Causes
Why you feel sick with pancreatitis is explained by the physiology of the pancreas. The organ secretes pancreatic juice, a fluid containing substances for the digestion of proteins, fats and carbohydrates. These substances are called enzymes, designed to break down food into tiny particles that are absorbed by the intestinal mucosa. There are several causes of nausea due to inflammation of the pancreas in women and men.
- Nausea with pancreatitis occurs due to inflammation in the pancreas. The production of pancreatic juice is disrupted, and an insufficient amount of enzymes enters the intestines. Digestion of food does not occur completely. Most of it passes through the intestines unchanged, which causes increased contractions and nausea.
- Another cause of nausea is severe intoxication of the body. It is caused by inflammation and destruction of organ cells. Toxic substances enter the bloodstream and spread throughout the body, causing nausea and vomiting.
- Pancreatitis is often combined with inflammation of the liver or gallbladder. At the same time, bile ceases to be produced normally. This digestive liquid has bactericidal properties. With its deficiency, the cause of stomach dysfunction is microbes that begin to actively multiply.
You can get rid of nausea due to pancreatitis by determining the cause of its occurrence.
Feeling pain
A feverish feeling along with chills and general weakness are signs that may indicate a problem with the pancreas. Many, although not all, patients with pancreatitis experience an increase in their body temperature. Fever may be caused by inflammation of the pancreas or one of the ducts, or an infection in the pancreas or elsewhere in the body. Depending on the cause of the fever, antibiotics may be recommended. Most often, the fever subsides after the pancreatitis resolves.
Text continues after advertisement
What happens
Manifestations of nausea and vomiting with pancreatitis vary. It depends on the form of the disease, the severity of inflammation, and the general condition of the body.
Acute form
Pancreatic disease that occurs for the first time is the most severe. A person suddenly experiences acute pain under the left rib, which quickly spreads throughout the entire abdomen, radiating to the back, becoming encircling in nature.
Nausea accompanies the pain syndrome from the very beginning.
After a short time, vomiting appears, caused by massive inflammation of the gland and intoxication. Vomiting with pancreatitis is painful, does not bring relief, and is repeated many times. In the intervals between attacks, the nausea does not stop.
At the same time, profuse loose stools occur. All this causes dehydration and electrolyte imbalance. If the disease was caused by an infection, the presence of bacteria is detected in the vomit.
Chronic form
Develops after acute inflammation. Manifestations of the disease are less pronounced, but are observed for a long time. If a person does not follow a diet, does not take enzyme preparations, he constantly feels sick and the pancreas area hurts. Pain and nausea manifest themselves in different ways - they will be intense or subtle. Vomiting occurs extremely rarely. Unstable stool is observed - constipation alternates with diarrhea.
Chronic pancreatitis is more severe during pregnancy. The nausea becomes more intense and the pain intensifies. Vomiting may occur.
Exacerbation of the chronic form
In the chronic form, symptoms manifest themselves in the form of periods of remission and exacerbation. Exacerbations can be triggered by:
- error in diet;
- drinking large amounts of alcohol;
- heavy physical activity.
For exacerbation of pancreatitis, sudden onset and severe abdominal pain are typical. At first, a person is bothered by severe nausea, vomiting occurs 6-12 hours after the onset of symptoms. Usually it is a one-time procedure, after which the person feels a little better.
If the exacerbation was caused by alcohol abuse, tissue destruction and bleeding from the mouth are observed. Sometimes an exacerbation is caused by microbes - if they become infected and intoxication occurs, an increase in temperature is noted.
Precautionary measures
If a person is diagnosed with chronic pancreatitis, he is prescribed preventive measures and drug therapy aimed at preventing exacerbations.
A prerequisite is compliance with the diet. Its goal is to normalize pancreatic function and reduce intestinal motility. It is recommended to exclude the following types of foods from your diet:
- meat - fatty pork and lamb, game;
- fish - fatty varieties, caviar;
- dairy - sour cream, cream, fatty cheese;
- drinks - strong tea, coffee, alcohol;
- spices.
