The causes of the pathological process in women have certain characteristics due to the close proximity of the intestines and reproductive organs.
In addition, we must not forget about menstruation, during which pelvic circulation changes. Another purely female cause of hemorrhoidal disease is pregnancy and labor. We will talk in more detail about other sources of the disease, as well as about the signs and modern methods of treating the pathological process.
Causes of hemorrhoids in women
The occurrence of an unpleasant disease occurs for one single most important reason - insufficiency of the veins located in the anorectal area. This condition can be either congenital or acquired during life.
The result of weakness of the walls of blood vessels is congestion in the pelvic region, impaired local circulation, and a slowdown in the outflow of venous blood from the cavernous bodies. As a result, a hemorrhoidal node is formed, which can hurt, become inflamed and bleed.
The development of anal varicose veins can be provoked by both general factors to which all categories of patients are exposed, and “catalysts” characteristic exclusively of women. Let's look at each group of reasons in more detail.
Provoking factors you need to know about
The provoking factors that initiate the symptoms of hemorrhoids in women, for the most part, represent classic examples of such a phenomenon as physical inactivity. The notorious sedentary work is the main culprit of congestion in the pelvis. Stagnation causes weakening of the venous valves and a gradual weakening of the vascular walls, which stretch under blood pressure. This is what is medically called varicose veins in the rectum.
Periodic hormonal fluctuations, which occur in the fairer sex every month, lead to varicose veins of hemorrhoidal vessels. During menstruation, blood flows to the pelvic organs, including the rectum.
An equally dangerous phenomenon for hemorrhoids is carrying a fetus during pregnancy. Here, to the gradually increasing physical inactivity, the increasing pressure of the uterus and fetus on the internal organs is added. During pregnancy, the onset of hemorrhoids in women manifests symptoms more strongly in the second and third trimesters, when the fetus is growing rapidly. The peak load on them occurs during childbirth. During the postpartum period, a woman notices obvious signs of the disease.
Stress and poor diet can increase the risk of hemorrhoids in women. Both of these phenomena negatively affect intestinal motility, as well as the circulatory system. Together, they lead to pathological expansion of hemorrhoids, constipation or diarrhea, which further injures the vessels localized in the anorectal area.
General conditions for the appearance of the disease
The general causes of hemorrhoids in women are not much different from the “male” prerequisites for the appearance of the pathological process. All of them are well studied and described in detail.
Low mobility. Many girls work in offices, where they are forced to sit at the computer for hours. In addition, there are many women who are sellers, teachers, and hairdressers. All of these professions require a sedentary lifestyle. A lack of movement is fraught with stagnation of blood in the pelvic area and hemorrhoids.- Poor nutrition. An unbalanced diet is the scourge of modern society. Today's table is replete with semi-finished products, salted and pickled dishes, smoked meats, an abundance of spices and seasonings, alcohol and coffee. All these “goodies” lead to a rush of blood to the hemorrhoidal veins.
- Constipation. This factor stems from the previous premise. An improper diet, depleted of vitamins and plant fiber, disrupts the functioning of the intestines. Constipation forces women to strain, which leads to increased pressure on the venous walls and protrusion of the cavernous bodies.
- Hard physical work. Emancipated ladies work on an equal basis with representatives of the stronger sex, including engaging in typically male types of work. The result of lifting weights is an increase in pressure in the peritoneal area.
- Lifting weights. When listing the common causes of hemorrhoids in girls, one cannot fail to note such a factor as passion for bodybuilding and body modeling in gyms. Regular lifting of loads increases intra-abdominal pressure and increases congestion in the pelvic area.
The risk group for the development of hemorrhoidal disease includes everyone who practices non-traditional sex (both men and girls). In this case, the mucous membrane of the rectal canal, as well as cavernous formations, are injured. As a result, the occurrence of hemorrhoidal symptoms.
“Female” conditions for the occurrence of hemorrhoids
In addition to the general prerequisites, there are also specific causes of hemorrhoids in women. These factors are associated with the characteristics of physiology and psychology.
