Erosive gastritis is an acute or chronic inflammation of the gastric mucosa, the main feature of which is a violation of the integrity of the mucosa with the formation of erosions. The disease occurs more often with increased acidity of gastric juice. A characteristic feature is varying degrees of bleeding.
Symptoms of the disease in adults: abdominal pain, heartburn, vomiting with dark, almost black blood, melena.
The drug treatment regimen includes: eradication of Helicobacter pylori, normalization of the pH of gastric juice, protection of the gastric mucosa (GMU).
In the article, we will look in more detail at what erosive gastritis is, its symptoms and treatment with medications.
Table of contents
- Erosive gastritis - what is it? Does erosive gastritis turn into cancer?
- Acute erosive gastritis
- Symptoms
- Acute erosive gastritis
- What fruits can you eat with erosive gastritis?
Treatment
Therapy for this disorder should consist only of a complex of drugs, which consists of:
- drug therapy;
- folk remedies;
- special diet.
Treatment of erosive gastritis with medications is aimed at eliminating the symptoms of the disease. Often prescribed:
- substances that relieve pain spasms;
- antibiotics;
- anti-inflammatory drugs;
- medications that bring stomach acidity back to normal;
- enzymes - to facilitate digestive processes;
- drugs that help restore the integrity of the mucous membrane;
- medications that reduce the concentration of aggressive acid;
- antibacterial agents;
- hemostatic agents.
Treatment of erosive gastritis with folk remedies combines:
- tincture of propolis and sea buckthorn oil;
- egg whites, which must be consumed internally;
- decoction of centaury and mint;
- medicine made from honey, aloe leaves, cocoa and animal fat;
- a decoction of a mixture of calendula flowers and medicinal chamomile;
- infusion of honey and olive oil;
- tea based on rosehip and fennel.
Traditional methods of therapy can be used only after being prescribed by the attending physician. Such remedies should not become the only method of treatment. In combination with medications, folk remedies will give results after a few weeks of use.
The diet for erosive gastritis of the stomach consists of:
- balanced and vitamin-enriched nutrition;
- eating small portions, six times a day;
- avoidance of salty, spicy and fatty foods;
- ban on alcoholic drinks, fresh juices, strong coffee;
- restrictions on the consumption of baked goods. You can only eat dried bread;
- eating only lean meats or fish, prepared without adding oil or boiled;
- eating warm food - it should never be too hot;
- cooking porridges and soups using water or vegetable broths;
- taken in any number of compotes.
It is worth noting that without following a special diet, drug treatment will not give the expected result.
Erosive gastritis - what is it?
Erosive gastritis is an acute or chronic inflammatory disease of the stomach, the distinctive feature of which is the occurrence of single or multiple erosions in the coolant.
Acute gastritis occurs due to short-term exposure to damaging factors (trauma, burns, intoxication, poor-quality food); almost the entire coolant is involved in the process, giving a pronounced clinical picture.
Symptoms of acute erosive gastritis:
- stomach ache;
- temperature;
- dyspepsia;
- vomiting mixed with dark blood;
- melena;
- severe weakness, fainting state.
Treatment of acute erosive gastritis is aimed at:
- rapid cessation of the damaging factor;
- rapid relief of symptoms of acidism (increased secretion of pepsin and hydrochloric acid) and normalization of stomach pH;
- strengthening the regeneration processes of damaged mucosa.
The main cause of chronic erosive gastritis (CEG) is an imbalance between damaging factors acting on the coolant and protective factors of the digestive system. The most common form of CEG is antrum gastritis, provoked by Helicobacter pylori infection. The inflammatory process, localized in the outlet section of the stomach, quickly spreads to the duodenum and its bulb, causing the clinic of duodenitis and erosive bulbitis, and the function of the pyloric sphincter is disrupted.
Gastric erosion: symptoms and treatment
The reflux of the contents of the duodenum into the stomach further damages the antral mucosa, which leads to the occurrence of erosive-hemorrhagic gastritis.
Further development of Helicobacter pylori infection leads to the death of parietal cells with mucosal atrophy, and foci of atrophic gastritis appear, which tend to expand.
Despite such a bright endoscopic picture, the clinical picture of the disease is quite poor. Therefore, the disease goes undiagnosed for a long time.