When following a diet, it is not recommended to eat vegetables and fruits raw, as fiber increases peristalsis and provokes nausea. Dishes are prepared boiled or steamed. One of the folk remedies used in the diet is oat decoction.
Enzyme preparations are used to maintain the pancreas and against nausea:
They are prescribed for a short course or long-term, depending on the stage of the disease.
What to do if the patient is sick
Antiemetic drugs are indicated for relief from pancreatitis. Traditional medicine is also used to relieve symptoms. This is prescribed by a gastroenterologist.
Treatment of pancreatitis is carried out comprehensively, taking into account the cause of its occurrence and the severity of its manifestations. The following remedies can help relieve nausea:
Factors that provoke nausea
The manifestation of nausea in the presence of pancreatitis is due to internal poisoning of the body. The following begin to be produced in excessive amounts:
- digestive enzymes;
- biologically active substances.
With excessive production of the listed components, gastrointestinal tract poisoning occurs. The violation has a detrimental effect on the excretory system and other internal organs. Some foods are difficult to digest. Such food intensifies the existing spasms. Dishes and drinks that cause nausea are listed in the table.
| Foods that cause nausea | Such food may include:
|
| Drinks that cause nausea | These drinks include:
|
All of these products have a detrimental effect on the functioning of the gastrointestinal tract and are difficult to digest. Their use does not go unnoticed. The patient's condition worsens. Additional symptoms occur, including nausea and vomiting.
Pancreatic dysfunction causes digestive problems
Doctors also consider the following to be the root causes of nausea:
- accumulation of enzymes produced in excessive amounts;
- impaired absorption of nutrients in the presence of pancreatitis and poisoning of the body with toxic components.
With pancreatitis, the situation is similar to typical poisoning. Nausea is a consequence of the inability to absorb required nutrients. The severity of the symptom directly depends on the severity of the pancreatic disease.
The nature of nausea and vomiting in pancreatitis
Nausea is one of the main symptoms of this disease. It worries 70-80% of patients in gastroenterology departments with this diagnosis. An increase in this unpleasant sensation can occur either suddenly or naturally after eating. Therefore, patients are often interested in “how to relieve nausea with pancreatitis quickly and effectively?”
All patients want to relieve an attack and relieve nausea during pancreatitis, but not many know why this unpleasant sensation occurs. Let's take a closer look at the causes of nausea:
- With pancreatitis, the exocrine functions of the pancreas are disrupted, that is, the organ does not secrete enough enzymes to break down proteins, fats and carbohydrates, or the enzymes are activated at the wrong time.
- Impaired exocrine function leads to the fact that enzymes trigger the digestion process in the organ itself, which results in inflammatory processes and attacks of nausea.
- A disrupted digestion process provokes the transformation of broken down elements, which the body tries to get rid of through vomiting. This condition is similar to a state of poisoning, only in this case the culprit is not food, but the body’s inability to digest and assimilate it.
Different people complain of different patterns of nausea episodes. For some, it brings very little anxiety, while for others it brings suffering throughout the entire treatment period. Most often, nausea with pancreatitis is characterized by the following symptoms:
- It may be permanent or occur due to any provoking factors, which is typical for the acute course of the disease.
- May be accompanied by pain or immediately follow an attack of pain. Although there are cases of nausea regardless of pain.
- Nausea is caused by alcoholic and carbonated drinks, strong tea and coffee, as well as other unhealthy foods, which are strictly recommended to be excluded from the diet for pancreatitis.
- The attack often turns into an episode of vomiting, but the nausea is not eliminated and relief is not observed.
How to get rid of the feeling of nausea
If the patient is haunted by fears that vomiting in acute pancreatitis is a constant phenomenon, it is logical to think about how to protect yourself from unpleasant sensations.
