Short description
Chronic pancreatitis (acute pancreatitis, see Surgical diseases) is a chronic inflammation of the pancreas. It usually occurs in middle and old age, more often in women. There are primary chronic pancreatitis and secondary, or concomitant, developing against the background of other diseases of the digestive tract (chronic gastritis, cholecystitis, enteritis, etc.). Prolonged acute pancreatitis can become chronic, but more often it develops gradually against the background of chronic cholecystitis, cholelithiasis or under the influence of unsystematic irregular nutrition, frequent consumption of spicy and fatty foods, chronic alcoholism, especially in combination with a systematic deficiency of proteins and vitamins in food, penetration ulcers of the stomach or duodenum in the pancreas, atherosclerotic damage to the vessels of the pancreas, infectious diseases (especially with infectious mumps, typhoid and typhus, viral hepatitis), some helminthiasis, chronic intoxication with lead, mercury, phosphorus, arsenic.
Code according to the international classification of diseases ICD-10:
- K86.1 Other chronic pancreatitis
Symptoms
Signs and manifestations are different for different forms of inflammation. In the acute form, patients complain of severe abdominal pain on the left, bloating, nausea and vomiting mixed with bile, and dehydration. Bluish-yellowish spots may appear on the left side or at the navel from burst small vessels and capillaries. The most dangerous complication of acute pancreatitis is intoxication of the body, which can cause cerebral edema, kidney failure and death of the patient.
Chronic disease reduces the ability of the pancreas to produce enzymes and hormones. As a result, the process of digesting food is disrupted. Sometimes in the pancreas, after acute inflammation, pseudocysts form in which fluid or pus accumulates. Over time, chronic inflammatory processes develop and these formations grow and are compressed by other organs, resulting in pain, heaviness after eating, nausea and a bitter taste in the mouth. Another symptom is obstructive jaundice, caused by narrowing and poor patency of the biliary tract.
Pathology has such symptoms not only with alcohol etiology, but also with other types of chronic disease, which are provided for by the tenth classifier of diseases. Digestive disorders, diarrhea, and intolerance to certain foods are also added to them.
Causes
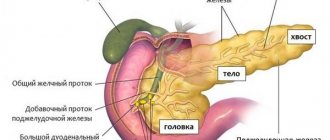
Pathogenesis : delayed release and intraorgan activation of pancreatic enzymes - trypsin and lipase, which carry out autolysis of the pancreatic parenchyma, reactive growth and cicatricial wrinkling of connective tissue, which then leads to sclerosis of the organ, chronic circulatory disorders in the pancreas. In the progression of the inflammatory process, processes of autoaggression are of great importance. In chronic pancreatitis of infectious origin, the pathogen can penetrate the pancreas from the lumen of the duodenum (for example, with dysbacteriosis) or from the bile ducts through the pancreatic ducts in an ascending way, which is facilitated by dyskinesia of the digestive tract, accompanied by duodeno- and choledocho-pancreatic reflux. Predispose to the occurrence of chronic pancreatitis are spasms, inflammatory stenosis or tumor of the papilla of Vater, which prevent the release of pancreatic juice into the duodenum, as well as insufficiency of the sphincter of Oddi, which facilitates the free entry of duodenal contents into the pancreatic duct, especially enterokinase contained in the intestinal juice, which activates trypsin. The inflammatory process can be diffuse or limited only to the head or tail of the pancreas. There are chronic edematous (interstitial), parenchymal, sclerosing and calculous pancreatitis.