- Bearing and giving birth to a child. Do pregnant women have hemorrhoids? Unfortunately, this exciting and important period in a woman’s life often provokes the appearance of hemorrhoids. Pathological formations develop due to compression of the pelvic veins by the growing fetus. All this leads to congestion in the anorectal area.
- Menstruation. This physiological feature is not the cause of the development of the disease, but can contribute to the occurrence of hemorrhoidal disease. During the regulation, the flow of blood to the pelvic area increases, the vessels become overcrowded, which is fraught (in case of predisposition) with the formation of nodes.
- Diseases of the genital organs. Inflammatory processes occurring in the female genital structures (especially of a chronic nature) often cause the appearance of negative symptoms. Experts attribute this dependence to the close proximity of the vagina, uterus and lower intestine.
- Diets. All ladies who are interested in dieting and weight loss should know that the desire to get an ideal figure is fraught with unpleasant consequences. An unbalanced diet can disrupt the intestinal microflora, worsen the functioning of the entire gastrointestinal tract, and lead to constipation.
- Reduced resistance to stress. The weaker sex reacts much more emotionally to all kinds of difficulties than men. Women are more likely to experience depression, stress, and preoccupation with problems. Together with other factors, a psychological reason can lead to hemorrhoidal symptoms.
Thus, the source of the pathological process is the weakness of the venous walls. But there are many factors that provoke hemorrhoids, and they can be both general and specific. Knowledge of the underlying causes of the disease is extremely important for the prevention and treatment of anal varicose veins.
How does hemorrhoids manifest in women?
Hemorrhoidal symptoms in women are no different from those in the stronger half of humanity. The clinical picture will depend on the type of pathological process and its severity (we’ll talk about this below).
Initial signs
These include initial hemorrhoidal symptoms, which may not bother the patient, but already require contacting a specialist for diagnosis and treatment. It is the beginning of the disease that is much easier to overcome without much time and money.
Let's look at the first signs of hemorrhoids in women:
- itchy sensations;
- feeling of heat in the anorectal area;
- bleeding during bowel movements;
- mucous discharge;
- pain during defecation;
- feeling of the presence of a foreign object in the rectum or anorectal area.
Hemorrhoids in women progress, symptoms increase, which worsens the prognosis for cure. It should also be understood that in each patient the pathological process can occur in its own way; for some, some symptoms appear earlier, while others appear much later.
Increasing symptoms of hemorrhoids in women
As the pathological process progresses, each manifestation of the disease becomes more intense and pronounced. A woman may experience the following unpleasant symptoms.
- Discomfort localized in the rectal canal or around the rectal opening intensifies. Itching and burning make themselves felt not only after visiting the restroom, but between acts of defecation.
- Bleeding from the anal canal intensifies, becoming more and more massive. If earlier it was possible to notice traces of blood on the paper, now there is heavy discharge. Interestingly, the blood does not mix with the feces, but is located on the surface of the feces.
- Soreness can appear not only during or after bowel movements, but between visits to the toilet. This is associated with the occurrence of cracks, inflammatory processes in the rectum, thrombosis of hemorrhoidal vessels and infringement of prolapsed cavernous formations.
- Mucous discharge also becomes more voluminous. At the same time, they irritate the skin in the anal area, increasing the itching and forcing women to scratch the disturbing areas. And this poses a risk of infection and the occurrence of pustular formations.
- The feeling of the presence of a foreign object in the anus also intensifies, turning into a feeling of incomplete bowel movement and a false urge to defecate. As a result, the woman tenses up in the toilet, further worsening her own condition.
The sooner treatment for hemorrhoidal disease begins, the greater the chance of avoiding an increase in negative symptoms. This should be remembered by those women who consider anorectal varicose veins to be something shameful or unworthy of attention.
Symptoms of hemorrhoids
There are two main types of hemorrhoids, they differ in the location of the hemorrhoids - internal and external. Therefore, the symptoms of these two forms of the disease are different and varied. For each woman, the disease progresses differently; for some, some symptoms appear earlier, others later.