In the treatment of erosive gastritis, the following groups of drugs are used:
- antibiotics (for eradication of Helicobacter pylori according to generally accepted schemes);
- drugs that normalize the pH of gastric juice;
- gastroprotectors;
- prokinetics;
- antispasmodics.
Does erosive gastritis turn into cancer?
There is no consensus among scientists about whether erosive gastritis turns into cancer. However, no one denies that stomach cancer is preceded by chronic diseases caused by the bacterium Helicobacter pylori. It was this microorganism that was put in first place among the causes of carcinogenesis.
There is debate about whether erosive gastritis can directly develop into cancer, or whether it must first go through the stage of an ulcer or atrophic gastritis. In defense of their arguments, supporters of the direct transition of erosive gastritis to cancer say that often a cancerous tumor develops against the background of erosive gastritis, without signs of mucosal atrophy or ulcers, so they believe that erosive gastritis is a precancerous condition. Their opponents, without denying the role of chronic irritation in carcinogenesis, believe that the processes occur in parallel.
Atrophic gastritis in women: causes, symptoms and treatment
Erosive antral gastritis
The antrum is the lowest section of the stomach; it is responsible for partial alkalization of the food coma digested in the acidic environment of the stomach and its promotion into the intestines. Inflammatory diseases of this part of the stomach, accompanied by erosions, are called erosive antrum gastritis. There are acute and chronic erosive antral gastritis.
Acute erosive antrum gastritis develops very quickly, spreading to almost the entire mucous membrane and causing insufficiency of the cardia (lower sphincter of the esophagus), pyloric sphincter (located between the stomach and duodenum). Acute erosive gastritis occurs as a result of extensive skin burns, renal and liver failure, and massive blood loss.
Symptoms of acute antral gastritis:
- stomach ache;
- heartburn;
- vomiting mixed with dark blood;
- Melena – foul-smelling, loose, black stool (due to the presence of blood).
This is one of the most severe types of gastritis, requiring rapid treatment.
Chronic erosive antrum gastritis occurs when there is an imbalance of damaging and protective factors acting on the gastric mucosa. The immediate cause of the disease is Helicobacter pylori.
A predisposing cause may be a violation of the body's protective functions: with HIV infection, chronic alcoholism, diseases of internal organs, dietary disorders (abuse of spicy foods, fasting, overeating). In its development, chronic erosive antral gastritis goes through several stages:
- superficial gastritis;
- focal erosive gastritis;
- widespread antrum gastritis with transition to the duodenum, resulting in bulbitis and duodenitis.
Symptoms of the disease:
- constant or intermittent abdominal pain;
- heartburn;
- flatulence,
- bloating;
- unstable chair.
Treatment includes:
- antibacterial therapy;
- agents that reduce the pH of gastric juice;
- gastroprotectors;
- prokinetics;
- antispasmodics.
Erosive-hyperplastic gastritis, a disease of unknown etiology, often occurs against the background of a gastrin-producing tumor of the pancreas, stands apart. The diagnosis is made by endoscopy. With this disease, significant hyperplasia of the mucosa is detected, mainly due to parietal cells, which leads to a significant increase in the production of hydrochloric acid with the formation of multiple erosions, and subsequently ulcers. The danger of the disease is the frequent malignancy of mucosal defects and the risk of massive bleeding.
Signs of the disease
Erosive antral gastritis is an inflammation of the gastric mucosa at the site of its transition into the duodenum with the formation of specific lesions - erosions.
What is the "antrum"?
In the antrum, which is the last section of the stomach on the way of food to the intestines, mechanical grinding, mixing and formation of a food coma occurs. Hydrochloric acid in food is also neutralized there so as not to interfere with the work of small intestinal enzymes. HCl is deactivated by protective mucus and bicarbonates secreted by the epithelium.
What does stomach inflammation look like?
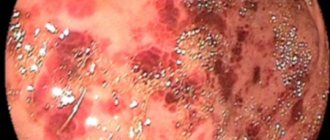
Today, the following types of erosions of the antrum of the stomach are identified:
- Full, they look like cone-shaped growths with a depression in the center, surrounded by red, swollen mucosa. They are located in numerous groups and indicate chronic inflammation of the stomach.
