doctor: pain occurs sharply, the patient experiences a state of shock, the pulse slows down, the abdominal walls are tense, hepatic dullness disappears, being replaced by a tympanic sound symptom of perforation. Add here the picture of an “acute abdomen” - the diagnosis is clear.
It turns out to be difficult to distinguish acute pancreatitis from a perforated ulcer, as evidenced by numerous outpatient and clinical errors. In both cases, the body goes into a state of shock and peripheral circulation is observed.
The first thing that pays attention to is the position of the patient: with a perforated ulcer, the pain intensifies when the patient tries to change position. With pancreatitis, patients change position quite often. The second, often overlooked, is vomiting. With a perforated ulcer, patients practically do not experience the urge to vomit; with pancreatitis, vomiting is a common occurrence. And finally, alpha-amylase: its indicators in perforated ulcers are close to normal, in contrast to patients with pancreatitis.
Pancreatitis or intestinal obstruction
The differential diagnosis of acute pancreatitis excludes the presence of obstruction. In the later stages of intestinal obstruction, the difference in symptoms disappears. At first, it is problematic to correctly determine the form of obstruction: mechanical or dynamic? Considering that dynamic obstruction is becoming a frequent accompaniment of pancreatitis, the task of choosing the correct diagnosis becomes much more complicated.
It is necessary to determine in which intestine the ailment is localized, its type, time and nature. If the doctor is faced with paralytic obstruction, guesses about the development of pancreatitis are confirmed. Attention is drawn to neurogenic mechanisms, since the pathological process, in most cases, exhibits reflex development.
The next step is to assess pain, repeat gagging and flatulence. As the pain increases and spreads throughout the abdomen, vomiting is repeated, increased gas formation occurs - the doctor is inclined towards pancreatitis. With mechanical obstruction, the intestines are practically paralyzed, gas formation is almost absent.
In addition to the general clinical picture, attention is drawn to the indicators of x-ray and laboratory tests: if there is still suspicion of obstruction, it is necessary:
- perform a fluoroscopy of the abdominal organs;
- find out the numbers of blood and urine tests showing the level of alpha-amylase;
- determine blood and urine test data showing chloride levels.
If the amount of chlorides is below normal, one is inclined to favor obstruction; if the level of alpha-amylase is increased and the level of chlorides is normal, one is inclined to favor pancreatitis.
Differential diagnosis of chronic pancreatitis
Perhaps the lion's share of patient complaints are complaints of severe pain in the upper abdomen, radiating to the back. Practice shows that such symptoms, coupled with an increased amount of alpha-amylase, become the basis for a diagnosis of pancreatitis.
Blood and urine tests that determine the amount of diastase help to choose the right diagnostic methods if the doctor suggests that acute pancreatitis is present.
It is impossible to make an unambiguous diagnosis, relying solely on the stated indicator, since changes in the amount of the enzyme have a different nature: alpha-amylase can change after taking tetracycline drugs, with alcohol poisoning, with other diseases of the abdominal cavity, for example, cholecystitis, peritonitis. Differential diagnosis of chronic pancreatitis facilitates the task of correct diagnosis.
The diagnosis of pancreatitis is established after obtaining a complete clinical picture of the disease and collecting laboratory data. The differential diagnosis of chronic pancreatitis is made by excluding diseases similar to the disease, alcohol and drug intoxication.
Pancreatitis or perforated ulcer?
Perforated ulcer is a common diagnosis. The symptoms of the disease are thoroughly known to every doctor: pain occurs sharply, the patient experiences a state of shock, the pulse slows down, the abdominal walls are tense, hepatic dullness disappears, being replaced by a tympanic sound symptom of perforation. Add here the picture of an “acute abdomen” - the diagnosis is clear.
It turns out to be difficult to distinguish acute pancreatitis from a perforated ulcer, as evidenced by numerous outpatient and clinical errors. In both cases, the body goes into a state of shock and peripheral circulation is observed.
The first thing that attention is paid to is the position of the patient: with a perforated ulcer, the pain intensifies when the patient tries to change position. With pancreatitis, patients change position quite often.
The second, often overlooked, is vomiting. With a perforated ulcer, patients practically do not experience the urge to vomit; with pancreatitis, vomiting is a common occurrence.
And finally, alpha-amylase: its indicators in perforated ulcers are close to normal, in contrast to patients with pancreatitis.
Pancreatitis or intestinal obstruction
The differential diagnosis of acute pancreatitis excludes the presence of obstruction. In the later stages of intestinal obstruction, the difference in symptoms disappears. At first, it is problematic to correctly determine the form of obstruction: mechanical or dynamic? Considering that dynamic obstruction is becoming a frequent accompaniment of pancreatitis, the task of choosing the correct diagnosis becomes much more complicated.
It is necessary to determine in which intestine the ailment is localized, its type, time and nature. If the doctor is faced with paralytic obstruction, guesses about the development of pancreatitis are confirmed. Attention is drawn to neurogenic mechanisms, since the pathological process, in most cases, exhibits reflex development.
