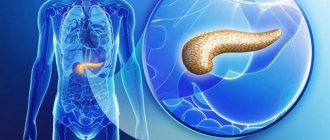
The name "pancreatitis" comes from the Latin word pancreas - pancreas. This is an organ that belongs to both intrasecretory (production of insulin and glucagon) and exocrine organs (production of pancreatin). Due to its inflammation, painful sensations occur. You can relieve the pain of pancreatitis at home, but you cannot cure it.
The pancreas lies deep in the abdominal cavity. At the back is the spine with numerous back muscles, at the front is the stomach and omentum. Therefore, the pancreas is considered one of the most protected organs from the external environment.
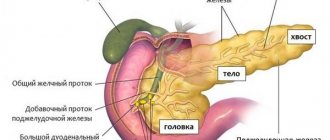
The structure of iron is similar to a comma: a large head, a prismatic body and a cone-shaped tail. The head is located in the right hypochondrium and “wound” around the duodenum.
The body and tail go to the left. This horizontal arrangement of the gland can explain the nature of pain during pancreatitis - right, left, girdling.
Pancreas functions
Production of basic enzymes and participation in digestion
This is carried out by exocrine cells - pancreatocytes. These cells are grouped into lobules, each of which has its own excretory duct.
The small ducts then merge into the common Wirsung, which joins the common bile duct, which flows into the duodenum. This connection of the ducts explains the frequent appearance of jaundice in pancreatitis.
Juice begins to be produced at the sight or smell of food. More intense production begins after food enters the digestive canal. The amount of juice directly depends on the type of food, on average - about 600 ml per day.
It contains all the necessary enzymes for the breakdown of proteins, fats and carbohydrates - trypsin, elastase, lipase, amylase. And also - nucleases that promote the breakdown of foreign proteins RNA and DNA.
Hormone production
These include insulin and glucagon, which regulate blood glucose levels and ensure normal carbohydrate metabolism. These substances are produced by endocrine cells located mainly in the tail of the gland and are released directly into the blood.
Insulin stimulates the conversion of glucose into glycogen and its accumulation in the muscles and liver. Glucagon, on the contrary, destroys glycogen and converts it into glucose.
Painkillers for chronic pancreatitis
Answering the question about what medications can be prescribed for pancreatitis, gastroenterologists note that the choice of medications directly depends on the degree of damage to the pancreas and the intensity of pain.
To relieve pain and complex therapy of aggravated chronic pancreatitis, it is advisable to use the following groups of medications.
Pancreatic enzymes
Against the background of chronic inflammation of the pancreas, the patient may develop concomitant diseases. For example, pancreatic enzyme deficiency. If this happens, the doctor prescribes enzyme preparations that can normalize the digestion process and significantly speed up the restoration of pancreatic function.
Enzymes are biologically active substances that improve the process of converting food.
Causes of pancreatitis
The pancreas can become inflamed in both adults and children for multiple reasons:
- Genetic predisposition.
- Excessive consumption of spicy, fatty, salty foods or alcohol.
- Diseases of the gastrointestinal tract.
- Cholelithiasis.
- Acute infectious diseases – chicken pox, mumps, hepatitis.
- Chronic infections – tuberculosis, syphilis.
- Obesity, diabetes.
- Liver diseases with impaired liver function - cirrhosis, chronic hepatitis.
- Malformations of pancreas – duplication of ducts, splitting of the gland, hypoplasia.
- The presence of parasites in the body.
- Cysts and malignant neoplasms of the gland.
- Gland injuries during surgery.
- Autoimmune diseases.
- Any mechanical damage.
- Long-term use of sulfonamides, corticosteroids, furosemide, tetracycline.
- Poisoning with salts of heavy metals.
- High levels of calcium and triglycerides in the blood.
- Changes in hormonal levels during various diseases and menopause.
Where does it hurt with pancreatitis and where does it radiate?
It hurts differently with acute and chronic inflammation. When the inflammation is acute, the patient feels like a stake in the chest, and chronic pancreatitis is characterized by cramping pain that increases and decreases. In only one out of ten patients with pancreatitis, the disease proceeds without pain.
In many ways, the nature of the painful manifestations depends on the degree of painful changes in the pancreas, and the localization depends on what is inflamed: the head, body or tail of the gland.
Inflammation occurring in the head of the pancreas manifests itself as pain in the solar plexus or in the right side. During the inflammatory process in the body and tail of the gland, pain is felt in the left hypochondrium.
If the entire pancreas is affected, the pain will be felt as girdling, covering the upper part of the body. Acute pancreatitis often has symptoms of angina pectoris. The patient has a burning sensation behind the sternum, pain under the left shoulder blade and jaw on the left side. The irradiation of pain under the left shoulder blade is so strong that it is similar to myocardial infarction.
Important! A painful attack in the chronic course of the disease can begin under the ribs on the right side, in the liver area, move to the left side, cover the entire abdomen and the entire torso. The abdomen is bursting, a burning sensation is felt in certain places and throughout the abdomen.