Precautionary measures
How to prevent nausea with pancreatitis:
- follow a diet and diet (eat at strictly prescribed times, to the extent prescribed by medical prescriptions);
- monitor the room temperature: the patient should not overheat or become hypothermic, avoiding unpleasant sensations and phenomena.
Diet and nutrition are extremely important. In case of acute pancreatitis, so that vomiting does not bother you, it is advisable not to eat or drink anything other than mineral water or rosehip decoction. The recommendation will eliminate the risk of dehydration and prevent possible attacks of nausea.
After the first days of an exacerbation, introduce easily digestible foods into your diet:
- vegetarian soups (excluding vegetables prohibited for pancreatitis);
- porridge with water (add a small dose of oil for taste, if desired);
- lean meat/fish;
- cottage cheese;
- jelly (with low juice concentration);
- puddings.
It will be necessary to exclude foods that strain the gastrointestinal tract.
Sometimes the body protects itself from excessive food intake and puts a psychological block on it, reducing appetite. The patient is able to listen to the block placed or, conversely, begins to overcome this condition. Staying for 2-3 days without food or trying to awaken your appetite with tasty dishes does not help: the described techniques do not bring relief to the intestines.
Despite the protests of the digestive system, it is required to adhere to the therapeutic diet prescribed by the attending physician. The body must receive energy to function, or the person’s condition will deteriorate sharply.
If, in such an uncomfortable state, the patient feels the need to smoke a cigarette or take a dose of alcohol, it is better to drive annoying thoughts away. Nicotine and alcohol cause the same negative reaction in the body and will lead to consequences much more unpleasant than vomiting due to pancreatitis.
If the patient is in remission and experiencing nausea, there is a reason to temporarily return to a strict diet.
What to do if the patient feels nauseous
There are a number of options for getting rid of nausea in acute pancreatitis:
- It is advisable to refuse food for the whole day and drink exclusively mineral water.
- In addition to mineral water, you can use rosehip decoction or dilute lemon juice with boiling water. Lemon is not recommended for pancreatitis; by reducing the concentration of substances in the juice that can cause digestive difficulties, you will be able to temporarily get rid of vomiting and nausea.
- It is recommended to lie down, relax, and apply ice to your left side. If there is no ice, a towel soaked in cold water will do. Some doctors advise applying cold closer to the back. Try both options, using the effective one.
Recommendation: an attack of vomiting is a way to get rid of stress and bring relief. After the vomiting attack ends, rinse your mouth, drink mineral or acidified water (for example, a solution of lemon juice), lie down in a cool place and complete rest.
Periodically take an antispasmodic pain reliever if the vomiting is intolerable. No-shpa will do. The tablet may not work, use an injection. If the result is positive, record the result using a proven method in the future.
Taking care of the body during an acute attack is the job of the attending physician. By making an appointment, the patient will receive advice from a professional who is knowledgeable about the patient’s condition. Self-medication will be harmful for such a serious illness.
If an attack of pancreatitis is so severe, the only option left is to call an ambulance; you will need to ensure the most gentle transportation possible. Before the carriage arrives, it is advisable to lie in a cool room, in complete peace, with a cold compress applied to your side (or back).
Inflammation of the pancreas (i.e. pancreatitis) is a fairly common disease of the gastrointestinal tract throughout the world. A variety of factors can provoke it. Nausea with pancreatitis is one of the leading symptoms.
Basic recommendations for eliminating the urge to vomit
Often an attack of pancreatitis is not limited to nausea. Episodes of severe vomiting occur, which does not bring relief, but only exhausts the body already affected by the disease.
As the patient's condition worsens, inclusions of mucus and bile may be observed in the vomit. With exacerbation of the disease, pathologies of the bile ducts are observed, which lead to the release of bile into the stomach.
