What is ulcerative colitis?
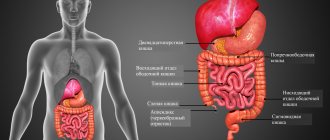
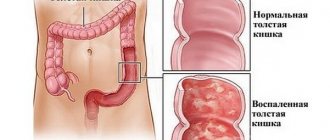
Nonspecific ulcerative colitis is a disease of the gastrointestinal tract, namely the large intestine, characterized by an inflammatory process of its mucous membrane.
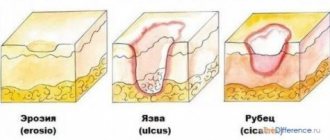
As a result of this inflammation, ulcers and areas of necrosis form in areas of the intestine. The disease is chronic and tends to recur.
Most often, the pathology affects the young population, people aged 15 to 30 years. Less commonly, the first attacks of the disease develop after 50 years. Statistics indicate that out of 100 thousand people, on average, 70 people fall ill. In addition, women are more often diagnosed than men.
The pathological process does not involve the small intestine and affects only certain areas of the large intestine, and not its entire surface. The disease manifests itself either in the rectum or in the sigmoid colon, that is, at the end of the large intestine. Then the inflammatory process further spreads.
Can ulcerative colitis be cured?
Every person who has been diagnosed with this question wonders whether it is possible to cure ulcerative colitis. Those diseases that are classified as chronic cannot be completely cured. Ulcerative colitis is one of these diseases. But this does not mean that you should completely abandon therapeutic effects.
The disease can and should be controlled by choosing the optimal tactics of influence together with the attending physician. This must be done, since the pathology is characterized by cyclicality, that is, periods of remission are replaced by periods of exacerbation. If you ignore the presence of colitis for a long time, this threatens the development of complications, including death. Therapy and diet help control the disease, preventing repeated attacks. Therefore, with proper treatment, the quality and life expectancy of a person with ulcerative colitis is not affected. Stable remission can be observed for years.
general description
Ulcerative colitis or nonspecific ulcerative colitis is a chronic inflammatory disease of the mucous membrane of the large intestine, resulting from an imbalance of the immune system (antibodies are released to the own epithelium of the mucous membrane).
Cases of morbidity are registered in 0.3-0.5% of people, which is approximately 3-5 cases per 100 thousand population. The disease occurs in both men and women.
Ulcerative colitis can affect people of any age, most often occurring in the 25-35 and 60-80 age groups.
Symptoms of nonspecific ulcerative colitis
The symptoms of the disease depend on where exactly the pathological process is localized and on its intensity. In addition, it is worth distinguishing between intestinal and extraintestinal manifestations.
Intestinal symptoms include:
- The appearance of diarrhea, in which blood impurities are found. Often, in addition to bloody clots, mucus and pus are present in the stool, which gives them a fetid odor. It happens that blood with mucus and pus appears in between bowel movements. The frequency of stool varies depending on the severity of the disease and can reach up to 20 times per day. A person can lose up to 300 ml of blood per day. With a milder course of the disease, a person defecates several times, more often in the morning and at night.
- Pain symptoms also vary in severity. They can be either sharp, causing severe discomfort, or weak, not causing serious suffering to a person. Sometimes it is not possible to get rid of painful sensations even with the help of medications, which indicates the development of complications of the disease. The location of the pain is the left side of the abdomen or the left iliac region. As a rule, increased pain occurs before the act of defecation, and after it they subside somewhat. Also, the pain may increase in severity after eating.
- An increase in body temperature, but, as a rule, insignificant, up to subfebrile levels.
- General intoxication of the body with accompanying symptoms, including the appearance of weakness, dizziness, the development of depression, decreased mood, the occurrence of irritability and tearfulness. The patient's appetite decreases, and therefore he begins to lose weight, which in some cases leads to anorexia. Intoxication is typical if the disease is severe.
- Tenesmus or false urge to have a bowel movement. In some cases, instead of feces, either mucus or mucopurulent masses are released.
- Severe flatulence.
- Fecal incontinence.
- Change from diarrhea to constipation. Such a transition is a sign that severe inflammation has begun to develop in the mucous membrane lining the colon.