- Superficial - flat growths of epithelium of various shapes and sizes. A rim of hyperemic tissue forms around them.
- Hemorrhagic - small, needle-prick-like dots on the mucous membrane from cherry to deep red. They are also surrounded by a swollen rim of hyperemic mucosa. The edges of erosions are bleeding.
Another name for this disease is erosive antrum gastritis. In the initial stage, it has superficial damage without affecting the deep layers of the mucosa. The progression of the pathology leads to increased secretion of hydrochloric acid. Erosion increases in size and damages the walls of small mucosal vessels. Bleeding of varying intensity begins (depending on the area of the lesion and the size of the vessel). This is the hemorrhagic stage.
How does the disease progress?
During the course of the disease, two forms are distinguished:
- Acute erosive antral gastritis occurs due to food or toxic poisoning. Characterized by rapid development of symptoms. More common in children.
- The chronic form lasts for years, at first it proceeds secretly, but the pathology tirelessly progresses, leading to complications in the form of stomach and duodenal ulcers or erosive antral gastropathy. A digestive abnormality common in adults.
Antral erosive gastritis is a disease in which swelling of the pylorus (the muscular ring between the stomach and duodenum) occurs, followed by narrowing of its walls. The evacuation of food from the stomach to the intestines slows down. Stagnation of the food coma with fermentation occurs. The acidity of gastric juice increases.
How does the patient feel?
In acute cases, after taking an irritating substance, vomiting appears, sometimes mixed with blood. The subsequent meal provokes sour belching with heartburn, which in rare cases takes the form of a cough. Traces of microscopic hemorrhages are observed in the stool.
Signs of a chronic course are:
- abdominal pain on an empty stomach or an hour after eating;
- nausea after eating, sometimes vomiting brings slight relief;
- belching bitter, sour, rotten;
- constant discomfort in the stomach;
- heartburn, flatulence, rumbling;
- The stool may be coffee-colored due to the high content of digested blood. This is possible with severe bleeding of ulcers and erosions;
- constipation as a result of impaired gastric motility and intestinal peristalsis;
- diarrhea caused by activation of opportunistic microflora due to a decrease in local intestinal immunity;
- weakness, fatigue, headache, dizziness;
- disruption of physiological processes as a result of poor absorption of nutrients and vitamins;
- anemia due to blood loss.
Clinical manifestations increase in waves, alternating periods of exacerbation and attenuation. Some relief comes with treatment aimed at relieving symptoms, but not eliminating the cause of the disease.
Symptoms of erosive gastritis
There are acute and chronic forms of erosive gastritis. If acute EG occurs with clear symptoms, then chronic EG proceeds for a long time practically asymptomatically, or with scant symptoms. Most authors emphasize that there is no clear correlation between the severity of changes in the gastric mucosa and the clinical picture of the disease.
Symptoms of erosive gastritis of the stomach in adults:
- dull pain in the abdomen;
- abdominal discomfort;
- nausea, belching;
- flatulence;
- loss of appetite.
Typically, patients ignore such symptoms, preferring to be treated with folk remedies. Signs of the disease become more obvious during the period of manifest manifestations with bleeding (vomiting with blood, melena), when the disease is diagnosed.
Acute erosive gastritis
Acute erosive gastritis is a disease that develops quickly with short-term exposure to pathogenic factors. As a result, total damage to the mucous membrane occurs.
In acute gastritis, the symptoms are as follows:
- severe weakness;
- temperature;
- dull pain in the abdomen;
- vomiting blood;
- diarrhea;
- melena;
When the antrum is involved in the process (antrum gastritis), the disease very quickly spreads to the bulbar region and the entire duodenum, giving the clinical picture of bulbitis and duodenitis. Signs of insufficiency of the pyloric sphincter appear, which is a prerequisite for the appearance of erosive-hemorrhagic gastritis.
Chronic erosive gastritis
CHE occurs in conditions of prolonged eating disorders, chronic exposure to alcohol and other dietary disorders. The most common form of CEG is antrum gastritis associated with H. Pylori. A disease appears superficially, like catarrhal gastritis. The process develops in the area closest to the duodenum, and this gives rise to its inflammation (duodenitis). Further development of the disease leads to reflux gastritis (type C) and erosive-hemorrhagic form of gastritis.