The next step is to assess pain, repeat gagging and flatulence. As the pain increases and spreads throughout the abdomen, vomiting is repeated, increased gas formation occurs - the doctor is inclined towards pancreatitis. With mechanical obstruction, the intestines are practically paralyzed, gas formation is almost absent.
In addition to the general clinical picture, attention is drawn to the indicators of x-ray and laboratory tests: if there is still suspicion of obstruction, it is necessary:
- perform a fluoroscopy of the abdominal organs;
- find out the numbers of blood and urine tests showing the level of alpha-amylase;
- determine blood and urine test data showing chloride levels.
If the amount of chlorides is below normal, one is inclined to favor obstruction; if the level of alpha-amylase is increased and the level of chlorides is normal, one is inclined to favor pancreatitis.
Pancreatitis or intestinal tuberculosis?
Intestinal tuberculosis is a bacterial disease, the culprits being microbacteria tuberculosis.
As a rule, at the onset of the disease, patients do not experience much discomfort and do not notice warning symptoms.
In rare cases, nausea, heaviness in the stomach after eating, general malaise and stool disorders appear. As a rule, the manifestations are not very disturbing, and the disease goes undetected for a long time.
Differentiation of intestinal tuberculosis
Considering the initial development of the disease in the lungs, people suffering from other types of tuberculosis should be excluded from the group of patients with pancreatitis. More confidence in making a diagnosis will be given by laboratory test numbers: in the case of tuberculosis, hypochromic anemia is observed with normal diastase values.
Pancreatitis or gallstone disease
Inflammation of the pancreas is easily confused with cholelithiasis, which is not surprising, given the close proximity of the gallbladder. Hence, it is important to differentiate the correct disease. The disease often mentioned becomes the ancestor of pancreatitis.
Gallstone disease is accompanied by similar symptoms: a tense abdomen, sore skin. Ultrasound diagnostics of the gallbladder will help shed light on the truth - the method remains the most informative and accessible, it allows you to determine the presence of stones, see how deformed the walls of the gallbladder are and how motility is changed.
You can use MRI and CT diagnostic indicators, conduct scintigraphy of the biliary system and identify data from a general and biochemical blood test showing an increase in erythrocyte sedimentation rate and an increase in alkaline phosphatase activity.
Pancreatitis or oncology?
Differential diagnosis of acute pancreatitis involves excluding the possibility of oncology. Pancreatic cancer is often indistinguishable from inflammation of the pancreas.
Cancer does not appear in any way until the fourth stage. Similar to previous cases, patient complaints begin with pain in the abdominal area of varying intensity: from slight discomfort to acute attacks.
Pay attention to the color of the skin, which acquires a yellowish tint. The stool becomes discolored, the urine darkens, the skin itches appears - this is what cancer looks like most often.
The condition of patients deteriorates sharply due to rapid metastasis.
The main symptom is rapid weight loss. Weight loss occurs due to decreased appetite and severe intoxication caused by tumor growth. To exclude cancer, it is necessary to include a number of studies in the diagnostic complex:
- blood analysis;
- CT;
- radiograph;
- ultrasonography;
- MRI;
- biopsy;
- PET-CT.
Pancreatitis or thrombosis of mesenteric vessels?
A frequent “double” of pancreatitis is thrombosis of mesenteric vessels. In both cases, severe pain is observed, leading the patient to the walls of the hospital. It is necessary to pay attention to details: with thrombosis, patients rarely complain of vomiting; upon palpation, tension and pain in the epigastric region are not felt, but bloody stools are not uncommon.
Certain parts of the intestine sometimes stop performing functions, but peristalsis periodically remains visible. Laboratory tests may not clarify the picture: in cases of intestinal infarction, alpha-amylase levels are also sometimes elevated.
Source: https://GastroTract.ru/bolezn/pankreatit/differentsialnaya-diagnostika-hronicheskogo-pankreatita.html
Pancreatitis or intestinal tuberculosis?
Intestinal tuberculosis is a bacterial disease, the culprits being microbacteria tuberculosis. As a rule, at the onset of the disease, patients do not experience much discomfort and do not notice warning symptoms. In rare cases, nausea, heaviness in the stomach after eating, general malaise and stool disorders appear. As a rule, the manifestations are not very disturbing, and the disease goes undetected for a long time.
Differentiation of intestinal tuberculosis
Considering the initial development of the disease in the lungs, people suffering from other types of tuberculosis should be excluded from the group of patients with pancreatitis. More confidence in making a diagnosis will be given by laboratory test numbers: in the case of tuberculosis, hypochromic anemia is observed with normal diastase values.
Pancreatitis or gallstone disease
Inflammation of the pancreas is easily confused with cholelithiasis, which is not surprising, given the close proximity of the gallbladder. Hence, it is important to differentiate the correct disease. The disease often mentioned becomes the ancestor of pancreatitis.