- Sometimes ulcerative colitis can develop rapidly. This form of the disease is called fulminant and will be discussed below.
In addition to intestinal symptoms, the patient suffers from extraintestinal lesions:
- Development of erythema nodosum (formation of subcutaneous nodules detected by palpation), gangrenous pyoderma (necrosis of a skin area). This is due to increased circulation in the blood of bacteria and immune complexes produced to fight them. In addition, skin lesions such as focal dermatitis, urticarial and postulous rashes were also noticed.
- Damage to the oropharynx, which occurs in 10% of patients. This is expressed in the spread of aphthae, which disappear after remission is achieved. Glossitis, gingivitis, and ulcerative stomatitis may also begin to develop in the oral cavity.
- Eye diseases are observed even less frequently, in no more than 8% of patients. Patients may suffer from iridocyclitis, uevitis, choroiditis, conjunctivitis, keratitis, retobulbar neuritis and panophthalmitis.
- Joint lesions, which are expressed in arthritis, spondylitis, sacroiliitis. Moreover, such lesions of articular tissue are often precursors to ulcerative colitis.
- More often than other systems, the lungs are exposed to pathological processes.
- As a result of malfunctions of the endocrine gland, malfunctions occur in the liver, biliary tract, and pancreas.
- It is extremely rare for patients to complain of myositis, osteomalacia, osteoporosis, vasculitis, and glomerulonephritis.
- Cases of the development of autoimmune thyroiditis and hemolytic anemia have been described.
The first signs of nonspecific ulcerative colitis
In order not to confuse the onset of the disease with other similar pathologies of the intestinal tract, you need to have an idea of what the first signs of colitis may be.
There are several options for the development of the disease:
- Firstly, diarrhea may initially develop, and after a few days blood and mucous masses are found in the stool.
- Secondly, rectal bleeding may occur immediately after the manifestation of the inflammatory process. In this case, the stool will not be liquid, but formed or have a porridge-like consistency.
- Thirdly, the patient may suffer from diarrhea, intoxication and rectal bleeding at the same time.
Most often, the disease begins to develop gradually, with diarrhea, which is caused by the development of extensive inflammation in the intestinal mucosa. Against the background of this process, it becomes unable to reabsorb sodium and water. Blood, in turn, appears due to the fact that ulcers form on the membrane, forming loose connective tissue penetrated by a vascular network. Symptoms tend to decrease and then gain momentum again.
In addition to diarrhea, the first signs of the onset of the disease may be pain occurring mainly on the left side and a slight increase in body temperature. A person may experience pain in the joints, since in some cases, damage to their tissues precedes the development of the disease.
So, four early signs that you should pay attention to, and which allow a person to independently suspect ulcerative colitis, are: bloody diarrhea, joint pain, abdominal discomfort and fever.
Nonspecific ulcerative colitis - symptoms and treatment
Tactics depend on the location of the lesion and the severity of the course. In distal forms of the disease, the course is usually mild, so patients can be treated on an outpatient basis. Total or left-sided lesions often have a severe course and therefore require hospitalization and treatment in a hospital setting.
Diet
Diets No. 4, 4B, 4B according to Pevzner are prescribed. The purpose of the diet is to reduce inflammation, fermentation and putrefactive processes in the intestines, and normalize the functions of the intestines and other digestive organs. Dishes are liquid, semi-liquid, pureed, boiled in water or steamed. Very hot and cold dishes are excluded.
Products allowed for ulcerative colitis:
- crackers, soups with a slimy consistency, cooked in low-fat meat, fish broth or vegetable broth, with well-cooked cereals, noodles or noodles, the addition of meatballs is allowed;
- lean meat and fish;
- thoroughly cooked porridge;
- fruit purees;
- fresh grated cottage cheese;
- sugar in small doses;
- jelly and jelly from blueberries, dogwoods, bird cherry, quince, pears;
- strong black tea, maybe with lemon, a decoction of rose hips, black currants, blueberries and bird cherry;
- steam omelette, hard-boiled eggs; butter.