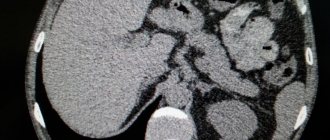
Symptoms, course . Pain in the epigastric region and left hypochondrium, dyspepsia, diarrhea, weight loss, diabetes mellitus. The pain is localized in the epigastric region on the right with a predominant localization of the process in the region of the head of the pancreas, if its body is involved in the inflammatory process - in the epigastric region on the left, if its tail is affected - in the left hypochondrium; Often the pain radiates to the back and has a girdling character; it can radiate to the heart area, simulating angina pectoris. The pain can be constant or paroxysmal and appear some time after eating fatty or spicy foods. There is pain in the epigastric region and left hypochondrium. Often there is a painful point in the left costovertebral angle (Mayo-Robson symptom). Sometimes a zone of skin hyperesthesia is determined corresponding to the zone of innervation of the eighth thoracic segment on the left (Kach’s symptom) and some atrophy of the subcutaneous fatty tissue in the area of the projection of the pancreas onto the anterior wall of the abdomen. Dyspeptic symptoms in chronic pancreatitis are almost constant. Complete loss of appetite and aversion to fatty foods are common. However, with the development of diabetes mellitus, on the contrary, patients may feel severe hunger and thirst. Increased salivation, belching, attacks of nausea, vomiting, flatulence, and rumbling in the stomach are often observed. Stupa in mild cases is normal, in more severe cases there is diarrhea or alternating constipation and diarrhea. Characterized by pancreatic diarrhea with the release of copious, pasty, foul-smelling, greasy feces; scatological examination reveals steatorrhea, creatorrhoea, kitarhinorrhea. In the blood - moderate hypochromic anemia, during an exacerbation - increased ESR, neutrophilic leukocytosis, hypoproteinemia and dysproteinemia due to increased globulin content. With the development of diabetes mellitus, hyperglycemia and glycosuria are detected, and in more severe cases, disturbances in electrolyte metabolism, in particular hyponatremia. The content of trypsin, antitrypsin, amylase and lipase in the blood and amylase in the urine increases during an exacerbation of pancreatitis, as well as when there are obstacles to the outflow of pancreatic juice (inflammatory swelling of the head of the gland and compression of the ducts, cicatricial stenosis of the papilla of Vater, etc.). In the duodenal contents, the concentration of enzymes and the total volume of juice in the initial period of the disease may be increased, but with a pronounced atrophic-sclerotic process in the gland, these indicators decrease, and pancreatic hyposecretion occurs. Duodenoradiography reveals deformations of the internal contour of the duodenal loop and depressions caused by an enlargement of the head of the pancreas. Echography and radioisotope scanning show the size and intensity of the pancreatic shadow; in diagnostically difficult cases, computed tomography is performed. The course of the disease is protracted. According to the characteristics of the course, chronic recurrent pancreatitis, painful, pseudotumor, and latent forms are distinguished (rare).
Patient examination plan
Treatment begins after diagnosis. A sick child (adult) must be interviewed and examined by a doctor. The following studies are being carried out:
- auscultation;
- percussion;
- palpation of the abdomen (superficial and deep);
- Ultrasound;
- blood chemistry;
- study of water-electrolyte status;
- general clinical tests;
- radiography;
- CT scan.
A blood test reveals the following changes:
- increased ESR;
- decrease in hematocrit;
- leukocytosis;
- increased concentrations of glucose, lipase, amylase, C-reactive protein, urea;
- decreased levels of total protein, calcium, sodium and potassium.
Treatment
Treatment . In the initial stages of the disease and in the absence of severe complications - conservative; during the period of exacerbation, it is advisable to carry out treatment in a gastroenterological hospital (during a period of sharp exacerbation, treatment is the same as for acute pancreatitis). The patient's meals should be fractional, 5-6 times a day, but in small portions. Avoid alcohol, marinades, fried, fatty and spicy foods, strong broths that have a significant stimulating effect on the pancreas. The diet should contain an increased amount of proteins (table No. 5) in the form of lean meats, fish, fresh low-fat cottage cheese, and mild cheese. The fat content in the diet is moderately limited (up to 80 - 70 g per day), mainly due to pork and lamb fat. With significant steatorrhea, the fat content in the diet is further reduced (to 50 g). Carbons are limited, especially mono- and disaccharides; with the development of diabetes mellitus, the latter are completely excluded. Food is given warm. For exacerbations, antienzyme agents (trasylol, contrical or pantripin) are prescribed; in less acute cases - metabolic drugs (pentoxyl 0.2 - 0.4 g per dose, methyluracil 1 g 3 - 4 times a day for 3 - 4 weeks), lipotropic drugs - lipocaine, methionine. Antibiotics are indicated for severe exacerbations or abscessation of the pancreas. For severe pain, perinephric or paravertebral novocaine blockade, non-narcotic analgesics, baralgin are indicated, and in especially severe cases, narcotic analgesics in combination with anticholinergic and antispasmodic agents. For exocrine pancreatic insufficiency, enzyme replacement preparations are prescribed: pancreatin (0.5 g 3-4 times a day), abomin, cholenzyme, festal, panzinorm, etc.; multivitamins. After the removal of acute phenomena and in order to prevent exacerbation in the future, resort treatment in Borjomi, Essentuki, Zheleznovodsk, Pyatigorsk, Karlovy Bary and in local gastroenterological sanatoriums is recommended. Patients with chronic pancreatitis are not recommended for types of work in which it is impossible to adhere to a strict diet; in case of severe disease - transfer to disability. Surgical treatment is recommended for severe painful forms of chronic pancreatitis, cicatricial inflammatory stenosis of the common bile and (or) pancreatic duct, abscess formation or the development of a gland cyst.