Symptoms of chronic erosive antrum gastritis:
- moderate abdominal pain;
- feeling of tightness in the stomach;
- dyspeptic symptoms;
- vomiting, sometimes with blood;
- flatulence;
- unstable chair
- severe weakness.
The chronic form of antrum gastritis is dangerous because with prolonged development and transition to erosive-hemorrhagic gastritis, internal bleeding may develop.
Symptoms
Chronic erosive gastritis may have nonspecific symptoms. The most commonly observed manifestations are:
- moderate pain in the epigastric region;
- nausea;
- stool disorders;
- heartburn;
- poor appetite;
- bloated stomach;
- general weakness;
- increased sweating;
- vomiting with blood.
In the acute form of erosive antral gastritis, more pronounced symptoms are typical:
- Sharp pain in the abdomen.
- Periodic pain in the lower abdomen (usually after eating).
- Feeling of stomach constriction, burning and heaviness in the abdomen.
- Belching, heartburn.
- Nausea and vomiting.
- Diarrhea followed by prolonged constipation.
If ulcers have formed on the walls of the antrum, the pain syndrome is similar to the pain associated with ulcerative gastrointestinal tract. Pain occurs in the morning on an empty stomach or 1-2 hours after eating. Signs of bleeding with erosive antral gastritis are:
- vomiting blood;
- melena (semi-liquid black stool);
- pale skin;
- cardiopalmus.
When an exacerbation of erosive antral gastritis occurs against the background of reflux, the following symptoms will be observed:
- Belching with a bitter taste.
- Unpleasant taste in the mouth.
- White coating on the tongue.
Over time, the inflammatory erosive process causes atrophy of the glands. In this case, pain may not be felt. Appetite decreases, a feeling of fullness in the stomach is felt, the person quickly becomes full and loses a little weight.
Chronic erosive gastritis in the acute stage
CEG occurs with periods of exacerbation and remission.
The causes of exacerbation may be:
- violation of the diet and prescribed diet;
- stress, chronic fatigue;
- diseases of internal organs;
- infection with Helicobacter pylori infection;
- binge eating.
All symptoms that were previously vague become more pronounced:
- discomfort in the abdominal area during exacerbation, as a rule, turns into acute cramping pain;
- as the disease progresses and reflux gastritis develops, symptoms arise: bitterness in the mouth, heartburn, a feeling of fullness in the stomach;
- loss of appetite becomes more noticeable;
- the severity of symptoms such as nausea and repeated vomiting, especially when blood appears in the vomit, indicate not only an exacerbation, but also the progression of the disease;
- unstable stools, accompanied by flatulence and rumbling in the stomach, are frequent signs of exacerbation of erosive gastritis.
In the stage of exacerbation of chronic gastritis, it is necessary to adhere to the diet especially strictly (table No. 1 according to Pevzner). The patient is obliged to use only fresh, approved products in the menu. For treatment, drugs from the following medicinal groups are used in maximum dosages: antibiotics, drugs that reduce the pH of gastric juice, gastroprotectors, probiotics, antispasmodics.
Diet for erosive gastritis of the stomach and menu for the week
Diet
In order to speed up treatment, it is imperative to adhere to a special diet and not eat foods that can be irritants to the stomach; gastritis often occurs due to poor nutrition. Treatment must be comprehensive; without a diet, taking medications will not give a quick and positive effect.
To understand how long it will take to follow the diet, let’s consider the types of gastritis separately; the composition of the diet depends on the patient’s acidity level.
General recommendations
- Diet for gastritis - restriction of food intake. If gastritis is in an acute form, within two days, with the help of correctly selected food products, it is possible to achieve improvements in the general condition of the body during the disease.
- It is important to eat familiar dishes and not to consume an excess of a variety of foods during meals.
- You need to have dinner a few hours before going to bed.
- It is strictly forbidden to consume alcoholic beverages, smoking, sauces and seasonings, and spices.
- It is not recommended to drink water during meals - the digestive fluid is diluted and food digestion worsens. The rule applies to patients with low acidity.