The first signs of hemorrhoids in women are the very initial symptoms, when they appear, you should seek advice from a specialist. In the first stage of the disease, it is easier to cope with the disease; you should not bring hemorrhoids to an advanced state. The first stage lasts several months or years. Initial hemorrhoids - its symptoms:
- unpleasant sensations, discomfort in the anus
- burning, slight itching
- slight difficulty with bowel movements
Signs of external hemorrhoids:
When hemorrhoids are located low in the rectum, the symptoms of such hemorrhoids are very characteristic. The nodes come out around the anus, singly or in groups, this is accompanied by:
- Burning, itching – inflammation in this disease provokes the formation of excess mucus, which, when released from the rectum, leads to irritation and itching in the anus.
- Discomfort in the anal area - a feeling of a foreign body in the rectum, a feeling of heaviness, after stool there is a feeling of incomplete bowel movement.
- Pain in the rectum - varying in intensity from periodic tingling, heaviness to severe tugging pain.
- Bleeding is a very characteristic sign of hemorrhoids; this is blood in the stool or on toilet paper after bowel movement. This occurs from injury to the nodes by feces. If the bleeding is significant, then after defecation blood may be released in drops or streams.
- Prolapse of hemorrhoids - at first this only happens when straining; after defecation, the nodes reset themselves, but as the disease progresses, the patient has to set the hemorrhoids himself. In advanced cases, when swelling and inflammation are severe, this becomes impossible.
Signs of internal hemorrhoids:
The symptoms of internal hemorrhoids are similar to external ones; women also experience discomfort, burning, itching, pain in the rectum and anus, bleeding, especially if there is constipation. But it is impossible to see hemorrhoids, since with internal hemorrhoids they do not fall out. This makes diagnosis difficult, so the doctor has to use additional instrumental examination methods.
Signs of acute hemorrhoids:
This is how newly diagnosed hemorrhoids can occur and the chronic process can worsen:
- Sudden sharp pain even with the slightest movement, tingling, twitching, impossible to sit or walk. Emptying sharply intensifies it.
- The node becomes bluish, swollen, tense
- The temperature rises when an infection gets into the strangulated node.
Chronic hemorrhoids occur in waves: periods of remission and well-being are followed by periods of exacerbations and relapses. During relapses, similar symptoms of hemorrhoids appear in women.
Stages of “female” hemorrhoids
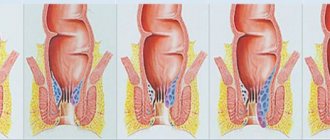
The severity of symptoms will depend on which of the successive stages the hemorrhoidal disease is at. Experts identify only 4 stages of the pathological process (below are photos of each degree of the disease).
- 1st stage. Hemorrhoids begin with changes in cavernous formations. They protrude slightly into the lumen of the rectum; upon examination, redness and slight swelling of the hemorrhoidal nodules are visible. The muscular system is not affected.
- 2nd stage. The venous plexuses are significantly increased in size and can extend beyond the anus during defecation, but are capable of returning back on their own. Blood and mucus are released from the rectal canal after visiting the restroom.
- 3rd stage. The nodules fall out not only after defecation, but they cannot straighten on their own (see photo). Such a symptom is evidence that degenerative changes have occurred in the muscles, as a result of which they have lost their elasticity and firmness.
- 4th stage. Severe hemorrhoids in girls are characterized by the inability to reduce the prolapsed cavernous formations back into the anus due to severe degenerative changes in the muscles. In addition, the disease is accompanied by excruciating pain, massive bleeding, and thrombosis of venous vessels (see photo).
The stage of the pathological process is important for determining therapeutic tactics. In the initial stages, conservative methods of treating hemorrhoids, including the use of medications, are indicated. Severe disease requires excision of cavernous formations.
Types of disease
There are several factors that underlie the classification of hemorrhoidal disease: the clinical course of the pathological process and the location of hemorrhoids.