Prevention . Timely treatment of diseases that play an etiological role in the occurrence of pancreatitis, elimination of the possibility of chronic intoxications that contribute to the development of this disease (industrial, as well as alcoholism), ensuring a balanced diet and daily routine.
The most common cause of chronic pancreatitis (about 60% of cases). Due to the fact that less than 5-10% of patients suffering from alcoholism develop chronic pancreatitis, it has been assumed that there are associated risk factors. Thus, in 5.8% of patients with chronic alcoholic pancreatitis, the N34S mutation was detected; in patients with alcoholism without the development of chronic pancreatitis, this mutation was observed in only 1% of cases.
Cystic fibrosis (cystic fibrosis).
It is an autosomal recessive disease in which there is a mutation in the CFTR gene, which encodes a protein involved in the transport of chlorine across the cell membrane. Mutations in the CFTR gene can lead to severe chronic pancreatitis and respiratory damage. Cystic fibrosis, as an etiological cause, accounts for a small proportion of cases of chronic pancreatitis.
An autosomal dominant disease with a penetrance of 80%. The disease is associated with a mutation in the cationic trypsinogen gene, located on chromosome 7.
Hyperlipidemia (usually types 1 and 5).
It can cause the development of chronic pancreatitis, but usually manifests itself as repeated attacks of acute pancreatitis.
Taking medications.
Pancreatic-damaging agents include azathioprine, chlorothiazide derivatives, estrogens, furosemide, and tetracycline. Less commonly, the same effect is observed when using cimetidine, metronidazole, glucocorticoids, brufen, nitrofuran.
Idiopathic chronic pancreatitis (in approximately 30% of cases).
Idiopathic pancreatitis is divided into early and late onset forms. Some cases of "idiopathic" pancreatitis may have genetic mutations.
- Obstructive causes of chronic pancreatitis (impaired outflow of exocrine pancreatic secretions):
- Congenital anomalies such as divided pancreas and annular divided pancreas. Congenital anomalies are very rare causes of chronic pancreatitis and, as a rule, require the presence of additional provoking factors for the development of chronic pancreatitis (stenosis of the minor duodenal papilla).
- Acquired obstructive forms of chronic pancreatitis occur as a result of blunt trauma to the abdomen, leading to damage to the pancreatic ductal system. Also, a violation of the outflow of pancreatic secretions can develop as a result of inflammatory processes in the 12pc, which leads to fibrosis and papillary stenosis, as well as as a result of a tumor or calculi. Diseases of the gallbladder and biliary tract are the most common cause of the development of obstructive chronic pancreatitis. It occurs as a result of intrapancreatic activation of pancreatic enzymes due to regurgitation of bile and the contents of the 12th intestine into its ducts, which is observed in cholelithiasis, biliary and duodenal hypertension, and pathology of the Fayer's nipple.
- Autoimmune pancreatitis.
Clinics for treatment with the best prices
| Price | Total: 612 in 33 cities |
| Selected clinics | Phones | City (metro) | Rating | Price of services |
| KDS Clinic on Belozerskaya | +7(499) 969..show Appointment +7(499) 969-23-25+7(495) 121-04-83+7(495) 121-04-23 | Moscow (m. Bibirevo) | rating: 4.3 | 11680ք |
| MedCenterService in Basmanny | +7(495) 927..show Appointment +7(495) 927-03-01+7(499) 641-13-02 | Moscow (metro station Chkalovskaya) | rating: 4.4 | 15215ք |
| MedCenterService in Maryino | +7(495) 927..show Appointment +7(495) 927-03-01+7(499) 641-13-02 | Moscow (metro Bratislavskaya) | rating: 4.4 | 15215ք |
| MedCenterService in Solntsevo | +7(495) 927..show Appointment +7(495) 927-03-01+7(495) 431-42-42+7(495) 324-88-22 | Moscow (metro station Rumyantsevo) | rating: 4.4 | 15215ք |
| MedCenterService in Cheryomushki | +7(495) 927..show Appointment +7(495) 927-03-01+7(499) 641-13-02 | Moscow (metro station Novye Cheryomushki) | rating: 4.5 | 15215ք |
| MedCenterService in Mitino | +7(495) 125..show Appointment +7(495) 125-22-36+7(499) 641-13-02 | Moscow (m. Mitino) | rating: 4.4 | 15215ք |
| MedCenterService in Taganskoye | +7(495) 927..show Appointment +7(495) 927-03-01+7(499) 641-13-02 | Moscow (metro station Taganskaya) | rating: 4.4 | 15215ք |
| MedCenterService in Krasnoselsky | +7(495) 927..show Appointment +7(495) 927-03-01+7(499) 641-13-02 | Moscow (metro station Sukharevskaya) | rating: 4.5 | 15215ք |
| MedCenterService in Northern Medvedkovo | +7(495) 927..show Appointment +7(495) 927-03-01+7(499) 641-13-02 | Moscow (metro station Medvedkovo) | rating: 4.4 | 15215ք |
| MedCenterService in Konkovo | +7(495) 927..show Appointment +7(495) 927-03-01+7(499) 641-13-02 | Moscow (metro station Belyaevo) | rating: 4.4 | 15215ք |