Gallstone disease is accompanied by similar symptoms: a tense abdomen, sore skin. Ultrasound diagnostics of the gallbladder will help shed light on the truth - the method remains the most informative and accessible, it allows you to determine the presence of stones, see how deformed the walls of the gallbladder are and how motility is changed.
You can use MRI and CT diagnostic indicators, conduct scintigraphy of the biliary system and identify data from a general and biochemical blood test showing an increase in erythrocyte sedimentation rate and an increase in alkaline phosphatase activity.
Diagnosis of pancreatitis
Correct diagnosis will help to quickly identify the disease and prescribe adequate treatment methods.
Diagnosing chronic pancreatitis is not easy, especially in the early stages. In this regard, the gastroenterologist is helped in diagnosing pancreatitis by laboratory tests and instrumental research methods.
Diagnostic signs of the acute course of the disease:
- Voskresensky's symptom, in which the doctor cannot feel the pulsation of the aorta.
- The most common symptom is called Gray-Thurner; bluish spots form on the patient’s abdominal wall, and Cullen’s symptom, cyanosis in the navel area, is also noted.
- Mayo-Robson symptom, when the ribs are palpated on the left side, the patient experiences acute pain.
Also read on our website: Biliary pancreatitis: causes, clinical picture, diagnosis
Diagnostic signs:
- Thrombosis of the splenic vein.
- Impaired digestive function.
- Anemic syndrome.
- Bile stagnation syndrome, which occurs with pronounced signs of jaundice.
General laboratory diagnostics:
- A biochemical blood test is prescribed.
- The water and electrolyte balance in the patient's blood is assessed.
- It is mandatory to take a general blood and urine test.
Instrumental diagnostic methods:
- Ultrasound examination of the pancreas.
Ultrasound diagnostics is a modern, highly informative method for studying various structures of the human body. - X-ray examination, which helps to identify stones in the pancreas or ducts.
- Computed tomography is often prescribed; it helps to identify necrotic areas.
Computed tomography is an important stage in complex diagnostics, which allows you to assess the condition and identify pathological changes in internal organs - If necessary, laparoscopy and endoscopy are performed.
Differential diagnosis is necessary to exclude acute surgical pathologies directly in the abdominal cavity. For example: perforated ulcer, acute cholecystitis, intestinal obstruction, as well as intestinal vein thrombosis.
Now you know that the classification of pancreatitis is extensive. But it is she who helps doctors determine all the nuances of this disease. In order to identify the disease at the initial stage of its development, at the first symptoms you must immediately consult a doctor and undergo a diagnostic examination.
Pancreatitis or oncology?
Differential diagnosis of acute pancreatitis involves excluding the possibility of oncology. Pancreatic cancer is often indistinguishable from inflammation of the pancreas.
Cancer does not appear in any way until the fourth stage. Similar to previous cases, patient complaints begin with pain in the abdominal area of varying intensity: from slight discomfort to acute attacks. Pay attention to the color of the skin, which acquires a yellowish tint. Stool becomes discolored, urine darkens, skin itches appears—this is what cancer looks like most often. The condition of patients deteriorates sharply due to rapid metastasis.
The main symptom is rapid weight loss. Weight loss occurs due to decreased appetite and severe intoxication caused by tumor growth. To exclude cancer, it is necessary to include a number of studies in the diagnostic complex:
- blood analysis;
- CT;
- radiograph;
- ultrasonography;
- MRI;
- biopsy;
- PET-CT.
Clinical manifestations
Abdominal pain and weight loss are the two most common clinical manifestations of chronic pancreatitis. Pain reduces patients' appetite and leads to food restriction, leading to weight loss and malnutrition. Abdominal pain is the most common indication for surgery for chronic pancreatitis. Typically the pain is characterized as diffuse and localized in the upper abdomen. Abdominal pain increases after eating and is also present at night. The exact mechanisms underlying the onset of pain remain a matter of debate, but it may be due to inflammation of the pancreas, increased intrapancreatic pressure, neuroinflammation, or extrapancreatic causes such as stenosis of the common bile duct or duodenum. Weight loss initially occurs due to a decrease in the number of calories taken in as a result of fear and anticipation of abdominal pain. Later, as pancreatitis progresses, the patient develops malabsorption as a result of pancreatic insufficiency. Diabetes mellitus develops when 80% of the glands are destroyed [8]. Steatorrhea occurs when 90% of pancreatic function is lost.
Pancreatitis or thrombosis of mesenteric vessels?
A common “double” of pancreatitis is thrombosis of mesenteric vessels. In both cases, severe pain is observed, leading the patient to the walls of the hospital. It is necessary to pay attention to details: with thrombosis, patients rarely complain of vomiting; upon palpation, tension and pain in the epigastric region are not felt, but bloody stools are not uncommon.
Certain parts of the intestine sometimes stop performing functions, but peristalsis periodically remains visible. Laboratory tests may not clarify the picture: in cases of intestinal infarction, alpha-amylase levels are also sometimes elevated.