Also, chronic pancreatitis is manifested by pain in the lower abdomen, radiating to the groin, back pain in the kidney area. A painful attack is possible when the pain is localized in the navel area. Sometimes it hurts in several places at the same time.
Symptoms of gland inflammation
Acute pancreatitis
The pain with pancreatitis of this type is acute and severe. It can be localized in the right, left hypochondrium or have a surrounding character, depending on the localization of the process in the gland. Often - nausea and vomiting, which does not bring relief.
Bile inclusions can be seen in the vomit. Bloating and bowel disorders - diarrhea or constipation. Deterioration of general condition – shortness of breath, sweating, rise in temperature.
Chronic pancreatitis
Pain in chronic pancreatitis is characterized by less intensity, in the same location. There is an increase in pain an hour or an hour and a half after eating. Often accompanied by nausea, belching and heartburn.
Pain is often accompanied by flatulence, diarrhea and steatorrhea - the presence of undigested fats in the stool. Appetite is reduced. With a long course, weight loss, yellowness of the skin and mucous membranes are possible.
Painkillers for acute pancreatitis
Since the acute form of pancreatitis is accompanied by very severe pain, the primary task of providing medical care is pain relief.
For this purpose you can use:
- analgesics;
- antispasmodics;
- narcotic and psychotropic drugs.
Injections
Pain in acute pancreatitis can be quickly relieved with the help of non-steroidal analgesics, which are administered intramuscularly. First of all, we are talking about No-shpa, Atropine, Analgin and Paracetamol. These medications are often prescribed with antihistamines (Diphenhydramine or Suprastin).
If the listed remedies are ineffective and the pain continues to increase, the patient may be prescribed narcotic drugs. Thus, drugs such as Tramadol, Promedol or Omnopol will help cope with extremely acute pain during exacerbation of pancreatitis.
Strong painkillers for pancreatitis can only be used as prescribed by a doctor and only in a hospital setting
Pills
In acute forms of the disease, tablets are prescribed to restore pancreatic function. They are selected by the doctor individually for each patient, depending on the degree of damage to the pancreas and the presence of concomitant diseases.
Typically, patients are prescribed diuretics to relieve intoxication of the body, drugs to reduce enzyme activity, antibiotics in case of a bacterial infection, hepatoprotectors to maintain liver function, antiulcer drugs and general restorative drugs.
Antispasmodics
Antispasmodics are designed to quickly and safely relieve spasms in acute pancreatitis and relieve mild pain. This group of drugs includes Papaverine, Platiphylline, Atropine.
What to do if pancreatitis worsens
Acute pancreatitis is classified as an “acute abdomen” and requires immediate hospitalization. Before the ambulance arrives, the patient should be provided with complete rest - lie on his back with his legs bent: this will reduce blood supply and reduce inflammation of the pancreas.
Apply an ice pack to the epigastric area. Self-treatment and taking painkillers are contraindicated so as not to “blur” the clinical picture.
Important. Do not heat! Do not feed the patient! The three basic principles are cold, hunger and peace.
Eliminate soreness at home
The formation of acute painful sensations of a sharp nature during a developing attack of pancreatic pathology manifests itself unexpectedly, and, basically, first aid must be provided at home or in a work environment. One of the main conditions for how to relieve an attack and anesthetize a patient is to follow the following recommendations:
- providing the sick person with a state of complete rest on the physical and emotional level,
- taking a sitting position, bending slightly towards the knee joint, or if the attack happened at home, taking the “embryo” position,
- Short-term delays in breathing and shallow breathing will also help reduce pain,
- complete exclusion of the consumption of any food products,
- If you have a desire to vomit, you should not use a variety of medications and solutions for bowel cleansing procedures. You need to induce vomiting by pressing two fingers on the area of the base of the tongue,
- do not use drugs developed on the basis of pancreatic enzyme components and drugs that have an analgesic effect. Since such actions do not allow the emergency specialist to assess the seriousness of the situation and make the correct diagnosis,
- it is necessary to ensure a constant supply of fluid to the patient’s body in the form of an alkaline drink or a weak tea drink, 50 ml every half hour,
- It is recommended to apply a heating pad or a plastic bottle with ice to the area of the most acute manifestation of pain. Cold will help relieve spasms in the muscle tissue of the gland,
- Among the medications, it is recommended to take a tablet of the domestic drug Drotaverine. And in order to relieve pain as quickly as possible and improve the general well-being of the patient, it is necessary to administer No-Shpu by intramuscular injection,
- and the last thing to do is call “03” and call the appropriate service.
After the patient is hospitalized in the intensive care unit or surgery and an accurate diagnosis is made - “acute pancreatitis”, schemes for further treatment and pain relief for the patient begin to be developed with strict adherence to bed rest.
In order to relieve pain, specialists can prescribe one of the following pain-relieving medications:
- Promedol,
- Novocaine for setting up novocaine blockade,
- Ketonov,
- Tramadol.
Acute pancreatitis and all painful signs of its manifestation can be eliminated through the use of medications such as antidepressant drugs, tranquilizers, neuroleptics, antiseptics, etc.