Etiology and predisposing factors
The etiological causes of this disease are varied. The most common causes of chronic pancreatitis include the following:
- hereditary predisposition to this pathology;
- excess body weight, accompanied by hyperlipidemia due to metabolic disorders in the body;
- exposure to toxic substances;
- cystic fibrosis is an autosomal recessive pathology that leads to the formation of cystic fibrosis of the pancreas due to a violation of the transmembrane conduction regulator, which disrupts many types of metabolism in cells (sodium, chlorine, H2O, ATP);
- Excessive alcohol consumption also leads to the development of pancreatic disease. In the ICD, pancreatitis of this etiology is allocated to a separate category - “Chronic pancreatitis of alcoholic etiology” (K 86.0);
- long-term use of medications;
- idiopathic CP;
- obstruction of the excretory ducts due to traumatic injury, tumor processes in nearby organs;
- congenital malformations of the pancreas;
- autoimmune form of pancreatitis;
- infectious viral infection;
- primary biliary cirrhosis;
- diseases of the duodenum;
- sclerosing cholangitis, cholelithiasis.
Predisposing factors for the development of chronic pancreatitis may be a violation of the diet (an abundance of fatty, fried, sweet foods), smoking, prolonged nervous tension, and severe stress.
Therapeutic tactics for pancreatitis
Every experienced doctor knows whether it is possible to die with acute inflammation of the pancreas. In order to reduce the risk of complications, patients should be treated as early as possible. If you suspect acute pancreatitis, you should do the following:
- provide the patient with peace;
- it is convenient to seat a person;
- exclude food intake;
- organize plenty of drinking;
- call a doctor or ambulance.
Enzyme preparations are contraindicated during an attack. It is not recommended to take painkillers. It is impossible to determine how long the attack will last. To alleviate the patient's condition, you need to give him a half-sitting position with his knees pressed. Medical assistance consists of the use of antispasmodics, novocaine blockade, and the use of enzyme inhibitors (Gordox, Trasylol, Aprotex).
Infusion therapy must be organized. It allows you to replenish fluid deficiency and restore electrolyte balance. Antibiotics are used to prevent purulent complications. All medications must be administered by injection. If an abscess or cyst forms, and if gallstone disease is detected, surgery is required.
Acute pancreatitis must be recorded in the surgical medical history. This is necessary so that in the future the doctor will have an idea about the inflammation of the pancreas suffered by the patient. After the course of treatment, you must follow a diet and give up alcohol. The doctor should tell the patient how long to adhere to proper nutrition.
Symptoms of the disease and features of the clinical course
Symptomatic manifestations will depend on the stage of the disease - the period of exacerbation or remission. If the patient is in remission, then the disease may proceed without any pronounced symptoms ; periodic discomfort in the epigastric region or in the left hypochondrium is possible.
The disease has significantly more symptomatic manifestations during the period of exacerbation. There are a number of main symptoms that can have varying degrees of severity depending on the severity of the pathology.
It should be noted that in addition to the fact that chronic pancreatitis in ICD 10 has a certain coding, in practice data from clinical classifications are also used to describe the diagnosis, for example, classification of the disease by severity:
- Mild form: periods of exacerbations are infrequent, from one to two times a year, the symptoms are not severe and are easily eliminated.
- Moderate form of severity - exacerbation of the disease occurs up to four times a year, and lasts quite a long time, with severe pain, a slight decrease in body weight and changes in laboratory parameters.
- Severe form – exacerbations are frequent, more than 5-6 times a year, pain is pronounced, body weight drops sharply, complications develop.
The main symptoms of chronic pancreatitis are:
- Painful sensations of varying intensity and duration. They arise mainly due to a violation of the diet and the intake of prohibited foods (spicy or fatty foods, carbonated drinks, confectionery in large quantities). Discomfort appears in the epigastric region, but irradiation is possible to the right or left hypochondrium, epigastric region, left shoulder, chest (depending on which part of the pancreas is affected).
- Decreased appetite or its complete absence.
- Nausea throughout the day.
- Vomiting that does not bring relief.