- Pieces of food are chewed thoroughly to ease the work of a sore stomach.
- You shouldn't overwork yourself physically, but playing sports will be beneficial. For example, swimming or yoga will help speed up the digestive process.
Diet for high acidity
To speed up drug treatment for gastritis with high acidity, it is necessary to achieve proper stomach activity. You will have to adhere to the rules:
- You should not overeat; it is advisable to eat little and often, observing the established time for eating.
- Minimize salt intake, which causes acidity.
- Avoid fried foods completely.
- You should not eat too hot or, conversely, cold food.
- You are allowed to drink water half an hour after eating.
- It is advisable to rest after eating, lie down or just sit for 30 minutes, making it easier for the stomach to digest.
- If you have high acidity, you need to follow a diet for several months in order to forget about gastritis forever.
It will be possible to significantly reduce the treatment time for the disease if you follow the mentioned rules and try to consume the listed products:
- lean meat, cooked using a double boiler, or boiled: pork, chicken or turkey, tender veal; You should not eat smoked meat, meat broth, or canned food;
- It is recommended to choose lean fish (cod, flounder, hake, pike, pollock); Canned fish, broth and salted fish are undesirable for consumption;
- vegetables are allowed in the menu of patients with gastritis with a high level of acidity, preferably boiled and grated: potatoes, beets, carrots, cauliflower; Eating garlic, white cabbage, cucumbers, and radishes is unacceptable;
- cereals allowed include semolina, oatmeal, buckwheat, and rice;
- It is better to eat bread stale, preferably even stale; fresh baked goods are not allowed;
- Milk and dairy products have a good effect on the stomach, neutralizing acidity; consumption of fermented milk products is indicated with caution;
- soft-boiled eggs only, no more than three eggs per day;
- fruits are important, they enrich the body with vitamins and microelements, but they should not be consumed on an empty stomach; it is better to eat them grated or baked.
Diagnostics
If there are symptoms of erosive gastritis, the patient should consult a gastroenterologist. After a physical examination, an examination is prescribed using laboratory and instrumental methods, the scope of which remains at the discretion of the doctor.
Laboratory methods:
- general analysis of peripheral blood and urine;
- coprogram;
- stool test for the presence of blood;
- analysis of stomach contents and feces for the presence of microorganisms;
- immunological blood tests;
- histological and cytological analysis of a biopsy taken during endoscopy.
- conducting a breath test for Helicobacter pylori (HP-test).
Instrumental methods:
- FGDS is a method that provides the most complete data on the condition of the mucosa and allows suspicious tissue to be taken for histological examination.
- X-ray examination with contrast - determines peristalsis disorders, makes it possible to characterize the organ as a whole.
- Thermographic examination – records the body’s thermal radiation, identifying the presence of focal inflammation.
The diagnosis of erosive gastritis is mainly based on FGDS data. It is this method that makes it possible to establish the presence of gastritis, its type, localization, and spread of the process to the duodenum. With erosive gastritis, the doctor sees hyperemia of the coolant, its swelling, and erosion.
Acute gastritis - symptoms and treatment
Diagnosis begins with interviewing and examining the patient. During the conversation, the gastroenterologist clarifies what the patient ate before the signs of acute gastritis appeared, what medications he is taking, and whether he has any concomitant diseases (neuralgia, gallbladder, liver or heart disease). Objectively, attention is drawn to pale and dry skin, coating on the tongue, rashes in the area of the nasolabial triangle, bitterness and bad breath. On palpation (palpation), pain occurs in the epigastrium with irradiation to the left or right hypochondrium.
To confirm the diagnosis, various laboratory and instrumental research methods are used.
Important laboratory tests include:
- clinical blood test;
- 13C-urease breath test for antigen to Helicobacter pylori;
- biochemical blood test - allows you to identify disturbances in the functioning of the pancreas, liver, gallbladder and its ducts.
most commonly used instrumental diagnostic methods are
- radiography with a contrast agent - allows you to examine the relief of the gastric mucosa and the degree of tension of its walls;
- Ultrasound of the stomach - makes it possible to study the affected areas during a detailed examination, but does not allow collecting material for a detailed laboratory study.
