Diagnosis of chronic pancreatitis: research methods
Diagnosis of chronic pancreatitis consists of basic and additional methods.
How can you identify pancreatitis? When examined on the skin of a patient with chronic pancreatitis, hemorrhagic rashes in the form of purple droplets up to 1–4 mm in size can be seen. These are pinpoint angiomas that occur as a result of proteolysis, a destructive effect on the capillaries of pancreatic enzymes released into the blood during an exacerbation of the process (Tuzhilin’s symptom).
After examination, objective symptoms of pancreatitis are determined:
1. Desjardins' symptom - pain on palpation is determined at the pancreatic point of Desjardins (projection of the head of the pancreas), located 4-6 centimeters from the navel along the line connecting the right axilla with the navel.
2. Shoffard's symptom - pain is detected in the Shoffard's area (projection of the head of the pancreas), located 5-6 centimeters above the navel on the right side between the bisector of the umbilical angle and the midline of the body.
3. Mayo-Robson symptom - pain is determined at the Mayo-Robson point, the projection of the tail of the pancreas, at the border of the middle and outer third of a line segment drawn through the navel, the left costal arch and the axillary region on the left. In this case, pain can be detected in the Mayo-Robson area, the left costovertebral angle.
4. Gubergrits-Skulsky symptom – palpation is painful along the line connecting the head and tail.
5. Grotta's sign - to the left of the navel in the projection of the pancreas, hypotrophic changes in the subcutaneous fat are determined.
6. Mussi -Georgievsky symptom - positive phrenicus - symptom on the left.
7. Kacha's symptom is a symptom of pancreatitis, in which palpation is painful in the projection of the transverse processes of the right T1X-TX1 and left TVIII-TIX thoracic vertebrae.
8. Voskresensky’s sign – in the projection of the pancreas the pulsation of the abdominal aorta is not detected.
After the examination, it is necessary to prescribe a number of mandatory research methods, as well as tests for pancreatitis. The laboratory examines once:
1.
General blood test can reveal inflammatory changes (leukocytosis, shift to the left of the leukocyte formula, acceleration of ESR)
2. Biochemical blood test (total bilirubin and its fractions, AST, ALT, alkaline phosphatase, GGTP, amylase, lipase, glucose, total calcium, proteinogram ):
- An amylase test during exacerbation of chronic pancreatitis reveals an increase in amylase levels in the blood 2 - 3 hours after the onset of relapse and persists for 2 - 6 days. Hyperamylasemia for more than 6 days indicates the development of complications (formation of pancreatic pseudocysts);
- The lipase test is more specific. The level of lipase in the blood increases 5-9 times from the 4th day from the onset of an exacerbation and persists for up to 10 days.
3. A general urine test determines inflammatory changes.
4. Diastasis in urine increases in direct proportion to the increase in blood amylase levels. Already in the first hours of relapse, its level can reach 100-200 norms.
5. In the coprogram, steatorrhea is determined (the presence of more than 5 grams of neutral fat in the stool when consuming 100 grams of fat in the daily diet), creatorrhoea (determination of muscle fibers with transverse striations in the stool) and amilorrhea (the appearance of starch in the stool).
Mandatory instrumental research methods include:
1. Plain radiography of the abdominal organs can reveal stones and calcification of the pancreatic parenchyma.
2. An ultrasound of the abdominal organs is performed once, and a targeted ultrasound of the pancreas is repeated after the inflammation has subsided.
The main, constantly occurring echographic signs of chronic pancreatitis include:
- changes in the size of the pancreas (increase in the acute stage, normalization of size in the remission stage, decrease in its size during a long course of pancreatitis with the appearance of fibrosis);
- strengthening of the echo structure, which can be homogeneous (type I), heterogeneous (type II) or heterogeneous (type III). Often, in the conclusion of a functionalist, such changes in echostructure can be described as “diffuse changes in the pancreas”;
- the contour of the pancreas becomes jagged, uneven, but clearly limited.
There may be a number of additional echographic signs indicating the presence of chronic pancreatitis: identification of pancreatic cysts, dilation of the ductal system and the Wirsung duct in particular, duodeno- and gastrostasis, effusion into the abdominal cavity, the presence of calcifications, signs of compression of the inferior vena cava.
3. Endoscopic retrograde cholangiopancreatography (ERCP), which helps to identify indirect signs of damage to the pancreas by changes in the flow-excretory system of the gland.
After a complete examination, a consultation with an abdominal surgeon and endocrinologist is mandatory. According to indications, it is possible to prescribe additional research methods.
Laboratory research methods may require:
1. Elastase test - an enzyme immunoassay method is used to determine an increase in the level of elastase-1 in the blood, which lasts longer than an increase in lipase and amylase.
2. Detection of a tumor growth marker (CA 19.9).
3. Detection of inflammatory cytokines (interleukins 1, 8, tumor necrosis factor)
4. Determination of coagulogram.
5. Glucose tolerance test.
To identify insufficiency of exocrine pancreatic function, perform:
1. Determination of elastase-1 in feces using enzyme immunoassay. Mild and moderate degrees of exocrine pancreatic insufficiency are determined when 1 gram of feces contains from 100 to 200 mcg of elastase -1, severe degree - less than 100 mcg of elastase -1 per 1 gram of feces.
2. The bentyramine test is positive during exacerbation of chronic pancreatitis, that is, within 6 hours after administration of the drug, less than 50% of bentyramine was excreted in the urine.