- Belching, feeling of bitterness in the mouth.
- The tongue is covered with a white coating.
- Excessive gas formation in the intestines, pronounced rumbling.
- Prolonged severe diarrhea, as a result of which a person quickly loses weight, the stool is liquid, oily, and may consist of undigested pieces of food.
- Increased body temperature.
Classification of the disease - pancreatitis
Reactive pancreatitis in children
A classification of chronic pancreatitis has been developed for accurate diagnosis, identification of the causes of the disease and more effective selection of medications.
Reactive
The mildest form of the disease is reactive pancreatitis.
It occurs with regular overeating, if the patient abuses fatty foods or often drinks alcoholic beverages.
Often the disease is provoked by problems with the gastrointestinal tract. The following symptoms are characteristic of reactive pancreatitis:
- sharp pain on the left side in the ribs;
- nausea;
- bouts of hiccups;
- stomach cramps;
- chills;
- during attacks, sticky sweat;
- bloating;
- dry mouth;
- white coating on the tongue;
- hyperthermia;
- flatulence;
- the appearance of shortness of breath.
Alcoholic
At the initial stage of the disease, alcoholic pancreatitis has virtually no symptoms. Therefore, patients often seek medical help when serious complications of the disease begin. Plugs appear in the pancreas, which provoke the development of edema and inflammatory processes. Protein plugs cause stagnation of fluid, which precipitates in the form of calcium salts. Over time they turn into stones.
As the stones grow, they disrupt the outflow of enzymes, causing inflammation in the gland. Fibrous tissue grows, which causes severe pain and interferes with the proper functioning of the organ. This causes stomach and duodenal ulcers, colitis, inflammatory processes in the bile ducts, and the appearance of diabetes mellitus.
Pseudotumorous
Pseudotumorous, or precancerous pancreatitis is associated with uneven hypertrophy of the pancreas. A malignant tumor appears, which can only be removed surgically.
The following symptoms are typical for this type of disease:
- severe weight loss and exhaustion;
- jaundice;
- decreased echogenicity of the organ;
- disturbances in the gastrointestinal tract;
- problems with the endocrine system;
- severe pain, which is characteristic of chronic pancreatitis.
Trypsin, phospholipase and other enzymes are activated in the gland, which begin to corrode the tissue, leading to the death of the organ cell and causing the appearance of necrosis. Iron, in order to avoid decay, reduces the production of enzymes, protecting the dead areas with connective tissue. Cysts appear and actively grow as the disease worsens. The gland becomes inflamed and swells. After 10-15 years, a large number of compactions are observed in the organ, which increase the pancreas in size.
The pseudotumorous form is characterized by the following symptoms:
- there is an exacerbation in the form of intense pain;
- the appearance of obstructive jaundice;
- vomiting and nausea;
- upon palpation, an enlargement of the gland is observed;
- the shape of the organ is heterogeneous;
- the patient quickly loses weight;
- Undigested fiber and muscle fibers are observed in the stool.
Pancreaopathy
Ancreopathy develops due to insufficient production of enzymes in the pancreas. The disease is most often observed in children. In adults, it can be triggered by excess or unusual nutrition. In older people, the disease is vascular in nature. Pancreopathy is manifested by the following symptoms:
- pain in the left hypochondrium;
- pain in the navel area;
- frequent diarrhea;
- decreased appetite.
When performing an ultrasound, changes are most often not detected. In blood and urine tests, enzyme levels are reduced. Undigested fat is observed in the stool.
Dispancreatism
The disease is characterized by the following symptoms:
- decreased appetite or complete absence of it;
- nausea even at the sight of food;
- vomiting after eating;
- aching or nagging pain in the upper abdomen;
- loose stools with a foul odor and undigested fatty components.
The disease is treated in the same way as chronic pancreatitis.
Diagnostic measures and treatment principles
Pancreatitis in ICD 10, depending on the form of the disease, is divided into acute and chronic, but the diagnosis of the pathology is almost the same.
To make a correct diagnosis and prescribe rational treatment, it is necessary to collect an anamnesis, thanks to which you can determine the etiology, as well as conduct the necessary laboratory and instrumental studies :
- clinical blood test;
- clinical urine analysis;
- blood chemistry;
- clinical examination of stool;
- ultrasound examination of the abdominal organs;
- radiography of the abdominal organs;
- cholangiopancreatography (endoscopic retrograde);
- glucose load tests;
- gastroscopy.
To determine the phase of pancreatitis, it is also necessary to conduct a study of pancreatic enzymes, lipids, calcium in the blood plasma; pancreatic function tests; study of antibody titers to viruses; computed tomography.
