Duodenitis is an inflammation of the mucous membrane of the duodenum. It digests food evacuated from the stomach with the help of pancreatic juice and bile. In addition, the duodenum produces hormones that regulate the activity of the digestive tract.
There is an acute and chronic form of the disease. In 90% of cases it is the second option that occurs. The disease is dangerous because it can be complicated by intestinal bleeding, pancreatitis and other diseases.
At CELT you can get advice from a gastroenterologist.
- Initial consultation – 4,200
- Repeated consultation – 3,000
Make an appointment
Causes of the disease
There are many factors leading to duodenitis. The most common are the following:
- poor nutrition (abuse of spicy, sour, smoked, fried foods);
- bad habits (drinking alcohol, smoking);
- Helicobacter Pylori infection;
- uncontrolled use of certain medications (in particular anti-inflammatory drugs);
- gastritis and peptic ulcer;
- disruption of the blood supply to the organ;
- chronic liver diseases (cirrhosis, hepatitis, etc.);
- anatomical features leading to obstruction of patency;
- Crohn's disease;
- helminthiasis and others.
Symptoms of acute and chronic duodenitis
The acute course of duodenitis lasts 7-10 days, all symptoms are quickly relieved with medications. Chronic duodenitis lasts a long time, can recur several times a year, clinical signs are not so pronounced.
Symptoms of acute duodenitis:
- Pain in the epigastric region (night pain, after eating, when feeling hungry).
- Feeling of bloating, flatulence.
- Belching with a bitter taste and heartburn.
- Decreased appetite.
- Diarrhea, vomiting.
- Abdominal muscle tension.
In the absence of timely and adequate assistance, the disease can become chronic. Characteristic signs of the disease in the chronic stage:
- Disruption of the digestive process.
- Painful sensations in the epigastrium of an aching nature.
- Pain in the right hypochondrium, radiating to the back.
- Feeling of fullness in the stomach.
- Belching and bitter taste in the mouth.
Central dopamine receptor blockers
Metoclopramide - restores motor-evacuation function in the gastrointestinal tract, eliminates nausea and vomiting, heartburn, and belching. Adults are prescribed in the form of intramuscular or intravenous (slow!) injections - 2 ml 3 times a day. The course can be extended up to 6 weeks.
Cerucal - has a good antiemetic effect, promotes rapid emptying of the stomach and intestines. Prescribed orally 10 mg 3-4 times a day. For chronic duodenitis, the course of therapy can last up to six months.
Methods for diagnosing duodenitis
Diagnostics plays an important role. An incorrect or inaccurate diagnosis will affect the entire treatment. Therefore, you should not be afraid and refuse diagnostic procedures prescribed by your doctor.
Gastroscopy
- Cost: 3,000 rub.
More details
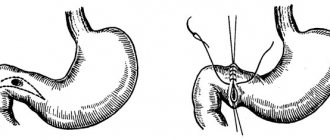
- EGDS (esophagogastroduodenoscopy) - using a flexible probe equipped with a video camera, the doctor examines the esophagus, stomach and duodenum. Using this method, you can see redness and swelling of the mucous membrane, erosion, and with a decrease in tone, smoothing of folds, the presence of nodules, hemorrhages and other signs that can be used to diagnose duodenitis.
- X-ray using a contrast agent (barium sulfate), which allows you to identify anatomical disorders, signs of inflammation, obstruction, the presence of an ulcer or tumor, signs of impaired intestinal tone and motility.
- Ultrasound diagnostics allows you to evaluate nearby organs, diseases of which can lead to duodenitis.
- A laboratory examination is prescribed (general blood test, biochemical analysis, examination for the presence of Helicobacter pylori infection, and others).
- Fecal occult blood test to ensure there are no bleeding ulcers or erosions.
- General analysis of stool (coprogram), which helps to identify signs of disturbances in duodenal digestion.