Vomiting can be accompanied by severe attacks of pain and last for quite a long period of time, depending on the severity of the disease. It may also be accompanied by lack of appetite, bitterness in the mouth, bloating, belching, colic and diarrhea.
During attacks of vomiting, the following recommendations must be followed:
- Don't try to hold back vomiting, even if it doesn't bring relief. Containing vomit can cause severe intoxication of the body and lead to serious consequences that will need to be treated for a long time.
- Stay hydrated. Vomiting can lead to dehydration, which is extremely undesirable when treating a pancreas debilitated by pancreatitis.
- In the first days of an attack, observe bed rest and therapeutic fasting to ease the attacks.
Why does nausea occur?
First, let's figure out what pancreatitis is and why this disease manifests itself as an unpleasant nagging sensation. Pancreatitis is an inflammation of the pancreas and is more common in women than in men.
When there is inflammation in the tissues of the gland, it cannot fully perform its functions, which means that the normal production of enzymes either stops altogether (with complete necrosis of the pancreas) or is reduced to a certain extent depending on the severity of the process and the type of pancreatitis (acute or chronic). All this time, when there are not enough enzymes, patients experience heaviness in the stomach because the stomach cannot cope with the food being digested.
Without the necessary enzymes, it simply does not have the ability to qualitatively transform the food received so that it can further move through the intestines. As a result of this imbalance, patients feel nausea from half-digested food, which releases gases and begins to decompose to a certain extent.
Nausea with pancreatitis develops due to improper functioning of the pancreas and stomach
There is also a second serious reason why this symptom occurs - disturbances in the enzyme conversion chain. To obtain complete digestive enzymes, the pancreas first produces so-called proenzymes - immature enzymes that are not ready for their role.
https://www.youtube.com/watch?v=0TUzrBR-JFo
The next stage of the reaction is the production of complete enzymes. The failure occurs precisely at this moment, so the proenzymes are not transformed, but accumulate in the pancreas itself, causing nausea and pain. The consequences of impaired enzyme formation can be as follows:
- enzymes accumulated in the pancreas digest the tissue of the gland itself, provoking or intensifying the pathological process;
- due to improper enzyme formation, the stomach suffers from a lack of elements that are very important for itself, so its food, untreated with enzymes, begins to release toxins.
After vomiting, the patient's condition may improve
Severe nausea often ends with vomiting, since the body experiences severe intoxication at this time, and it has a natural reflex to eliminate the cause that caused the illness. At the initial stage, the stomach gives out all the contents that it could not process, and according to the residual principle, bile and gastric juice are released.
The following factors can provoke unpleasant symptoms of pancreatitis:
- binge eating;
- consumption of prohibited foods, neglect of food preparation methods;
- drinking alcohol.
Nausea can be caused by both eating prohibited foods and simply overeating.
What to do first?
Getting rid of nausea with pancreatitis is not as easy as it might seem at first glance. First of all, you need to monitor your lifestyle and determine the exact cause of nausea.
If sensations provoke eating, you need to tighten your diet. For unbearable and painful episodes of nausea, it is recommended to completely avoid eating food for several days, that is, go on a hunger strike. To prevent exhaustion of the body, you should consume a decoction of rose hips or still table mineral water.
After improvement, it is necessary to return to the diet recommended by the gastroenterologist for pancreatitis. Food should be easily digestible and not irritate the walls of the pancreas. If episodes of severe nausea return, it is necessary to return to therapeutic fasting.
One of the basic rules for pancreatitis is to keep the affected organ cold. This is necessary because if the pancreas overheats, a new attack of nausea may occur.
To cool the organ, you can use a heating pad with cold water or other devices wrapped in a thin towel. But don’t overdo it: the temperature should be comfortable.
Ways to eliminate symptoms of pancreatitis
You can combat the manifestations of nausea during pancreatitis at the first stage as follows:
- Prevent symptoms of dehydration.
- Start drug treatment for the disease.