The main point of treatment for chronic pancreatitis is a strict diet, which is prescribed by a doctor and excludes the consumption of fatty, spicy, sour foods , foods containing preservatives, as well as carbonated drinks and alcohol. In case of exacerbation, symptomatic therapy is prescribed - analgesics, antihistamines, antispasmodics, proton pump inhibitors, enzyme medications, antacids.
Save the link, or share useful information on social media. networks
Types of acute forms of pancreatitis
The disease can be primary or secondary. In the latter case, the inflammatory process is caused by pathology of other digestive organs (liver, gall bladder). Every second acute pancreatitis is associated with cholecystitis. There are edematous (catarrhal) and necrotic forms of the disease. The difference is that in the first case there is no mass death of gland cells.
Pancreatic necrosis can be sterile or infected. There are also mild and severe degrees of the disease. In the first case, the prognosis is more favorable, since other organs and systems are practically not involved in the process. In severe cases, complications develop. Sterile pancreatic necrosis can be focal or widespread. There are fatty, mixed and hemorrhagic forms of this pathology. There are also drug-induced pancreatitis.
Diagnosis of pancreatitis code according to ICD 10
Healthcare, for the purpose of systematization and management, has developed a classification of diseases (ICD), which is revised once every 10 years. This is a normative document that provides a unified approach to the classification of diseases and serves as a mandatory classifier when making a diagnosis.
There are more than 40 classifiers of pancreatitis, which significantly complicates the communication between doctors when voicing a patient’s diagnosis. So that experts from different countries could easily share skills and understand each other, the International Systematization of Diseases (ICD) was established. Currently, the 10th revision system (ICD-10) is in effect, which is used to diagnose the disease.
According to the international classification, pancreatitis according to ICD 10 is divided into:
- K85 Acute pancreatitis.
- K86.0 Chronic pancreatitis of alcoholic etiology.
- K86.1 Other chronic pancreatitis.
There are 3 key types of chronic pancreatitis ICD code 10:
- Chronic calcific inflammation, often caused by alcoholism. With this inflammatory process, changes in the structure of the ducts of the organ and thickening of secretion are observed, which leads to blockage of the ducts.
- Chronic obstructive inflammation. It is characterized by a narrowing of the main ducts of the gland or its large branches.
- Acute inflammation of pancreatitis is not common and is an exacerbation of chronic pancreatitis.
In some cases, biliary or biliary-dependent pancreatitis is observed, which develops against the background of existing diseases - pathologies of the liver, gallbladder or biliary tract.
Patients often consult a doctor if they have the following symptoms and signs:
- presence of pain;
- for nausea;
- vomiting;
- with rapid loss of body weight;
- with unstable stools;
- manifestation of bad breath.
The doctor conducts and prescribes a number of tests if he suspects a person has pancreatic disease:
- Initial examination of the patient. The course of the disease in this type of disease, as a rule, is not pronounced. Moderate bloating is observed. Small protruding red formations are visible on the skin of the abdomen. By palpation, the organ can be felt in severely malnourished patients. With cystic disease of the pancreas, the organ is easily palpable due to pathological changes that lead to its enlargement. In severe forms of this disease, slight abdominal tension is often observed.
- In the acute course of the disease, an increase in phospholipase A 2 is observed.
- The doctor prescribes laboratory tests to make a diagnosis, one of which is a general analysis of blood, stool and urine. In severe cases of the disease, an increase in the number of leukocytes and ESR is observed. In other forms of the disease, blood counts remain normal.
- A person is given glucose to drink, and if after a couple of hours its level exceeds 8 mmol/l, then this indicates the presence of diabetes mellitus, which is often a concomitant pathology of this disease.
- Study of enzymes. In acute exacerbation of chronic pancreatitis according to ICD 10, an increase in amylase is observed. The study of this enzyme is rather non-specific. That is why another enzyme test, elastase, is being studied at the same time.
- Conduct a study of lipase activity.
- Study of blood elastase. This indicator increases with acute exacerbation.
- Study of blood trypsin. A reduced rate indicates insufficiency of the exocrine function of the gland, which manifests itself in the chronic form of the disease.
- Study of the mass of feces produced per day. Externally, secretory organ failure (polyfecal matter) leads to an increase in fecal mass. This indicator is observed in the later stages of the disease.-00
- Carrying out tests to study exocrine function using special probes. With their help, secretin and pancreozymin are administered, as a result of which the gland secretes pancreatic secretions of a different nature. The combination of both stimuli allows us to judge the external secretory insufficiency of the organ.
- Ultrasound.
- X-ray of the pancreas.
- CT scan of the pancreas.