Duodenitis
Signs
Pain with duodenitis exists constantly, but intensifies after the “wrong” food (tomatoes, fatty meat, goose), at night or on an empty stomach. Pain can be over a wide area, in the hypochondrium, navel area. In young women, duodenal insufficiency begins to manifest itself in the premenstrual period. Headaches, nausea, vomiting, irritability occur, and performance decreases. Attacks of severe weakness can sometimes last for several weeks, accompanied by palpitations, heart pain, nausea, vomiting, often in the morning on an empty stomach. In this case, the ability to work and interest in life are completely lost. For many, attacks of weakness with trembling, pain in the heart, and frequent urination occur immediately after eating or after 2-3 hours, sometimes at night. A particularly painful point is the projection of the confluence of the common bile duct and the pancreatic duct (slightly to the right of the navel - under the lower point of the right rib). The pain can spread to the back and be accompanied by nausea, vomiting, general malaise, fever, and slight muscle tension in the anterior abdominal wall. All these phenomena quickly pass, leaving only heartburn, bloating in the abdomen, and mild pain in the right hypochondrium, which, undoubtedly, cannot but affect the quality of life.
Description
Duodenitis can be acute (with food poisoning, trauma to the mucous membrane by a foreign body) and chronic - associated with a disorder of the nervous and endocrine regulation of the functions of the duodenum, infection, poor nutrition, smoking, alcohol abuse, etc. Secondary duodenitis can develop with cholecystitis, pancreatitis, diseases intestines.
And yet, the main cause of acute duodenitis is a gross malnutrition. For example, a sharp change in the nature of food when traveling to Asian or African countries, where the dishes are sometimes too spicy or fatty, or simply unusual for our stomach. Inflammation of the duodenal mucosa is easily caused by eating dry food, alcohol abuse, and excessive consumption of fatty and smoked foods. Such duodenitis is accompanied by an increase in the amount of hydrochloric acid in the gastric contents.
Inflammation can also be caused by: food poisoning, poisoning with toxic substances that have an irritating effect on the mucous membrane of the digestive tract.
Infection with Giardia, chronic infection in the oral cavity, pharynx, genitals, gall bladder, kidney failure, and tuberculosis contribute to the development of duodenitis.
With repeated duodenitis, a chronic form of the disease may develop. Complications such as intestinal bleeding, perforation of the intestinal wall, and the development of acute pancreatitis occur.
Long-term duodenitis can lead to a serious complication - duodenal hormonal insufficiency, when inflammation, destroying the duodenal mucosa, causes death and inhibition of cells that secrete hormones. Contribute to the appearance of symptoms of duodenal insufficiency: congenital weakness of the endocrine apparatus of the duodenum, oxygen starvation, concomitant chronic infectious diseases. Insufficiency of the hormonal function of the duodenum causes indigestion, carbohydrate metabolism, significant weight loss or excess weight. Severe neuropsychic and cardiovascular disorders may appear
Diagnostics
The diagnosis is made by a gastroenterologist. To do this, fibrogastroduodenoscopy (FGDS) is performed, which detects inflammatory changes in the duodenal mucosa. A biopsy of the duodenal mucosa and a morphological examination of its tissues are also performed. According to indications, an X-ray examination is prescribed. If Giardia cysts, roundworm eggs, and crooked heads are found in the stool, then the inflammation is parasitic in nature. In some cases, a stool test for occult blood is done.
Treatment
Acute catarrhal and erosive-ulcerative duodenitis usually heals on its own within a few days. Treatment of other types of duodenitis depends on the cause that caused it.
If the disease is caused by parasites (giardia, helminths), then the main treatment is aimed at getting rid of them.
Treatment of acute duodenitis is carried out in combination with therapeutic nutrition. 1-2 days - fasting, bed rest, gastric lavage with a weak solution of potassium permanganate, followed by the introduction of 25-30 g of magnesium sulfate (magnesia) in a glass of warm water to cleanse the intestines. In the following days - diet No. 1a -1, astringents and enveloping agents inside, for pain - antispasmodic and analgesic drugs. To improve regeneration processes, vitamins A, B6, B12 are prescribed.
In the future, depending on the acidity of the gastric secretion, concomitant diseases and complications, dietary nutrition and drug therapy are prescribed.
Treatment is very long - sometimes up to six months or more. But it is necessary to be treated, and very carefully, in order to avoid serious complications.
Lifestyle
During exacerbation of duodenitis, a special diet is necessary. The amount of carbohydrates should be reduced to 400 g per day, protein, on the contrary, should be increased (up to 120-130 g per day). The diet should contain a lot of vitamin C, preferably in the form of fruit juices. Meals should be at least 4 times a day.