Products prohibited for ulcerative colitis:
- baked goods and confectionery products;
- black bread;
- meat and fish fatty broths;
- sausages, salted and smoked fish, canned food;
- alcohol;
- coffee;
- milk;
- carbonated sweet drinks;
- fresh vegetables and fruits;
- pearl barley and wheat porridge, legumes.
Conservative therapy
Conservative therapy includes:
- aminosalicylates, 5-aminosalicylic acid preparations (5-ASA, mesalazine);
- corticosteroids;
- immunosuppressants;
- biological therapy.
Aminosalicylates are first-line drugs and are used first. To stop an attack of ulcerative colitis, 3-6 weeks of therapy at 1-2 g/kg per day are usually required. After this, anti-relapse treatment is carried out with sulfasalazine (3 g/day) or mesalazine (2 g/day).
For distal lesions (proctitis), preference is given to the forms of the drug in the form of suppositories . For left-sided lesions - drugs in the form of foam for rectal use. In case of total damage, tablet forms of drugs are used.
When treated with these drugs, remission is achieved in 74-81% of cases.
The most pronounced and effective anti-inflammatory agent are glucocorticoids .
The main indications for treatment with glucocorticoids are:
- acute course of severe and moderate severity;
- severe or moderate left-sided and total lesion in the presence of III degree of inflammation according to endoscopic examination;
- ineffectiveness or lack of effectiveness of treatment with aminosalicylates in chronic disease.
In acute severe cases, intravenous administration of glucocorticoids (prednisolone at least 120 mg/day) is prescribed 4-6 times a day. Correction of water and electrolyte balance, transfusion of blood components, and hemosorption are required. A week after intravenous administration, they switch to taking prednisolone orally. During this time, gastroscopy is performed to exclude peptic ulcers of the stomach and duodenum.
For moderate forms, you can limit yourself to oral prednisolone. Typically, prednisolone is prescribed at a dose of 1.5-2 mg/kg body weight per day. The maximum dose is 100 mg (in elderly people 60 mg).
If there are no side effects, then continue taking it for another 10-14 days, then reduce the dose by 10 mg every 10 days. From 30-40 mg they switch to a single dose of prednisolone. From 30 mg, the dose is reduced by 5 mg per week. Typically, the course of hormone therapy lasts from 8 to 12 weeks. In parallel with hormone therapy, aminosalicylates are used until hormones are completely withdrawn.
For proctitis, glucocorticoids are used rectally in microenemas. Usually hydrocortisone is used for this, applied after bowel movements 2 times a day.
Side effects of hormone therapy:
- swelling;
- arterial hypertension;
- osteoporosis;
- various autonomic disorders;
- may contribute to the development of stomach ulcers, and, as a result, gastrointestinal bleeding may occur.
The modern glucocorticoid is budenofalk (containing budesonide). The daily dose is 3 mg budesonide (1 capsule) 4-6 times a day.
When treated with glucocorticoids, hormonal dependence or even hormone resistance may occur, which develops in 20-35% of patients with severe ulcerative colitis. Hormonal dependence is the body’s response to glucocorticoid treatment, in which the inflammatory process resumes after the dosage is reduced.
If there is no effect from hormonal therapy, drugs that have an immunosuppressive effect, as well as biological therapy, are prescribed. The main ones are 6-mercaptopurine and azathioprine - these are first-line drugs. They help reduce the dose of hormones and cancel them in 62-71% of cases. Treatment is usually started along with hormone therapy. The maximum daily dose is 150 mg. A small number of side effects, compared to glucocorticoids, allows the drug to be used for many years.
There is also a similar drug - methotrexate, which is used for intolerance to azathioprine or to accelerate the therapeutic effect. Orally or intramuscularly 30 mg per week. The effect occurs within 2-4 weeks
If there is no effect from azathioprine and 6-mercaptopurine, second-line drugs are used - these are infliximab and cyclosporine A.
If there is no effect from the second injection of infliximab and a 7-day course of cyclosporine A, surgical treatment is indicated.
Anti-relapse treatment
After relief of acute inflammatory processes, anti-relapse therapy with aminosalicylates is prescribed for up to 6 months. If treatment is successful and there are no clinical and endoscopic signs of the disease, therapy is discontinued.