- MRI of the organ.
Prognosis and possible complications
The prognosis for life with pseudotumor pancreatitis is favorable. The disease develops slowly, exacerbation occurs rarely, but in the absence of treatment the patient may experience the following complications:
- gland calcification,
- jaundice,
- vein blockage,
- peritonitis,
- diabetes,
- internal bleeding,
- degeneration of hypertrophied organ tissue into a malignant neoplasm.
Strictly following the doctor’s recommendations will allow the patient to save life and ensure stable remission.
Diagnostic methods
Diagnosis of this form of pathology consists of a step-by-step examination of the patient:
- stool, blood and urine tests are prescribed for a general clinical examination,
- performing ultrasound,
- blood for biochemistry,
- radiography,
- MRI and CT,
- endoscopic examination of the pancreatic ducts,
- histological examination for differential diagnosis with the development of a cancerous tumor in the area of the head of the gland.
Laboratory diagnostic results
Laboratory testing reveals the following in the blood:
- increased ESR concentration,
- increased level of white blood cells,
- biochemical examination shows an increase in bilirubin, lipase, trypsin and sialic acids.
Urine tests show an increased concentration of bilirubin but no urobilin, as well as an increased amount of alpha-amylase. Based on stool tests, conclusions are drawn about disruption of the digestive processes.
Abdominal ultrasound
Ultrasound diagnostics can detect an increase in the affected part of the gland, an uneven echo signal from pancreatic tissue structures, an uneven contour, narrowing or complete occlusion of the pancreatic ducts.
To obtain more complete information about the development of pathology and differentiate it from the development of cancer, a histological examination will help.
MRI of the pancreas
MRI diagnostics is one of the most highly informative ways to clarify the condition of parenchymal organs. When performing MRI or CT diagnostics, the development of the slow process of carcinoma formation is confirmed or completely excluded.
To visualize the condition of the pancreatic ducts and assess the extent of their damage during MRI, an ERCP procedure is performed, and in some situations an angiographic examination of the vascular fibers of the pancreas can be performed.
4Treatment
Chronic pseudotumor pancreatitis requires emergency treatment in a hospital setting. Complex therapy is used, the individual characteristics of which depend on the clinical picture of the disease and the patient’s condition.
First of all, patients are prescribed a special diet. The next important stage is eliminating the cause of the disease and regulating the secretory functions of the pancreas.
Therapeutic diet
If pseudotumorous pancreatitis is diagnosed at the initial stage, patients are prescribed diet No. 5, which alleviates the condition. During acute periods, fasting is recommended for the first few days, then gentle food is gradually introduced into the patient’s diet in small portions. Compliance with the treatment table is mandatory before the operation.
Drug treatment
- To eliminate pain, patients are prescribed antispasmodics (for example, No-shpa, Papaverine).
- It is mandatory to prescribe medications that regulate the production of enzymes (Pancreatin, Amylase).
- At the discretion of the doctor, additional antibacterial and other drugs are prescribed.
In the initial stages of the disease, conservative methods will help avoid surgical intervention. If surgery is necessary, after the procedure the doctor prescribes medications to stimulate the normal functioning of the pancreas and alleviate the patient’s condition.
Surgical treatment
Unfortunately, in most cases, cure for pseudotumorous pancreatitis is impossible without surgery to remove the tumor or affected part of the pancreas, as well as restore the pancreatic duct.
During the operation, the detected cysts are desquamated, and part of the removed cells is taken in order to quickly carry out histological analysis. If cancer is confirmed, the surgeon adjusts the actions during the operation.
Such methods allow doctors to achieve stable remission and avoid the development of other pathologies - diabetes and gallstone disease. However, surgery does not mean complete recovery. Patients are prescribed to follow a diet, take special medications and be monitored by a doctor.
First of all, treatment of pseudotumor pancreatitis is aimed at eliminating the cause of its occurrence, if possible. The method is selected based on diagnosis.
Surgical intervention
Surgical treatment of the disease is necessary in most cases. The operation removes the affected areas of the gland, as well as cysts and tumors of the head, body and tail. During the operation, a histological analysis of the removed tissue is also carried out for possible cancer development.
If this diagnosis is confirmed, the course of the procedure can be changed depending on the situation. It is also possible to use drainage in the area where abnormal fluid accumulates.
The operation allows you to achieve stable remissions, and also prevents complications such as diabetes and gallbladder diseases. After such therapy, the patient is prescribed a therapeutic diet, regimen, drug treatment, as well as constant monitoring by the attending physician. In rare cases, the gland needs to be re-operated.