Analgesic drugs, in order to relieve pain as effectively as possible, should be combined with antispasmodics, antibiotics, and inhibitory drugs that promote the deactivation of enzymatic components in the pancreas. In addition, a saline, protein and detoxification solution is infused.
Only a comprehensive medical approach to eliminating acute pancreatitis can give effective results and improve the patient’s overall well-being in a short time.
How to relieve pain with chronic pancreatitis
If the diagnosis is firmly established, you can provide assistance at home yourself. Non-narcotic analgesics - Analgin or isopropionic acid derivative - Ibuprofen have a good effect.
The pyrazolone derivative Maxigan is an analgesic-antispasmodic, has an effective combined effect, and is suitable for pain relief.
To relieve pain from pancreatitis, you can use atropine drugs - Bellastesin and Bellataminal. Their side effects are dry mucous membranes and rapid heartbeat.
Taking myotropic antispasmodics (Duspatalin, No-shpa, Papaverine, Drotaverine) and neurotropic (Buscopan) relieves spasms, reduces pain and normalizes stomach function.
A nitroglycerin tablet under the tongue relieves spasms and pain well.
Drugs that reduce the secretion of hydrochloric acid: Omez and Omeprazole (proton pump inhibitors), Almagel (antacid). They also relieve pain.
Cimetidine and Famotidine also reduce acid production in the stomach by blocking the release of histamine. But recently they have begun to be used much less frequently due to a pronounced “withdrawal syndrome” when stopping treatment with these drugs.
Enzymes – Mezim and Mezim-forte, Enzistal, Panzinorm and Creon. Take two tablets three times a day during or after meals. You can drink it with alkaline mineral water.
Important. During fasting, use is contraindicated!
These products stimulate the breakdown of proteins, fats and carbohydrates. Enzyme preparations containing bile - Festal, Enzistal, Digestal - are not recommended.
To improve gastrointestinal motility - Cerucal and Motilium. Cerucal can also be used to relieve nausea and vomiting.
Alkaline mineral water – Borjomi, Essentuki, Narzan.
Lipoic acid and vitamins of all groups.
Herbal medicine: herbs for pain in pancreatitis
Pour 50 grams of chopped chicory root into one and a half cups of boiling water. Leave for two hours. Divide into several steps. Drink before meals. Instant store-bought chicory can be used instead of coffee - it tastes great. In addition, it has a sedative effect.
Using the same recipe, prepare an infusion of dandelion root.
Prepare a mixture of equal quantities of dried chamomile, dried flowers, calendula, St. John's wort and horsetail. Brew one teaspoon of the mixture with a glass of boiling water. Divide into several steps. Drink before meals.
Pour two teaspoons of cumin seeds into a glass of boiling water, leave for two hours, drink before meals during the day.
Brew a tablespoon of a mixture of equal parts of motherwort, immortelle and calendula with a glass of boiling water. Take during the day before meals.
Folk remedies for pain with pancreatitis
Freshly squeezed juices from vegetables with a low content of organic acids work well.
Squeeze juice from one carrot and two potatoes. Drink on an empty stomach in the morning for ten days.
Drink 50 ml of potato juice in the morning before meals for ten days.
Take pumpkin juice using the same recipe.
Boil oatmeal jelly in water. Use as a main dish or drink one third of a glass three times a day before meals.
Mechanism of pain development
The development of pain in chronic pancreatitis can be influenced by various factors and various processes developing in the gland. How long exactly does chronic pancreatitis hurt? The severity of these pains depends on many aspects. The following factors can provoke pain:
- weakening of microcirculation in tissues (reduced oxygen delivery to cells, development of ischemia);
- blockage (obstruction) of the gland ducts;
- pathological changes in the pancreas that are inflammatory and dystrophic in nature.
The acute form of the pathology is caused by inflammatory changes in the organ itself, i.e. pancreas. Therefore, the following symptoms are observed:
- strong pain;
- development of swelling;
- violation of the functional abilities of the organ;
- acquiring an unhealthy color (redness).
Inflamed pancreas
Swelling develops against the background of excessive fluid accumulation, which has a negative effect. In the process, swelling puts pressure on the gland tissue.
Further, the development of dystrophic areas is observed, which can be either in the form of single foci or total damage to the organ.
In this case, there is a clear violation of the integrity of the pancreas, so the pain syndrome with pancreatitis has an increasing character.
Chronic pancreatitis is caused by less intense inflammatory processes. This form of pathology is characterized by the development of microcirculation disorders and the formation of connective tissue instead of glandular tissue. As the pathology develops, various types of neoplasms may be diagnosed in some areas of the gland. As a result, compression of areas occurs, including healthy ones, which leads to disruption of the outflow of enzymes; pain in chronic pancreatitis becomes more intense.
Where exactly does it hurt in chronic pancreatitis, how to determine the pathology? Most often, the patient observes pain in the center of the abdomen closer to the right hypochondrium. In this case, the pain is aching in nature, in contrast to the acute form of the disease.
The location of pain during pancreatitis is in the center of the abdomen closer to the right hypochondrium