In case of unstable effect from anti-relapse treatment, therapy is extended for an additional 6 months.
If aminosalicylate monotherapy is ineffective, immunosuppressants (azathioprine or 6-mercaptopurine) and hormones are added to treatment.
Patients with ulcerative colitis receiving conservative therapy require constant medical supervision and regular endoscopic examination with biopsy.
Surgery
According to statistics, surgical treatment is indicated for patients in 11-22% of cases. The only method of radical surgical treatment of ulcerative colitis is colproctectomy, that is, removal of the entire colon. The main indications for surgical treatment are:
- lack of effect from conservative treatment;
- development of complications of ulcerative colitis (bleeding, perforation, cancer, toxic dilatation of the large intestine).
Postoperative complications
Occurs in weakened patients against a background of severe disease:
- eventration (intestinal prolapse through a defect in the abdominal wall);
- failure of intestinal stoma sutures;
- serous peritonitis (inflammation of the peritoneum);
- polyserositis;
- abdominal abscesses;
- pneumonia.
Features of treatment depending on the form and course
Left-sided colitis or proctitis of low activity: suppositories and salofalk foam.
Moderate or widespread colitis: salofalk tablets, glucocorticoids.
Severe course: salofalk tablets, glucocorticoids, infusion therapy, iron supplements, transfusion of plasma and red blood cells, colproctectomy (removal of the entire colon with the formation of a permanent ileostomy - an opening in the abdominal cavity to which a colostomy bag is attached).
Fulminant colitis: treatment is the same as for severe colitis.
Causes of ulcerative colitis
The question of the etiology of the disease still remains open and scientists are still searching for the reasons that cause its development.
However, risk factors that have a provoking effect on the development of the pathological process in the large intestine are reliably known:
- Genetic predisposition. The risk of a close blood relative suffering from the disease increases significantly if there is a family history of similar cases of ulcerative colitis.
- Infectious nature of the disease. The intestine is a part of the body where a huge number of bacteria are concentrated. Some of them at a certain point in time can lead to the development of inflammation.
- Autoimmune mechanisms occurring in the body. This idea was prompted to scientists by the fact that ulcerative colitis is associated with seasonal exacerbations and responds well to treatment with hormonal drugs. Studies have confirmed that the more severe the process occurring in the intestines, the more aggravated the changes in immune status are.
- Violation of the diet, errors in the menu.
- Stress and other traumatic factors.
Scientists come to the conclusion that this disease depends on many factors, each of which has a specific impact on the formation of ulcerative colitis. However, the leading role most likely belongs to intestinal antigens. As proof of this theory, one can cite a large study conducted by American scientists, the results of which were published in the Los Angeles Times. Scientists were able to experimentally establish a connection between fungi found in the intestines and ulcerative colitis.
Thus, at present, in the theory of disease pathogenesis, the leading role is assigned to two factors: immune and genetically determined.
Causes of ulcerative colitis
Until now, the exact cause of ulcerative colitis is unknown.
Several reasons are considered in the scientific literature, but they are not fully understood:
- Genetic predisposition: close relatives have diseases such as Crohn's disease or ulcerative colitis
- Bacterial and viral infections
- Environmental factors (smoking, adherence to diets, long-term use of oral contraceptives)
Forms of ulcerative colitis
It is customary to distinguish several forms of the disease, which depend on the location and degree of localization of the inflammatory process in the colon, as well as on the nature and intensity of the disease.
So, depending on the location of inflammation, they distinguish:
- Left-sided colitis. This form differs in that the colon is affected. Symptoms begin with diarrhea, which contains blood. The pain is localized on the left side, appetite disappears, which leads to dystrophy.
- Total colitis. This form of the disease is considered the most life-threatening, as it threatens the development of complications, in particular, dehydration, drop in blood pressure, and hemorrhagic shock. Symptoms of such colitis manifest themselves in the form of high-intensity pain, persistent profuse diarrhea, and massive blood loss.
- Pancolitis, characterized by inflammation of the rectum along its entire length.