FGDS deserves special attention - insertion of a thin endoscope into the stomach through the esophagus. This procedure is the optimal diagnostic method for gastric diseases [12]. It is prescribed regardless of the patient’s age. It allows you to determine the areas and extent of damage to the mucosa, assess the risk of internal bleeding and timely detect a malignant neoplasm.
The advantage of FGDS is the ability to perform a biopsy - to pinch off a small piece of tissue from different parts of the stomach. This procedure is painless and cannot cause bleeding.
The rules for preparing for FGDS are quite simple:
- a few days before the procedure, you need to give up some medications or coordinate their use with your doctor;
- 12 hours before the examination, refuse to eat (if the procedure is scheduled for the morning, then the last meal can be at 18:00, but not later).
Often patients are emotionally frightened due to the upcoming FGDS. The procedure is unpleasant, but tolerable and practically painless. As a rule, 15 minutes are allotted for it, but in the absence of pathologies, the process takes no more than 2-5 minutes.
FGDS can take place under:
- general anesthesia;
- light sedation (pain relief);
- local anesthesia.
Most often, doctors use local anesthesia - irrigation of the mucous membrane of the pharynx and the root of the tongue with a special anesthetic drug. This is a reliable method, proven over the years, which does not cause any complications and is easily tolerated by patients of any age. It allows you to reduce the gag reflex and calm the patient, without causing complications. Within 10-15 minutes the patient feels the same as before.
Anesthesia (medicated sleep) is carried out in the absence of contraindications, is easily tolerated, makes it possible to avoid negative emotions from the procedure, and also allows the endoscopist to work calmly and efficiently. Medication-induced sleep is performed in many countries around the world on a regular basis during a standard endoscopic procedure (sleep endoscopy). Local anesthesia is often an exception to the rule and is performed in the presence of contraindications to intravenous sedation, of which there are very few.
Complications after FGDS are rare. These include: dry or sore mouth, headache due to the patient’s severe nervousness. When the walls of the stomach are straightened during the procedure, belching of air may occur.
to become infected during FGDS if the equipment is processed and sterilized not manually, but in automatic installations for washing endoscopes.
Erosive-hemorrhagic gastritis
A distinctive feature of erosive-hemorrhagic gastritis is bleeding, that is, the disease occurs with a hemorrhagic component. With this pathology, it is not inflammation that is primary, but a violation of blood circulation in the capillaries and small vessels. The result of such a violation is hemorrhage and the formation of blood clots, which causes an inflammatory reaction in the coolant with leukocyte infiltration. Erosion appears on the surface of the mucosa. The pathology must be treated in a hospital.
There are two forms of erosive-hemorrhagic gastritis: acute and chronic. Acute hemorrhagic gastritis occurs with a more pronounced clinical picture.
Hemorrhagic gastritis is often the result of erosive inflammation of the antrum of the stomach, causing bulbitis and reflux gastritis.
Complex treatment of hemorrhagic gastritis necessarily includes nutritional recommendations: diet No. 1 according to Pevzner during exacerbation, and No. 5 when symptoms subside.
Symptoms
Erosive gastritis with a hemorrhagic component is characterized by the following symptoms:
- stomach ache;
- nausea;
- belching;
- vomiting dark blood;
- melena;
- dizziness, weakness.
Drug treatment regimen
Erosive-hemorrhagic gastritis requires a drug therapy regimen that should include drugs that affect all parts of its pathogenesis.
- Drugs that reduce the pH of gastric contents: OPP (Omeprazole, Nolpaza, Pariet), IRG (Ranitidine), antacids (Almagel, Phosphalugel).
- Hemostatic agents (aminocaproic acid, Vikasol, Dicinone).
- Enzyme therapy (Pancreatin, Mezim).
- Products that enhance regenerative processes (Aloe, Actovegin).
All medications are taken strictly according to the regimen prescribed by the doctor.
Erosive gastritis - how to treat
Now let's look at how to treat erosive gastritis of the stomach, and what medications are the drugs of choice. The most effective therapeutic methods for this pathology include several stages.
- Stage I: etiotropic drug treatment. Since the most common cause of EG is Helicobacter pylori infection, antibiotics are prescribed (Levofloxacin, Clarithromycin, Tetracycline, Trichopolum).