- Go on a special diet.
If a person has pancreatitis, then nausea can be stopped in the first days by taking large amounts of water or rosehip decoction. This must be done to prevent dehydration. Transferring the patient to a cool place in the room, out of direct sunlight, can reduce attacks.
If the patient has been examined and the diagnosis is confirmed, the doctor will prescribe the necessary medications. For mild nausea, medical intervention is not required, since taking rosehip decoction helps stabilize the situation.
What to do if a patient has chronic inflammation of the pancreas? Such patients experience loss of appetite and refuse to eat in order to relieve severe pain. A hunger strike is dangerous for them, so such people are put on a special diet. It is agreed upon with the attending physician.
If the pancreas constantly hurts, the nausea does not go away, and the measures taken do not help, then the question of performing a surgical operation may arise.
If the above methods reduce the symptoms of the disease, the patient is transferred to the second stage of treatment. Instead of a strict diet, the patient’s menu for 4-7 days includes light dishes, such as vegetable soups, lean meat, various cereals, compotes, and jelly.
If the nausea intensifies again, the person will have to be put on a strict diet prescribed by the doctor.
When an attack occurs while a patient is walking, at work, or elsewhere, the following methods can be used to eliminate symptoms:
- If you feel nauseous, you need to lie down and put something cold under your ribs on your left side, such as a bottle of cool water or a piece of ice.
- You can get rid of nausea by drinking water with lemon added. This will reduce discomfort.
Acute pancreatitis - manifestations
A mild form of acute pancreatitis is manifested by vomiting, which is repeated once or twice, or may be absent. Sometimes it develops after a certain time from the onset of the disease and is associated with inflammation of the biliary tract or diet disorders.
In general, uncontrollable vomiting in acute pancreatitis does not bring relief. The presence of urge in the absence of vomiting is a common sign of acute pancreatitis. Pain is accompanied by anxiety and fear. In this case, severe bleeding often develops, resulting in shock or collapse, which can also cause nausea and vomiting.
Interstitial and necrotic inflammation of the gland
In patients with acute interstitial (edematous) or hemorrhagic (pancreatic necrosis) pancreatitis, the clinical picture is different.
Interstitial (edematous) pancreatitis
- severe pain;
- repeated repeated vomiting with a large amount of vomit (sometimes up to 4-6 liters), which contains remnants of undigested food, subsequently mucus and bile appear;
- lack of relief after an attack;
- increased vomiting after several sips of water;
- lasting 3–7 days;
- bitterness in the mouth;
- sometimes - “coffee grounds” vomiting associated with bleeding from eroded pancreatic vessels.
To stop vomiting, conservative therapy and therapy to help reduce swelling are prescribed.
Hemorrhagic (necrotizing) pancreatitis
With necrotizing pancreatitis, which is provoked by alcohol, necrosis of pancreatic tissue develops, which is accompanied by:
- excruciating pain of high intensity;
- the smell of alcohol coming from vomit;
- debilitating vomiting with mushy masses consisting of blood, undigested food and bile;
- melena, indicating bleeding in the upper digestive tract.
All this leads to severe dehydration. Happens:
- loss of sodium, calcium and chlorine ions;
- development of collapse or shock;
- aspiration of vomit;
- stopping breathing.
Manifestations of chronic pancreatitis
In chronic pancreatitis, moderate vomiting is usually observed 2-3 times. In a severe attack, it can be repeated; it occurs against the background of severe pain, provoked by gross non-compliance with the diet or alcohol intake.
An attack develops 6–12 hours after a malnutrition or 48–72 hours after consuming alcoholic beverages.
- vomiting mixed with bile and duodenal contents;
- lack of blood in the vomit;
- the duration of the attack is four hours;
- pain.
In addition to the above, we are also concerned about:
- bitterness in the mouth;
- diarrhea;
- flatulence;
- heartburn;
- lack of appetite.