- Distal colitis. This form of colitis is characterized by the inclusion in the pathological process of the lining of the left intestine, that is, the sigmoid and rectum at the same time. It is distal colitis that is widespread. Symptoms manifest themselves in sharp pain, mainly localized in the left iliac region, tenesmus, secretion of mucus and streaks of blood in the stool, flatulence and, sometimes, constipation.
- Proctitis, in which only the rectum is affected.
Depending on the characteristics of the disease, the following are distinguished:
- Chronic continuous colitis.
- Fulminant or acute colitis.
- Chronic relapsing colitis.
Chronic ulcerative colitis
Chronic ulcerative colitis is characterized by the fact that the intestinal lining is hyperemic, the vascular pattern undergoes a change, and erosions and atrophic formations are found along its line.
The main symptom of chronic ulcerative colitis is a long-term disorder of stool, which during the period of exacerbation becomes more frequent up to 15 times a day. Also, diarrhea gives way to constipation.
In addition, a constant companion of chronic colitis is abdominal pain, which is aching and monotonous. During periods of remission, patients complain of increased gas formation and rumbling in the stomach. However, no weight loss is observed, and appetite, as a rule, is not impaired.
Often such people have neurological disorders, in particular, fatigue, irritability, and hyperhidrosis. The abdomen is swollen, and upon palpation, moderate pain in individual segments of the colon is noted.
Exacerbation of ulcerative colitis
An exacerbation of the disease is characterized by a rapid manifestation of all symptoms. The stool becomes more frequent and contains blood and mucus. Electrolyte disturbances quickly increase, and if left untreated, dehydration develops.
It is dangerous to ignore an acute ulcerative process in the colon, as it threatens complications. Among them are the development of arrhythmia (due to a lack of magnesium and potassium), swelling (due to a drop in oncotic pressure of the blood against the background of a decrease in proteins in the blood), hypotension, dizziness, decreased vision, and intoxication of the body.
In addition, the fulminant or fulminant form of colitis is especially dangerous, which can even lead to rupture of the colon and internal bleeding.
Tablets for ulcerative colitis
Ulcerative colitis
This is a chronic inflammation of the large intestine. A typical symptom is diarrhea mixed with blood and mucus. In addition, pain appears, often in the epigastric region on the left. In most cases, ulcerative colitis occurs in the form of attacks (exacerbations): during the absence of symptoms, the patient can lead a normal daily life. During an exacerbation, on the contrary, hospitalization may be necessary. Here you can read information about how you can help yourself with ulcerative colitis, how nutrition affects the disease and how inflammation of the large intestine actually occurs.
Spread of ulcerative colitis
Ulcerative colitis always begins in the rectum. From there it can always spread to a greater or lesser extent into the colon.
However, in many patients the inflammation is limited to the rectal area. In this case, doctors talk about proctitis. If the inflammation additionally spreads to the left side of the colon, left-sided colitis occurs. In some patients, the inflammation spreads even further into the large intestine. If the entire large intestine (along with the rectum) is eventually affected, then it is referred to as pancolitis.
As colitis spreads, the severity of symptoms also increases.
Ulcerative colitis: different types of disease course
In more than 80 percent of patients, ulcerative colitis occurs in the form of periodic exacerbations: phases of more or less pronounced symptoms (exacerbations) are replaced by phases without inflammation and complaints. In this case, doctors talk about a chronically relapsing course.
In approximately ten percent of patients, the disease has a chronically constant course. In this form, symptoms do not go away completely after an exacerbation.
Diagnosis of ulcerative colitis
If a person suspects that he is developing ulcerative colitis, he should seek medical help. The disease can be diagnosed by either a therapist or a gastroenterologist.
To make an accurate diagnosis, laboratory tests will be required, including:
- General blood analysis. Based on its results, anemia and an increase in the number of leukocytes are diagnosed.
- A biochemical blood test will show an increase in C - reactive protein, indicating the presence of an inflammatory process. The number of gamma globulins will increase, the quantitative content of magnesium, calcium and albumin will decrease.
- An immunological blood test that will detect the growth of antibodies (cytoplasmic antineutrophil).
- Stool analysis, which will contain blood, mucus and pus.