Drug therapy
Taking medications can be effective only in the early stages of the disease. In this case, a whole range of medications is prescribed, including:
- antispasmodics and painkillers (No-Shpa, Drotaverine);
- antimicrobial agents (in some cases);
- drugs that regulate the production of pancreatic and gastric enzymes (Pancreatin, Festal);
- anticholinergics (Methyldiazyl);
- medications with an antacid effect (Almagel, Maalox).
Medicines are not able to eliminate the cause of the progression of pseudotumor pancreatitis; they are effective only as a measure to alleviate symptoms.
This type of treatment requires systematic examinations by a gastroenterologist and therapist in order to monitor results and record changes in the body. In the absence of positive dynamics, a surgical method may be prescribed.
Endoscopy
Endoscopic treatment methods are quite effective. However, they can only be used if jaundice develops of the mechanical type.
Pseudotumorous pancreatitis with damage to the head of the pancreas and stenosis are also indications for the use of endoscopy. Their presence can be determined using ultrasound examination.
Diet therapy
Changing your diet to a therapeutic one is a necessary measure in the treatment of pancreatitis of any type. Therefore, each patient must adhere to the gastroenterologist’s instructions. The best diet in this case may be table number 5 according to Pevzner.
Nutrition involves excluding the following foods:
- alcohol and carbonated drinks;
- strong coffee and tea;
- fresh baked goods;
- sour fruits, vegetables and berries;
- cabbage;
- fatty rich broths;
- meat and fish products with high fat content;
- sweets and confectionery;
- legumes;
- fermented milk products with high fat content.
Thus, nutrition can be based on the following products:
- fruits and vegetables after heat treatment;
- pasta made from durum wheat;
- low-fat dairy products;
- light soups;
- cereals and porridges;
- lean varieties of meat and fish.
You can cook dishes only with steam and water, in rare cases, perhaps bake them in the oven without adding sauces and seasonings. It is also recommended to avoid large amounts of salt and sugar.
ethnoscience
The use of traditional medicine can be dangerous if it is not agreed with the attending physician. It is also important to remember that home recipes cannot replace full treatment of a serious illness. However, this method can be combined with the main ones if used correctly.
Conservative therapy is used to alleviate the symptoms of the pathology. Eliminating the disease and preventing its further progression is possible only with the use of surgical intervention. Traditional medicine recipes contribute to the overall strengthening of the body’s immune system and gently alleviate the patient’s condition. To prevent worsening of the pathology, the patient should follow nutritional rules.
Conservative
Drug therapy can suppress pain. For this purpose, the patient may be prescribed:
- Painkillers, for example Papaverine, No-shpa.
- Drugs that affect the secretion of the gland - Gordox, Contrikal.
- Antacids Maalox, Almagel.
Medicines are taken during preparation for surgery. It is impossible to achieve stable remission with drug treatment.
Folk remedies
Alternative medicine is used to relieve intoxication of the body, suppress inflammation in the pancreas, prevent the development of concomitant diseases, and normalize sleep. Folk remedies are indicated to improve the functioning of the gland before surgery and for preventive purposes after surgery.
If pancreatitis is not treated promptly, it will lead to dysfunction of other organs. If you are diagnosed with chronic pancreatitis and its symptoms worsen, then therapy must be carried out immediately.
The patient is treated in a hospital, where he is prescribed a set of measures:
- Following a strict diet. For the first time, fasting is practiced. When the patient is allowed to eat, the food should be taken in small portions.
- Elimination of pain and spasms.
- Normalization of the digestive process.
- Replenishment of enzyme deficiency.
- Stop the inflammatory process.
- Restore damaged organ tissue.
- Carry out preventive measures.
When treating the chronic form, antibiotics are used if infection is present. This course lasts approximately 7 days. In case of inflammation of the ducts, Amoxicillin is prescribed to facilitate the outflow of bile; this allows the inflammatory focus to be stopped and prevent it from developing further.
Anti-inflammatory drugs can relieve pain. Only a doctor can competently select the dose of the drug.
“No-shpa” and “Drotaverine” will help to cope with spasms.
Chronic pancreatitis ICD code 10 is accompanied by digestive pathology, for this reason the patient must adhere to a strict diet and take enzymes.
In complex treatment, medications are prescribed to reduce the level of acidity (Almagel, Maalox).
Injections of Ringer, the drug “Hemodez” and saline have proven themselves to be effective in reducing intoxication in the body.
If therapeutic measures do not have the desired effect, then the patient is prepared for surgery.
For chronic pancreatitis, choleretic and enzyme preparations are indicated:
- Festal;
- Mezim Forte;
- Pancreatin;
- Vigeratin;
- Digestal;
- Creon.