Based on their clinical course, there are 2 types of hemorrhoids:
- acute - the disease proceeds more vividly, characterized by sudden severe pain, cyanosis and swelling of the nodes, fever, bleeding, inflammation, and the formation of blood clots in the veins;
- chronic - this form of the disease is characterized by a wave-like course, when periods of remission and exacerbation alternate. Vivid symptoms appear during relapse of the disease.
Both forms of the pathological process require seeking medical help. It is the proctologist who, after carrying out diagnostic procedures, will explain to the patient how and how to treat the disease, which methods of therapy are most preferable in a particular case.
Based on the location of the cavernous formations, there are 3 main types of hemorrhoidal disease:
- internal hemorrhoids - enlarged venous plexuses are located in the submucosal layer of the rectal canal above the so-called serrated line. Signs of internal hemorrhoids in women include frequent bleeding and constipation;
- external hemorrhoids - inflamed cavernous formations are located under the skin below the serrated line (around the anus);
- combined hemorrhoids - as the name suggests, the affected areas are located on both sides of the dentate line. This is the most difficult form of the disease from a therapeutic point of view.
Thus, the manifestations of hemorrhoidal disease are diverse and depend on the form and type of disease, the stage of the pathological process. But the symptoms do not depend on gender. That is, the signs of pathology in women are no different from the symptoms of the same disease in men.
External and internal hemorrhoids - what's the difference?
Internal hemorrhoids differ from external hemorrhoids in location, symptoms and treatment methods. External bumps, unlike internal ones, are located under the skin around the anus. The dilated vessels of external hemorrhoids look like soft, leathery sacs filled with fluid. The internal nodes are located inside the anal canal, above the dentate line. They differ from external ones in that they are not immediately noticeable. They can be detected at stages 2-3 of hemorrhoids, when they begin to fall out of the anus.
You can determine whether a particular patient has internal or external hemorrhoids using the table below.
| Property | External hemorrhoids | Internal hemorrhoids |
| Location | Outside the anus, under the skin of the perineum around the anus. | Inside the anal canal of the rectum, above the dentate line. |
| How many stages are there? | Three stages, with each subsequent stage the cones increase in size. | Stage 1 - the nodes do not fall out, at stage 2 - they fall out during tension and are immediately set, at the 3rd stage they are set only manually, at the 4th stage it is impossible to set them. |
| What does it look like from the outside | Like soft sacs around the anus, they may have a bluish tint due to thrombosis. | At stages 1-2 they are not visible. At stages 3-4 they look like grapes. When pinched - blue-red. |
| Bleeding | Rare, scarce. | Frequent, abundant. |
| Thrombosis | The main complication of the external type of disease. | It occurs less frequently than in the external form. |
| Infringement | No. | Often observed at stages 3-4 of the disease. |
| Inflammation | Infrequently. | It happens even at stage 1. |
| Pain while walking, straining, sitting | Severe itching, burning, throbbing pain. | Sensitive at stages 3-4, with fallen, pinched nodes. |
| Constipation | Sometimes. | Often. |
The signs of one form or another of the disease have a clear difference. Symptoms of the disease appear brightly and strongly at the acute stage of development; they are smoothed out, sometimes latent in nature during the chronic course.
Methods for diagnosing the disease
Who diagnoses and treats hemorrhoids in women? These activities are within the competence of the proctologist. It should be understood that an experienced specialist will carry out a number of mandatory diagnostic procedures before prescribing the necessary medications.
- Visual inspection. An experienced specialist is able to determine the external form of the disease after a visual examination of the anorectal area. In this case, swollen, reddened hemorrhoids are visible, sometimes covered with cracks and ulcers.
- Palpation. This method is quite informative, since digital examination allows one to establish the preliminary location of hemorrhoids, determine their swelling and inflammation, and the severity of pain.
- Anoscopy. What is an anoscopic examination method? This is the study of the rectal canal at a distance of 12 cm from the rectal opening. The procedure is carried out using a special endoscopic device - an anoscope.