Endoscopy, which includes colonoscopy and rectosigmoidoscopy, will indicate the presence of:
- Purulent, mucous and bloody discharge in the intestinal lumen;
- Swelling;
- Hyperemia;
- Pseudopolyps;
- Bleeding.
When endoscopy is performed during remission of the disease, atrophy of the mucous membrane lining the intestines is observed.
We must not forget about x-ray examination. For this disease, a barium mixture is used to create contrast. According to the results of the x-ray, the patient can see polyps, ulcerations, and a decrease in the length of the intestine, if any.
Scientists are developing a new type of examination - capsule endoscopy, which in some cases can replace colonoscopy. This procedure is painless and does not cause discomfort, however, visualization with it is worse than with direct examination of the intestine.
Consequences of ulcerative colitis
The consequences of ulcerative colitis that was diagnosed late can be quite serious:
- If the entire colon is affected, there is a risk of developing colorectal cancer over the next few years.
- There is also a risk of colon perforation, which can be fatal.
- The disease often causes cracks to form in the intestines and intestinal bleeding to develop.
- Toxic megacolon is another complication of the disease, which consists in the expansion of the intestine in the affected colitis area. The process is accompanied by severe pain, high fever and general weakness.
Symptoms of the disease
Nonspecific ulcerative colitis can occur in different ways, depending on the prevalence and severity of the lesion. Some patients may not have symptoms for a long time (months or even years).
Most often, the disease manifests itself in the form of abdominal pain, diarrhea (usually at night and in the morning, up to 20 times a day, and in severe cases - up to 40 times), impurities of blood, pus and mucus in the stool. If the entire large intestine is involved in the pathological process, in addition to the described symptoms, weakness and weight loss occur. With each new exacerbation, weight loss increases more and more.
The most severe form of ulcerative colitis is fulminant. Severe abdominal pain, severe weakness, severe diarrhea and vomiting occur, which can lead to dehydration. Body temperature rises.
Get a treatment program
Treatment of ulcerative colitis of the intestine
Treatment of the disease is carried out symptomatically, since there is no possibility of medicinal treatment of the cause of inflammation. Therefore, the goals that doctors strive to achieve boil down to relieving inflammation, preventing serious complications and establishing a state of stable remission.
Conservative treatment of the disease consists of:
- In following a diet. When the disease is in the acute phase, the patient is completely limited in food, and only water is offered as a source of drink. When the acute phase ends, the patient needs to switch to a protein diet, low in fat. The priority will be eggs, cottage cheese, lean meat and lean fish. Coarse fiber is also not suitable for consumption, as it can injure the irritated intestinal mucosa. The source of carbohydrates should be sought in a variety of cereals, berry-based compotes, etc. In particularly difficult cases, the patient is transferred to artificial nutrition.
- Since refusal of fresh fruits and vegetables threatens vitamin deficiency, the patient is recommended to take vitamin and mineral complexes.
- Taking non-steroidal anti-inflammatory drugs, including mesalazine, sulfasalazine, salofalk.
- Corticosteroid hormonal drugs are prescribed, but with extreme caution. This is due to the fact that they can cause some serious complications, in particular osteoporosis and hypertension. These are drugs such as prednisolone, methylprednisolone.
- Therapy with antibacterial agents: Cifran, ciprofoxalin, ceftriaxocone.
- Symptomatic drugs necessary for pain relief, stopping diarrhea, increasing iron levels in the blood if there is anemia.
- There are physiotherapeutic methods of influencing the disease. Among them, the following have shown particular effectiveness: SMT (modulated current exposure), diadynamic therapy, interference therapy and others.
When conservative methods do not provide the desired effect in fighting the disease, doctors resort to surgery.
Indications for surgery for ulcerative colitis are:
- perforation (perforation of the intestinal wall)
- signs of intestinal obstruction
- abscess
- presence of toxic megacolon
- profuse bleeding
- fistulas
- bowel cancer
The following modern surgical techniques are used:
- Proctocolectomy with either a temporary or permanent ileostomy to remove human waste products.