3. Lund test, secretin-pancreozymin and starch test, which give positive results in case of exacerbation of pancreatitis.
To determine intrasecretory pancreatic insufficiency, the following is carried out:
1. Determination of blood glucose levels (fasting hypoglycemia is observed at the onset of the disease), fasting and/or postprandial (after eating) increases in blood glucose are observed subsequently continuously or during periods of exacerbation of pancraetitis.
2. You may also need to perform a glucose tolerance test, measuring C-peptide and glucagon levels in the blood.
Additional instrumental research methods are sometimes prescribed:
1. Spiral computed tomography, which reveals a number of changes in chronic pancreatitis: the contours of the pancreas are determined to be diffusely uneven, the size of the organ is increased or decreased depending on the form of the disease.
2. Plain radiography of the chest organs can determine the limited mobility of the dome of the diaphragm, the high location of the left dome of the diaphragm, unevenness and blurring of the contour of the diaphragm, and the appearance of effusion in the left pleural cavity.
3. FEGDS with visualization of the major duodenal papilla reveals probable signs of an inflammatory process in the pancreas and, sometimes, the reasons for its development. Bulging of the posterior wall of the stomach body may indicate an increase in the size of the pancreas. The appearance of ulcers in the gastric and duodenal mucosa and the development of reflux esophagitis often accompanies the course of chronic pancreatitis. With secondary pancreatitis, changes in the biliary tract can be detected, such as hyperemia and swelling of the mucous membrane of the duodenum, dyskinesia of the postbulbar part of the small intestine, pain when passing a duodenoscope into the postbulbar part of the duodenum.
4. It is also possible to perform laparoscopy with targeted biopsy of the pancreas, angiography, more often by celiacography, radionuclide cholecystography, or less often, diagnostic laparotomy.
Diagnosis of the disease
Based on general signs of malaise, it is impossible to immediately make a diagnosis and say that pancreatitis is certainly present. In addition to the form of the disease, several types of pancreatitis with various complications are known. A thorough examination is carried out to make a diagnosis. It will be necessary to take tests, conduct an ultrasound examination and a full examination of the patient.
The examination is carried out by palpation according to the established methodology. The method is based on a person’s feeling of pain in certain places during palpation and percussion of the area under study; each case is characterized by special symptoms. Symptoms of pancreatitis are named after the authors, named after the doctors who studied these symptoms: Kerte's symptom, Mayo-Robson, Voskresensky, Kach, Razdolsky, Mondor.
The principle of palpation for pancreatitis
This method has been used since the mid-20th century, when it was not possible to use special equipment for diagnostics; doctors trusted their fingers during examination. And now palpation and percussion are included in the research complex for making a diagnosis.
In a healthy person, the pancreas cannot be palpated. The only thing that will help is excellent knowledge of the anatomical structure of the human body. You can feel the pulsation of the aorta on the anterior abdominal wall during examination, a large vascular trunk lying on the spine. When palpating and percussing the pancreas, it is necessary to observe changes in the nature of the patient's pain.
Characteristic signs of pathology
With the Mayo-Robson symptom, pain is felt at a point located in the pancreas itself. Such a point is located on the left side in the corner of the costovertebral view. Unpleasant sensations, and then severe pain, begin with inflammatory processes in the pancreas.
With the Mayo-Robson symptom, pain is felt at a point located in the pancreas itself.
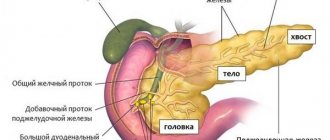
As for the anatomical topographical basis, the gland is usually located approximately at the level of the first lumbar vertebra. The longitudinal axis is located at an oblique angle from bottom to top and from right to left.
In the maximum right position, the head of the organ can be located 70 mm closer to the outer side of the spine. At this time, the tail extends approximately 30 mm into the left area of the spine. The body of the gland does not extend, but is completely superimposed on this contour.
In the maximum left position, the head of the gland is located opposite the spine, but the tail and body of the organ can be located approximately at a distance of approximately 90 mm from the left side of the spine.
Inflammatory processes in the pancreas lead to a pancreatic attack. The acute syndrome, in its symptomatic picture, resembles poisoning: vomiting and diarrhea appear. But with the release of the masses there is no relief - the person still feels very sick.
Other characteristic signs of pathology include the following:
- severe pain in the upper abdomen;
- increased body temperature;
- yellowing of the sclera of the eyes;
- grayish complexion, circles under the eyes and sharpened facial features;
- tachycardia;
- jumps in blood pressure;
- shortness of breath;
- putrid smell of feces;
- taste of bile and dry mouth.
Chronic inflammation of the pancreas is more difficult to diagnose than acute pancreatitis. If the patient complains of lack of appetite in the morning, significant weight loss and frequent aching pain in the epigastric region, he is referred to a gastroenterologist for consultation and confirmation (or denial) of suspicions of pancreatitis.
Symptoms of acute pancreatitis, determined by a specialist
The abdomen is limited in mobility. Its swelling is recorded over the entire area of the peritoneum. There is unbearable pain when pressing on the upper part of the epigastric region and complete or sharply reduced hearing of the sounds of intestinal peristalsis.
Further progression of pain and other symptoms of pancreatitis may indicate the development of peritonitis. In particular, this formidable complication can be supported by increased pain even with a light touch of the peritoneum, as well as “board-shaped abdomen syndrome”, which consists of its uniform density over the entire area and complete exclusion from respiratory movements.