- Rectoscopy. This is another instrumental way to study the rectal canal. Using a rectoscope - a tube equipped with a lighting and optical system - a proctologist can examine almost the entire large intestine and confirm or refute the diagnosis of hemorrhoids.
- Irrigoscopy. This procedure involves an x-ray examination of the large intestine. A barium mixture, which is a contrast agent, is injected into the anus, after which several x-rays are taken. This method allows you to detect not only hemorrhoids, but also diverticulosis, polyposis, various neoplasms, etc.
For hemorrhoids, in addition to instrumental and radiological diagnostic methods, laboratory research procedures are also prescribed. A complete blood count is a mandatory test for women with hemorrhoidal disease, as it can detect anemia resulting from prolonged or frequent bleeding.
Characteristics of pain of different localization
The main source of pain for hemorrhoids in women
Most often, pain occurs in the anus. But it also happens that there are unpleasant sensations accompanied by pain in the groin. This is typical during exacerbation of the disease. Then it hurts a person to even sit and go to the toilet. It seems that the unpleasant sensations are spreading throughout the entire butt. As a result, even a minute of sitting turns into torture. It happens that with hemorrhoids, the lower abdomen and lower back, back and tailbone hurt.
Stomach ache
Mostly women note that with hemorrhoids, the lower abdomen hurts. This is typical for the second stage of the disease. The reason here is that the intestines are not completely emptied, stool accumulates, and constipation occurs.
The intensity and frequency of pain is directly related to the emotional state of the woman, as well as to the health of the body as a whole.
Pain occurs in the lower or left side of the abdomen. In addition to pain, a woman is worried about symptoms such as heaviness and bloating. If these signs of the disease occur very often, an urgent examination by a proctologist is necessary.
Lower back pain
Many women are concerned about the question: “Can my lower back hurt due to hemorrhoids?” Professionals answer this question positively. After all, a huge number of nerve endings are concentrated in the rectum and anus. If the disease is already advanced, then lower back pain with hemorrhoids intensifies.
The cause of such pain is pinching of one of the nodes.
The patient simply cannot find a place for himself. It hurts him to sit, stand and move. The lower back hurts to such an extent that you have to think about what drug to take to relieve the discomfort.
Back pain
The occurrence of back pain is mainly associated with diseases of the spine. But in some cases, a person still understands that his back hurts due to hemorrhoids. Such unpleasant sensations can appear in women with internal lumps, but external lumps do not cause such symptoms.
Acute pain accompanies exacerbation of the disease.
This mainly occurs in a supine position. Sometimes it is enough to change your position. Then the pain subsides or goes away completely. Sometimes women have a question: “Can hemorrhoids radiate to the lower back?” With acute, persistent pain, some women experience exactly this feeling. Therefore, to relieve such symptoms, you need to take painkillers.
Pain in the tailbone
Sometimes the pain is so intense that this unpleasant sensation spreads throughout the body. Therefore, patients often complain of severe pain in the tailbone.
In exceptional cases, the cause of such pain may be a complicated form of hemorrhoids, fistulas or paraproctitis.
In all other situations, the woman should turn to other specialists - a neurologist or traumatologist, depending on what caused the pain.
Degree of pain
The nature and degree of pain is different for all women. It depends on how long ago the hemorrhoids appeared, its stage and type. If the pain begins during or after bowel movements, the cause is constipation. When the stool normalizes, the pain goes away.
Acute and unbearable pain appears in the event of pinching of internal hemorrhoids and thrombosis of external cones.
Particularly unpleasant is the exacerbation of pain with anal fissures. They are injured by feces and bleed. An infection gets into them, causing inflammation. Constipation contributes to the appearance of cracks. How hemorrhoids hurt when cracked can only be compared to the pain syndrome in which an instrument is inserted into an open wound. The pain of hemorrhoids may either subside or recur. Without complete treatment of hemorrhoids, the pain will not go away on its own.
Treatment of hemorrhoids in women
The question of how to treat hemorrhoids in women is again decided by the proctologist, taking into account the severity of the symptoms and the form of the disease. There are conservative and surgical methods for treating varicose hemorrhoidal veins. Let's look at them in a little more detail.