- Colectomy (excision of the colon)
- Proctocolectomy (removal of the rectum and colon) with preservation of the anus
As for the prognosis, in the case of uncomplicated colitis it is favorable. The majority of patients (almost 80%) who begin treatment in a timely manner do not experience attacks of exacerbation of the disease throughout the year. Relapses occur on average once every five years, but in rare cases (about 4%), this period can last up to 15 years.
Surgical intervention is required relatively infrequently, requiring it in about 20% of the total number of cases. Malignant neoplasms develop in 10% of cases. The absence of clinical manifestations does not mean that the patient is insured against cases of relapse of the disease. The prognosis is considered most unfavorable for the progressive form of the disease.
On topic: Treatment of colitis with folk remedies
Nonspecific ulcerative colitis
Since the causes of nonspecific ulcerative colitis are not fully understood, the goals of therapy for this disease are to reduce the intensity of the inflammatory process, subside clinical symptoms and prevent exacerbations and complications. With timely correct treatment and strict adherence to the recommendations of the proctologist, it is possible to achieve stable remission and improve the patient’s quality of life.
Ulcerative colitis is treated with therapeutic and surgical methods, depending on the course of the disease and the patient’s condition. One of the important elements of symptomatic treatment of nonspecific ulcerative colitis is dietary nutrition.
In severe cases of the disease at the height of clinical manifestations, the proctologist may recommend a complete refusal to eat, limiting yourself to drinking water. Most often, during an exacerbation, patients lose their appetite and tolerate the ban quite easily. If necessary, parenteral nutrition is prescribed. Sometimes patients are transferred to parenteral nutrition in order to more quickly alleviate the condition of severe colitis. Eating is resumed immediately after appetite is restored.
Diet recommendations for ulcerative colitis are aimed at stopping diarrhea and reducing irritation of the intestinal mucosa by food components. Products containing dietary fiber, fiber, spicy and sour foods, alcoholic beverages, and roughage are removed from the diet. In addition, patients suffering from chronic intestinal inflammation are recommended to increase the protein content in their diet (at the rate of 1.5-2 grams per kilogram of body per day).
Drug therapy for ulcerative colitis includes anti-inflammatory drugs, immunosuppressants (azathioprine, methotrexate, cyclosporine, mercaptopurine) and anticytokines (infliximab). In addition, symptomatic medications are prescribed: antidiarrheals, painkillers, iron supplements for signs of anemia.
Non-steroidal anti-inflammatory drugs - 5-aminosalicylic acid derivatives (sulfasalazine, mesalazine) and corticosteroid hormonal drugs are used as anti-inflammatory drugs for this pathology. Corticosteroid drugs are used during periods of severe exacerbation in cases of severe and moderate severity (or if 5-aminosalicylates are ineffective) and are not prescribed for more than a few months.
Corticosteroid hormones are prescribed to children with extreme caution. Anti-inflammatory hormone therapy can cause a number of severe side effects: arterial hypertension, glucoseemia, osteoporosis, etc. Physiotherapeutic methods of treatment for ulcerative colitis can include diadynamic therapy, SMT, interference therapy, etc.
Indications for surgical treatment are the ineffectiveness of diet and conservative therapy, the development of complications (massive bleeding, perforation of the colon, if a malignant neoplasm is suspected, etc.). Resection of the large intestine followed by the creation of an ileorectal anastomosis (connection of the free end of the ileum to the anal canal) is the most common surgical technique for treating ulcerative colitis. In some cases, a section of the affected intestine limited within healthy tissues is removed (segmental resection).
Diet and nutrition for ulcerative colitis
According to most gastroenterologists, it is impossible to create a single diet that would suit every patient without exception. Each case requires an individual approach. However, there are practical recommendations regarding what a sick person’s diet should be.
The following principles must be adhered to:
- A diet for ulcerative colitis is not able to cover all the needs of the human body for vitamins and minerals, since it is gentle and excludes many foods.
- It is important to avoid lactose-containing products. We are talking about milk and all its derivatives.
- Fats should be avoided.
- Fiber and carbohydrate foods are prohibited.
- The emphasis of the diet should be on protein foods.
Traditionally, doctors recommend that patients with inflammatory processes in the intestines follow diet number 4b.