Symptoms of chronic inflammation in remission
During the period of remission, chronic pancreatitis is manifested by nausea and isolated episodes of vomiting. This is usually due to:
- eating disorders;
- lack of enzymes;
- pathology of the digestive organs.
The latter include:
- duodenal ulcer;
- gastritis,
- biliary dyskinesia;
- cholecystitis.
In these cases, vomiting is not accompanied by pain and causes noticeable relief. If pain is present, it is not as intense as with acute pancreatitis. After each meal, nausea intensifies and vomiting becomes more frequent. The more a person eats, the more risk they are exposed to.
Lack of appetite can be considered as a protective reaction of the body against possible deterioration of the condition. In such cases, you need to reduce portions, increase the frequency of meals, and follow the diet and regimen.
Description of the characteristic
Nausea is one of the main symptoms of pancreatitis. Present in 70-80% of patients. An increase in the intensity of a trait can occur either gradually or spontaneously when interacting with certain negative factors.
Vomiting with pancreatitis does not relieve nausea. The symptom can be either short-term or permanent. Usually the symptom depends on the painful syndrome and appears together with it or after it.
Nausea often after eating
Most often, nausea occurs after eating food. Any harmful product can provoke a symptom. That is why, after diagnosis, the patient is recommended to adhere to a strict diet. The heavier the dish is for the gastrointestinal tract, the higher the risk of a negative sign.
Nausea may cause a decrease in appetite. This is a natural reaction of the body aimed at protecting against the recurrence of the symptom.
In most cases, nausea is caused by alcohol-containing drinks. If you suspect the presence of pathology, it is important to immediately stop drinking alcohol.
Pancreatitis is the result of pathology of the biliary tract
According to statistics, about 70% of acute pancreatitis or exacerbations of chronic pancreatitis are provoked by diseases of the biliary tract. These include:
- biliary dyskinesia;
- exacerbation of calculous cholecystitis;
- obstructive jaundice.
With obstructive jaundice, spasm of the sphincter of Oddi occurs, dyskinesia of the biliary tract and blockage with stones develop. Bile enters the intestines and stomach and appears in the vomit.
A similar picture develops with swelling and sclerosis of the head of the pancreas.
In acute pancreatitis or inflammation of the pancreas during the chronic course of the disease caused by alcohol intake, bile is also found in the vomit. Abuse of alcoholic beverages causes spasm of the sphincter of Oddi, an increase in intraductal pressure, which results in inflammation of the pancreas.
Nausea and vomiting continue to bother you for a long time during the recovery period. The inflammatory process is not pronounced, and the presence of dyspeptic symptoms is explained by a lack of enzymes and diseases of other organs of the digestive system.
What to do if vomiting develops
If vomiting occurs, medications are used to help replenish lost fluid and restore electrolyte balance:
- infusion therapy to normalize the volume of fluid and electrolytes;
- analgesics;
- anti-vomiting agents.
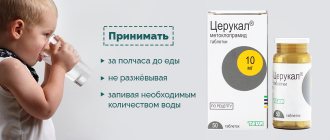
The latter are used when the attack continues despite treatment. They belong to various pharmacological groups, their use is symptomatic therapy: Domperidone, Domidon, Cerucal, Metoclopramide, Reglan, Osetron, Ciel, etc.
Self-treatment of vomiting fails, because taking drugs in tablet form is ineffective: they do not have time to be absorbed in the stomach. Infusion therapy is required in a hospital setting. It is prescribed depending on the severity of the condition individually in each specific case. Stopping vomiting without further detoxification therapy will cause the accumulation of toxic substances and increased intoxication.
The high mortality rate from pancreatitis and its complications is due to late seeking medical help.
If vomiting occurs, you must contact a specialist for examination, clarification of the diagnosis and prescription of treatment, taking into account the identified causes. Only a doctor can adequately assess the condition and prescribe complete treatment that will lead to success.