Drug therapy
The first and second stages of the pathological process are usually treated with medications that have local and general effects on the body. At the same time, local preparations (ointments, suppositories and gels) can quickly relieve acute symptoms.
The popular and most effective local antihemorrhoidal medications act comprehensively: that is, they destroy pathogenic bacteria, stop bleeding (or prevent the formation of blood clots), and relieve swelling and inflammation.
The most popular among patients and specialists are the following ointments, many of which can be used externally or rectally:
- heparin ointment;
- Hepatrombin G;
- Troxevasin gel;
- Posterisan;
- Proctosan;
- Relief, Relief Advance;
- Aurobin;
- Bezornil;
- Levomekol;
- Procto-Glyvenol;
- Proctosedyl, etc.
Treatment of inflamed internal hemorrhoids in women involves the use of rectal suppositories with anti-inflammatory, anesthetic and wound-healing effects. The most common candles include the following:
- Relief, Relief Advance, Relief Ultra;
- Hepatrombin G;
- Posterisan;
- Proctosan;
- Ultraproct;
- Procto-Glyvenol;
- Natalsid;
- Anestezol;
- Neo-Anuzol;
- Proctosedyl M, etc.
To act directly on the source of the disease, women are prescribed systemic venotonic drugs. They are able to increase venous tone, elasticity, and reduce the permeability of vascular walls. All this prevents further expansion of hemorrhoids.
The following venotonics are suitable for oral administration:
- Detralex;
- Phlebodia 600;
- Venarus;
- Aescusan;
- Troxevasin;
- Ginkor Fort, etc.
Which drug will be effective in a particular case must be determined by the attending physician. The question of how to treat hemorrhoids in women (as well as in men) is best addressed to a specialist. Independent selection of medications is fraught with complications, undesirable consequences and worsening of the condition.
Minimally invasive and radical treatment methods
If drug treatment is ineffective, there are complications or the disease is advanced, the doctor may prescribe surgical treatment, which can be minimally invasive (less traumatic) or radical.
Today, specialists and patients increasingly prefer minimally invasive techniques, since they do not require long-term rehabilitation and are better tolerated by the human body due to the abandonment of general anesthesia.
- Sclerosis of blood vessels. The surgeon injects special drugs into the venous plexuses, which lead to flattening and gluing of the vessels. As a result, hemorrhoids die off.
- Ligation with latex rings. The use of a ligature, which is placed on the base of the cavernous formation, helps to cure hemorrhoids. Due to the lack of blood supply, the nodule soon dies.
- Laser coagulation. The venous plexuses are coagulated with narrowly targeted radiation, as a result of which their blood supply is disrupted. The vessels become empty and collapse. The method is painless and highly effective.
- Infrared coagulation. With the help of radiation, the tissue at the base of the hemorrhoid coagulates, it stops receiving recharge in the form of arterial blood and gradually dies. The method is most effective in the initial stages.
- Cryotherapy. In this case, hemorrhoids are treated using ultra-low temperatures. With such an effect, pathological formations freeze, die and come out naturally. The method is most effective in the initial stages.
The last stages of anorectal varicose veins and the presence of complications are a direct indication for hemorrhoidectomy. This procedure has a more serious effect on the body, the use of anesthesia and a long recovery period. But it is characterized by very high efficiency.
Folk remedies for hemorrhoids in women
The presence of hemorrhoids in women implies treatment with alternative medicine recipes. But it is important to remember that they are permissible in the early stages of the disease and only as an additional method of therapeutic intervention.
Typically, to treat hemorrhoidal disease at home, sitz baths, microenemas and compresses with infusions of medicinal plants, suppositories made from potato or carrot pulp, ointments based on honey, birch tar, beeswax or propolis are used.
- Sitz baths. Pre-prepare decoctions or infusions from oak bark, chamomile inflorescences, marigolds, nettle leaves or burdock root. Then the healing potion is poured into a basin, into which the woman sits. In addition to herbal ingredients, you can use a weak solution of potassium permanganate.