Diet 4b
Principles of the melon diet:
- It involves avoiding fresh vegetables and fruits that contain coarse, indigestible fiber, which causes bloating and can injure the intestines. In addition, all legumes, fruit juices, corn, nuts, seeds, sorrel, rhubarb, spinach, etc. are prohibited. Cream, cheeses, sour cream, coffee, garlic, onions, and seasonings are excluded.
- However, not all fruits are prohibited. When the patient's condition has stabilized, he is allowed to eat a banana, pear or apple without peel, after heat treatment. Vegetables you can use are zucchini, pumpkin, carrots, potatoes after heat treatment and in grated form.
- You need to avoid flour products; only dried bread will do. Soups are prepared in low-fat meat or vegetable broths. Meat in second courses is twisted or ground. Desserts are mainly jellies and mousses. Jelly, compotes and decoctions of dried berries (currants, rose hips, hawthorn) are useful. It is important to eat at least five eggs a week. They are prepared soft-boiled, steamed, or in the form of omelettes.
- The dishes themselves are steamed, boiled or baked; under no circumstances should they be fried or brought to a brown crust. When it is possible to achieve stable remission, the diet can be expanded with prohibited dishes, but only after consultation with a doctor.
Menu for a week for ulcerative colitis
Recommendations for creating a menu for a sick person must be given by a doctor. During the acute phase, a person is not recommended to eat food at all. Therefore, the proposed menu is suitable for the period of remission.
Monday
- For your first breakfast, you can cook a steamed omelette and drink weak tea.
- For second breakfast, an apple baked in the oven is perfect.
- For lunch, the patient can be offered chicken breast meat broth with egg flakes. The second consists of carrot puree and steamed lean beef cutlets. Kissel is used as a dessert.
- In the afternoon you can drink cocoa with water.
- For dinner, they eat boiled pollock with mashed potatoes, rice pudding (from white rice), seasoned with pear sauce, and unsweetened tea.
- Before going to bed, you can drink jelly.
Tuesday
- The first breakfast consists of manna and unsweetened tea.
- As a second snack, you can use grated low-fat cottage cheese.
- For lunch they prepare vegetable puree soup (potatoes, carrots, zucchini) and boiled veal meatballs.
- The afternoon snack consists of quince decoction and crackers.
- For dinner they prepare pike perch cutlets with buckwheat porridge. Unsweetened tea is used as a drink.
- The evening ends with blueberry jelly.
Wednesday
- You can start the day with oatmeal in water and a little butter. The drink used is unsweetened herbal tea.
- For second breakfast, you can eat a soft-boiled egg.
- For lunch, the patient eats a serving of rice soup with pike meatballs. For the second course, you can prepare mashed potatoes and steamed chicken cutlets. A rosehip decoction is suitable as a drink.
- The afternoon snack consists of grated cottage cheese with a small amount of sugar.
- Steamed fish dumplings and buckwheat porridge are prepared for dinner.
- The day ends with jelly and crackers.
Thursday
- The morning begins with poached eggs and semolina porridge. The drink is unsweetened cocoa with water.
- The second breakfast consists of pear jelly.
- For lunch they prepare a decoction of vegetables with river fish meatballs, veal soufflé and buckwheat pudding. You can wash down your meal with a decoction of bird cherry.
- As a snack before dinner, you can use crackers and rosehip decoction.
- For dinner, prepare rabbit quenelles with boiled rice.
- Before going to bed, you can drink a glass of oatmeal jelly.
Friday
- The morning starts with a bunch of rice porridge and blueberry compote.
- As a snack before the main meal, eat a soft-boiled egg.
- For lunch, chicken meatballs with liquid boiled puree and pear compote.
- The afternoon snack consists of cottage cheese and apple pudding.
- For dinner, carrot puree and boiled softened pike perch with blackcurrant jelly.
Saturday
- In the morning, a slimy decoction of oatmeal with rosehip jelly is used.
- As a snack before lunch - egg porridge.
- Lunch itself consists of pureed buckwheat soup, steamed cod balls with vegetable casserole.
- At midday, the patient is offered cottage cheese pate with carrots and tea.
- For dinner, potato cutlets with boiled tongue and quince jelly.
- Before going to bed, you can eat a baked apple.