- Stage II: normalization of the pH of the stomach contents using medical means. The treatment regimen includes PPI (Omez, Nolpaza), IGR (Famotidine), antacids (Maalox, Almagel). To improve food digestion, enzyme preparations (Digestal, Festal, Mezim) are prescribed, and antispasmodics (No-shpa, Papaverine) are prescribed to relieve severe pain.
Acute erosive gastritis
OEG is the result of short-term exposure to aggressive factors (poisoning, radiation, burns), so the treatment of acute erosive gastritis is not limited to medications, but, first of all, implies getting rid of the damaging agent.
Despite the fact that OEG is a severe urgent pathology, timely urgent measures can quickly cure the patient. When the patient’s life is not in danger, tablets are prescribed for:
- blocking symptoms of acidism: PPI (Rabeprazole, Solcoseryl, Nexium), IGR (Famotidine), antacids (Almagel, Maalox);
- accelerating the healing processes of the mucous membrane (De-nol, Vikair, Solcoseryl, Dalargin);
- restoration of normal blood circulation in the stomach (Dipyridamole, Parmidine).
- sedative therapy (Tenoten).
You must take medications regularly, according to the regimen prescribed by your doctor.
Treatment of chronic erosive gastritis
Although the localization of CEG can be very different (lesser curvature, body of the stomach), it most often occurs in the antrum. The cause of chronic antrum gastritis is Helicobacter pylori infection. Treatment of chronic antral erosive gastritis includes:
- antibacterial therapy (Amoxicillin, Clarithromycin, Metronidazole);
- drugs that reduce the pH of gastric juice (PPIs, IGRs, antacids);
- drugs that normalize the peristalsis of the stomach and duodenum (Motilium, Cerucal, Trimedat, Ganaton);
- hemostatic drugs (Ditsinon, Vikasol);
- drugs that accelerate regenerative processes (Gastrofarm)
In the complex treatment of antrum gastritis, diet occupies an important place (nutrition according to the recommendations of table No. 5 according to Pevzner). To speed up the healing of the erosive process at home, use sea buckthorn oil and preparations based on sea buckthorn.
Drug treatment of antral gastritis in the acute stage
Treatment of erosive antral gastritis in the acute stage is aimed at relieving symptoms of exacerbation and preventing further development of the disease. For this purpose, medications with enveloping and cytoprotective effects (De-nol) are widely used. The treatment regimen includes the same groups of drugs as outside of an exacerbation, but in maximum doses.
Disease prevention measures
Prevention of the disease consists of following the principles of a healthy diet, quitting smoking and alcohol, moderate physical activity, and regular monitoring by a doctor. An established work and rest schedule, lack of stress, and taking care of the immune system will have a positive effect on the health of the digestive organs.
Erosive antral gastritis is a common, easily diagnosed disease. It is quite possible to cure the disease with complex therapy consisting of medications, diet, and herbal decoctions. Prevention of gastrointestinal diseases is the surest way to maintain health for many years.
We recommend: What nuts can you eat for gastritis?
Treatment of erosive gastritis with folk remedies
The most effective traditional medicine for erosive gastritis: sea buckthorn oil, black cumin oil, potato juice, propolis, flax seed. The table below contains recommendations on how to treat erosive gastritis with folk remedies.
Table 1. Effective folk remedies for the treatment of erosive gastritis
| Raw materials | Cooking method | Effect |
| Flax seed | 35 g flax seeds per 1 liter of hot water. The mixture is brought to a boil and infused for 12 hours. Recommended course duration - one and a half months | Relief of pain symptoms and dysphagia |
| Potato juice | Take 120-150 ml of freshly squeezed juice three times a day, half an hour before meals. The recommended course duration is 10 days. | Reducing inflammation |
| Propolis | Important! The patient should tolerate dairy products well. Dilute the alcohol tincture of propolis (20 drops) with a glass of milk (1 glass). Drink once a night. | Reducing the acidity of gastric juice; Bactericidal effect; Improving the functioning of the gastrointestinal tract |
| Sea buckthorn oil | Take 5 grams. oils on an empty stomach | Restoring the integrity of the mucosa; Relief of the inflammatory process; Antimicrobial action |
| Black cumin oil | Important! The patient should tolerate dairy products well. Oil (12 drops) is mixed with natural honey (200 g), dried pomegranate peels are added (1 tbsp.), Take 10 g. before meals with warm milk | Relief of dysphagia symptoms; Improved appetite; Normalization of gastric motility; Healing of affected areas of the mucosa |
What can you eat with erosive gastritis?
Diet for acute and chronic gastritis is an integral part of the treatment process. In the acute phase of the disease, diet No. 1 according to Pevzner is prescribed; when the severity of the process subsides, the patient is transferred to diet No. 5.
What can you eat with erosive gastritis:
- boiled dietary meat;
- low-fat fish;
- yesterday's or dried white bread, crackers;
- boiled vegetables in the form of puree (beets);
- well-cooked porridge in water (rice, buckwheat, oatmeal);
- soups made with vegetable broths, the vegetables in them should be pureed
- sauerkraut, stewed or boiled in small quantities;
- ginger in small quantities;
- soft-boiled chicken or quail eggs;
- fermented milk products (kefir, cottage cheese, yogurt);
- jelly, rosehip decoction, compote of raisins and other dried fruits, herbal tea (mint, chamomile);
- a mixture of vegetable juices (potato juice + carrot juice + beet juice in a ratio of 1:1:1);
- seeds, crushed nuts.
What kind of yogurt is good for erosive gastritis?
In order not to cause an exacerbation, you need to eat regularly, at the same time, in small portions, increasing the number of meals.
What fruits can you eat with erosive gastritis?
For erosive gastritis, it is better to eat fruits in pureed or crushed form. For chronic erosive gastritis, you are allowed to eat: bananas, avocados, persimmons, peaches, ripe and sweet apples and pears. Baked apples and pears are recommended, as well as fruit salads with chopped ingredients.
It is very good to take crushed berries for erosive gastritis: black currants, pomegranates, grapes.
What not to eat with erosive gastritis
Prohibited products;
- fresh bread;
- baked goods;
- fatty animal products (pork, lard, homemade sausages);
- hot seasonings and spices (garlic);
- aspic;
- "crab sticks
- beer;
- chocolate;
- ice cream;
- coffee;
- carbonated drinks.
Milk consumption for erosive gastritis should be sharply limited. You can’t drink milk in large quantities, because once it gets into the stomach, it quickly curdles, and as it precipitates, milk fat and protein are covered on all sides with food particles that interfere with the action of digestive juices. The process of digesting food slows down. Unprocessed milk enters the intestines, where it causes fermentation processes and flatulence.
What should be the dishes for erosive gastritis?
- dishes for erosive gastritis should be warm;
- products must be fresh and only from the list of permitted ones;
- You need to eat in small portions, but do not starve.
Signs of poisoning with toxic substances
If aggressive substances enter the stomach as a result of their ingestion, then acute obstruction of the gastrointestinal tract immediately occurs. In this case, the person feels pain throughout the esophagus, a burning sensation in the mouth, excessive salivation and difficulty swallowing. In this case, the secreted saliva becomes viscous.
There are signs of excruciating thirst and the inability to get enough liquid, since it cannot be swallowed.
Nausea occurs, accompanied by continuous vomiting, the mass of which contains not only food debris, but also bloody streaks, as well as remnants of the gastric mucosa. If you want to learn more about gastritis, we recommend reading this https://fb.ru/article/244285/kakoy-byivaet-gastrit-vidyi-klassifikatsiya-i-prichinyi-vozniknoveniya article, which describes all types of gastritis.
conclusions
Erosive gastritis is a pathology accompanied by significant disturbances in the functions of the gastrointestinal tract. The symptoms and treatment of the disease are quite well studied, but without adequate therapy the prognosis can be unfavorable. There is a risk of developing severe pathologies such as neoplasms.
To avoid exacerbations of the disease and progression of pathology, drug treatment alone is not enough. It is necessary to change the lifestyle that led to the disease:
- Eat regularly, choosing from the list of foods only those allowed by the diet.
- Avoid mental and physical fatigue.
- Do not drink alcohol, do not smoke.
During the period of remission, if possible, at least once a year, undergo a course of treatment in a sanatorium.