- Ice suppositories. If the hemorrhoid hurts or bleeds, you can make candles from water or herbal decoctions, and the liquid must first be kept in the freezer. Just do not keep the suppositories in the anus for too long, otherwise the risk of hypothermia will increase.
- Potato or carrot candles. A “torpedo” of the appropriate size is cut out of the pulp of the raw root vegetable. Before administration, the homemade preparation can be additionally lubricated with honey, olive or sea buckthorn oil. This will enhance the effectiveness of the suppository.
- Microclysters. To carry them out, take the same decoction as for sitz baths, or sea buckthorn oil or honey diluted in water. The volume of healing liquid is usually 50-70 milliliters. The procedure is suitable for the treatment of rectal hemorrhoids.
- Ointment. This is a popular folk remedy for external hemorrhoids. To make the drug, you can mix 20 grams of beeswax and 200 milliliters of vegetable (olive) oil. The composition is placed in a water bath and then poured into jars.
Traditional methods of treatment cannot act as monotherapy. What is the danger of selecting prescriptions without taking into account the opinion of the treating doctor? First of all, such drugs are characterized by low efficiency and the presence of contraindications. In addition, preference for traditional recipes can lead to aggravation of negative symptoms.
Prevention
Preventive measures are a good opportunity to protect yourself from the occurrence of a pathological process or prevent the exacerbation of a chronic disease. Moreover, the factors that provoke hemorrhoids can be more or less successfully excluded from your own life.
To prevent the appearance of anorectal varicose veins, experts advise adhering to certain rules and principles. Let's take a closer look at them.
- Diet correction. Doctors recommend avoiding salty, smoked and fatty foods. Priority is given to foods that prevent the development of constipation: fermented milk dishes, fruits and vegetables, cereals, whole grain bread. It is better to eat fractionally – 5-6 times a day.
- Refusal to lift heavy objects. If possible, avoid lifting or carrying heavy objects. Strength sports involving increased physical activity are also not recommended.
- Rejection of bad habits. Alcoholic drinks and smoking irritate the rectal mucosa and increase blood flow to the pelvis. Strong coffee and tea drinks have the same effect.
- Going to the toilet correctly. When defecating, you should not strain too hard or sit in the toilet for a long period of time. This is known to increase the pressure inside the peritoneum.
- Prevention of constipation. Improving the functioning of the digestive tract is achieved by optimizing nutrition, intestinal microflora and taking laxatives. The latter method is not preferable because laxatives cannot be used for too long.
- Increased activity. Doctors recommend moving as much as possible, walking, and swimming. Office workers are advised to periodically take a short break and do physical exercise. However, it is important to remember that you should not exceed the permissible load.
- Pregnancy tracking. Expectant and nursing mothers should monitor their health even more closely, following all the rules described above. In addition, the doctor may recommend special exercises to strengthen the muscles in the pelvic area.
The doctor’s task is to help the patient treat the disease. However, the patient himself should be more attentive to his own health, including by implementing the preventive measures listed above.
EXTERNAL HEMORRHOIDS: SYMPTOMS AND FEATURES
Most proctologists conventionally believe that external hemorrhoids are “better” diagnosed, because many of its symptoms are detected without special diagnostic procedures, including by the patient himself. However, the external form of hemorrhoids, like the internal one, is also very dangerous. If the disease is ignored, very serious consequences are possible, with node thrombosis, acute pain, and tissue necrosis. In order not to lead the situation to the need for urgent hospitalization with serious surgical interventions, you should immediately consult a doctor if you notice the following symptoms:
- Pain, itching, burning in the anal area;
- Detection of a hemorrhoidal node when washing;
- Pain when walking and sitting;
- Bleeding from the anus;
- Painful bowel movement.
Don't ignore symptoms, don't hesitate to visit your doctor, and don't rely on self-medication. You can forget about hemorrhoids for a long time if you receive timely and adequate treatment, but this is definitely not a disease that goes away on its own.