Food should be gentle on the mucous membranes of the duodenum. You can eat vegetarian cereal and pureed vegetable soups with the addition of milk and cream; meat, chicken, fish (low-fat boiled varieties, minced or in the form of meat porridge, meatballs or chicken and fish dumplings). It is allowed to include dairy products in the daily menu: pureed cottage cheese, sweet sour cream (limited), acidophilus, yogurt, kefir (non-sour), milk, cream, butter. Also allowed are soft-boiled eggs, boiled vegetables in the form of puree, cooked in milk with the addition of butter, boiled fruit in the form of puree, raw carrot juice; milk or with the addition of butter porridge, honey, sugar, fruit candies (individually and in limited quantities), white bread, white bread crackers, meringues, dry sponge cake, fresh fruit compote, jelly (except cranberry, preferably from dry rosehip, rhubarb), weak tea (preferably with milk or cream), salt is sharply limited.
After 3-4 weeks, the diet begins to gradually expand by moving to meat, chicken and fish in pieces, beef sausages, boiled sausage, omelette, cereal porridge, boiled vegetables, vegetable salads (without onions!), compotes, raw fruits and berries.
The diet quickly alleviates the condition, pain goes away, and dyspeptic disorders decrease. To prevent relapses, you need to limit smoking, drinking alcohol and spicy foods, and eat regularly.
Prevention
Rational, regular nutrition, the fight against alcoholism, timely treatment of other diseases against which duodenitis is possible.
Prevention of duodenal insufficiency consists of early treatment of duodenitis, especially in children, early detection and treatment of giardiasis, helminthic diseases, sanitation of foci of infection and intoxication. Adequate (proteins, vitamins) and timely nutrition is important.
© Dr. Peter
Treatment of duodenitis
First of all, it is necessary to normalize your diet. As a rule, a therapeutic diet is prescribed (table No. 1 in the acute stage and No. 5 in the chronic stage).
In acute cases of the disease, it is allowed to consume weak tea, cocoa, low-fat cottage cheese, eggs, oatmeal and semolina porridge, and pureed soups. Prohibited: mushrooms, peppers, sweets, coffee, fatty meat and fish, buns. During chronic exacerbation, vegetable soups, bread, lean meats (beef, chicken), and non-acidic fruits are allowed. The same things are prohibited as in the acute stage. During the period of remission, you can eat any food, but in moderation. Preference should be given to a healthy and proper diet and not to overeat.
Medicines are prescribed depending on the cause of the disease.
- Antibiotic therapy for Helicobacter Pylori infection
- Medicines to reduce acid production in the stomach.
- Preparations with an enveloping effect.
- Anti-inflammatory drugs.
- Pancreatic enzymes.
- Medicines aimed at restoring the mucous membrane (cytoprotectors).
- Antispasmodic drugs.
- If helminths are present, take medications to get rid of them.
- With high psycho-emotional stress, sedatives may be prescribed.
Attention! All medications are prescribed only by a doctor based on an analysis of the medical history, examination and research. Self-medication is unacceptable. Information about medications is given for informational purposes only.
Therapeutic nutrition for duodenitis
Drug treatment of duodenitis is important, but without proper nutrition its effectiveness will be significantly lower. If during an acute period an adult himself understands the need to limit excesses, then outside of an exacerbation many consider dietary restrictions unnecessary. This is fundamentally wrong. The duodenal mucosa suffers primarily from fatty, spicy and salty foods.
Therapeutic nutrition is prescribed taking into account the patient’s current condition and the presence of concomitant diseases. It is necessarily fractional (5-6 times), contains the physiological norm of nutrients. Milk and fermented milk products, boiled fish, cheeses, and milk soups are recommended. Boiled meat is allowed in minced form. It is also advisable to include vegetables and non-acidic fruits/berries in the diet.
Important! In order not to create a diet yourself, you can use specially designed treatment tables. Each of them is assigned its own number, and the diet is developed by specialists. Outside of an exacerbation, the treatment table can be supplemented with some products; during the acute period, you need to stick to the menu.
Complications of the disease
Since the disease is not always pronounced, many people let the disease take its course. When taking painkillers, do not rush to see a doctor. But relief of symptoms will never replace proper treatment, and its absence can lead to the following adverse consequences:
- duodenal ulcer with perforation (a through hole in the intestinal wall);
- intestinal bleeding;
- acute pancreatitis (inflammation of the pancreas);
- jaundice (if the secretion of bile from the ducts into the duodenum is impaired, bilirubin in the blood increases);
- duodenal dystrophy.
Treatment
Treatment of proximal duodenitis begins with drugs:
- Antibiotics to eliminate the original source of the disease (Amoxicillin or Amoxiclav)
- Prebiotics for antibiotic therapy
- Sorbents for removing toxins from the body
- Antispasmodics relieve symptoms (Ibuprofen, Spazmalgon, Drotaverine, Ketanov)
- Antacids restore the intestinal mucosa
- Inhibitors block the production of hydrochloric acid
- Prokinetics improve digestion (Pancreatin, Imodium, Mezim Forte)
To improve the general condition of the body, take vitamin complexes.
Prognosis and prevention
A timely diagnosis and prescribed treatment will help solve the problem of acute duodenitis. If the disease has progressed to a chronic stage, then it is necessary to regularly see a gastroenterologist. Optimally – 1-2 times a year. In general, the prognosis is favorable.
Preventive measures are aimed at eliminating nutritional problems, giving up alcohol and smoking. It is necessary to promptly identify and treat other diseases of the gastrointestinal tract. Never take medications without a doctor's prescription, especially for a long period. After all, even seemingly harmless aspirin can lead to the development of duodenitis. In the chronic course of the disease, it is useful to visit sanatoriums and resorts. Do not forget about the rules of hygiene to prevent infections with helminths and Helicobacter.
At the CELT clinic you can see a gastroenterologist, as well as undergo all the necessary examinations and tests.
Complications
If symptoms are ignored, treatment is started late or inflammation of the duodenum is chronic, there is a possibility of complications such as:
- inflammation of the serous membrane of this organ;
- extensive bleeding;
- ulcerative lesions of the stomach or duodenum;
- narrowing of the pylorus of the stomach;
- insufficiency of duodenal hormones;
- intestinal obstruction;
- purulent inflammation of the tissues surrounding the duodenum.
But, despite the high probability of such complications, the prognosis for duodenitis is favorable. If the disease is detected in the early stages, a complete cure is achieved.
There is no specific prevention for this disorder. You just need to lead a healthy lifestyle, promptly eliminate gastrointestinal diseases, follow nutritional recommendations, and undergo preventive examinations with a gastroenterologist several times a year.
Diseases of the digestive tract are quite diverse and can be caused by a variety of reasons. However, in the vast majority of cases, the pathological process develops in the mucous membrane lining the walls of the esophagus, stomach and various parts of the intestine. Duodenitis is an inflammation that develops in the epithelium of the mucous membrane of the inner wall of the duodenum. It rarely occurs in isolation and in most cases is combined with gastritis. This “combination” is called gastroduodenitis.
The pathology is quite common. According to statistics, every fifth person who consults a gastroenterologist suffers from duodenitis. The pathology is characterized by dystrophic, inflammatory and degenerative changes in the mucous membrane of the duodenum. Such processes cause disorders of the functional activity of the glandular apparatus, which is accompanied by a disruption of the structure of epithelial cells.
As a rule, as a result of duodenitis, not the entire duodenum is affected, but its sections.
Therefore, depending on the location, duodenitis occurs:
- distal, in which the upper part of this section of the digestive tract is not affected;
- bulbitis with damage to the bulb (apex), often combined with gastritis;
- diffuse (total);
- focal or local.
According to the course and characteristics of the etiology, acute and chronic duodenitis are distinguished. In the first case, only the superficial structures of the mucous membrane are involved in the pathological process. Such changes are reversible, and the integrity of the epithelium is completely restored after appropriate therapy.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Gastroscopy (videoesophagogastroduodenoscopy) | 6 000 |
| Ultrasound of the abdominal organs (liver, gall bladder, pancreas, spleen) | 3 800 |
| Fluoroscopy and radiography of the stomach | 4 800 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions