The pancreas (lat. pancreas) is an endocrine organ of mixed secretion that performs digestive and sugar-regulating functions in the human body. Phylogenetically, this is one of the most ancient glands. For the first time, its rudiments appear in lampreys; in amphibians, a multilobed pancreas can be found. The organ is represented as a separate formation in birds and reptiles. In humans, this is an isolated organ, which has a clear division into lobules. The structure of the human pancreas differs from that of animals.
Anatomical structure
The pancreas consists of three sections: head, body, tail. There are no clear boundaries between the departments; division occurs based on the location of neighboring formations relative to the organ itself. Each section consists of 3-4 lobes, which in turn are divided into lobules. Each lobule has its own excretory duct, which flows into the interlobular ones. The latter are combined into shares. Uniting, the lobes form the common pancreatic duct.
Opening of the common duct is variant:
- Along the way, the common duct unites with the common bile duct, forming the common bile duct, which opens with one hole at the apex of the duodenal papilla. This is the most common option.
- If the duct does not unite with the common bile duct, then it opens with a separate opening at the top of the duodenal papilla.
- The lobar ducts may not be united into one common one from birth; their structure is different from each other. In this case, one of them unites with the common bile duct, and the second opens with an independent opening, called the accessory duct of the pancreas.
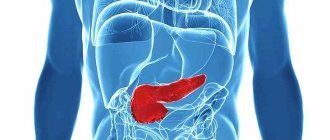
Position and projection onto the body surface
The organ is located retroperitoneally, in the upper part of the retroperitoneal space. The pancreas is reliably protected from injury and other damage, since in front it is covered by the anterior abdominal wall and abdominal organs. And at the back - the bony base of the spinal column and the powerful muscles of the back and lower back.
The pancreas is projected onto the anterior abdominal wall as follows:
- Head – in the left hypochondrium;
- Body – in the epigastric region;
- The tail is in the right hypochondrium.
To determine where the pancreas is located, it is enough to measure the distance between the navel and the end of the sternum. Its bulk is located in the middle of this distance. The lower edge is located 5-6 cm above the navel, the upper edge is 9-10 cm even higher.
Knowledge of the projection areas helps the patient determine where the pancreas hurts. When it is inflamed, the pain is localized mainly in the epigastric region, but can radiate to both the right and left hypochondrium. In severe cases, pain affects the entire upper floor of the anterior abdominal wall.
Skeletotopia
The gland is located at the level of the first lumbar vertebra, as if going around it. High and low placement of pancreas is possible. High - at the level of the last thoracic vertebra, low - at the level of the second lumbar vertebra and below.
Syntopy
Syntopy is the location of an organ relative to other formations. The gland is located in the retroperitoneal tissue, deep in the abdomen.
Due to its anatomical features, the pancreas has a close interaction with the duodenum, aorta, common bile duct, superior and inferior vena cava, and superior branches of the abdominal aorta (superior mesenteric and splenic). Pancreas also interacts with the stomach, left kidney and adrenal gland, and spleen.
Important! Such close proximity to many internal organs creates a risk of spread of the pathological process from one organ to another. With inflammation of any of the above formations, the infectious process can spread to the pancreas and vice versa.
The head is completely enclosed by the bend of the duodenum, and this is where the common bile duct opens. In front of the head are the transverse colon and the superior mesenteric artery. At the back are the inferior vena cava and portal veins, renal vessels.
What to do
In order for the pancreas to resume its work and function normally, it is regularly cleansed. For example, for two weeks, every morning after 6-10 hours, eat 15 dates on an empty stomach. You can wash it down, but only with boiled water or spring water, if available. After half an hour they start eating.
We also recommend viewing: Diet for pancreatic disease
In the absence of dates, cleansing can be replaced by taking buckwheat for ten days. This procedure is done as follows: a glass of buckwheat is washed and filled with kefir in a volume of 500 grams per glass of buckwheat. In the morning, divide the resulting porridge into two parts: eat one instead of breakfast, and the second a couple of hours before bed.
Fresh parsley juice is also useful for restoring the functioning of the gland. To do this, several bunches of green parsley are chopped in a mixer with the addition of lemon. The crushed mass is transferred to a fine sieve and a container is placed under it. Then pour the mixture into a sieve with one and a half liters of clean boiled water. The resulting liquid is poured into another container and consumed throughout the day; honey can be added to taste. You need to drink up to three liters of fluid per day. During this period, it is recommended to avoid drinking coffee and black tea. These drinks can be replaced with mineral, boiled or spring water. A variety of dried fruit compotes or natural vegetable and fruit juices are also suitable. In the morning, switch to drinking herbal tea, to which you can add a small amount of green tea, rose hips or hibiscus tea.
To stimulate the glands, include a variety of spices in the diet, onions, garlic, ginger and horseradish; it should also contain legumes and sprouted grains. Daily consumption of raspberries, sorrel, barberry and pomegranate has a good effect on improving the functioning of the pancreas. Taking infusions of string, linden blossom and wild strawberry also has a beneficial effect.
To restore the functioning of the gland, you must stop eating fatty, fried, smoked foods and reduce alcohol consumption to a minimum. You can give up sugar for a while and eat more plant-based foods.
Histological and microscopic structure
If you look at the section under magnification, you will notice that the gland tissue (parenchyma) consists of two elements: cells and stroma (areas of connective tissue). The stroma contains blood vessels and excretory ducts. It communicates between the lobules and promotes the release of secretions.
As for cells, there are 2 types of them:
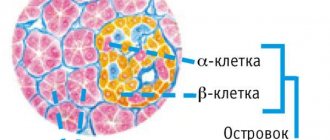
- Endocrine - secrete hormones directly into adjacent vessels, performing an intrasecretory function. The cells are united among themselves into several groups (islets of Langerhans). These pancreatic islets contain four types of cells, each of which synthesizes a different hormone.
- Exocrine (secretory) - synthesize and secrete digestive enzymes, thereby performing exocrine functions. Inside each cell there are granules filled with biologically active substances. The cells are collected in terminal acini, each of which has its own excretory duct. Their structure is such that they subsequently merge into one common duct, the end section of which opens at the apex of the duodenal papilla.
Physiology
When food enters the stomach cavity and its subsequent evacuation into the cavity of the small intestine, the pancreas begins to actively secrete digestive enzymes. These metabolites are initially produced in an inactive form, as they are active metabolites that can digest their own tissues. Once they enter the intestinal lumen, they are activated, after which the cavity stage of food digestion begins.
Enzymes that carry out intracavitary digestion of food:
- Trypsin.
- Chymotrypsin.
- Carboxypeptidase.
- Elastase.
- Lipase.
- Amylase.
After digestion is complete, the broken down nutrients are absorbed into the blood. Normally, in response to an increase in blood glucose, the pancreas will immediately respond by releasing the hormone insulin.
Insulin is the only glucose-lowering hormone in our body. This is a peptide whose structure is a chain of amino acids. Insulin is produced in an inactive form. Once in the bloodstream, insulin undergoes several biochemical reactions, after which it begins to actively perform its function: to utilize glucose and other simple sugars from the blood into tissue cells. With inflammation and other pathologies, insulin production decreases, a state of hyperglycemia occurs, and subsequently insulin-dependent diabetes mellitus.
Relationship between functions and the structure and location of the gland
The functions of the pancreas depend on the characteristic features of the structure and location of organs in the abdominal cavity. The correct location of the organs contributes to high-quality threshing of food and normal secretion of the necessary enzymatic substances and other components involved in the digestive process.
The parts of the pancreas are conventionally divided into: head, body and tail.
structure of the pancreas
The head is located in the duodenal arch. Connects the liver and pancreas through the major papilla and various ducts, including the bile duct.
The body of the organ is covered with peritoneum in front, and the tail borders the spleen.
The organ plays an important role in the assimilation of food. Without it, it is impossible to transform food macromolecules into smaller segments that can be absorbed into the blood. Cleavage to monomers allows their absorption in the small intestine. Digestion itself is conventionally divided into mechanical and chemical. Pancreatic juice, together with gastric juice and bile, plays an important role in breaking down chyme (a semi-digested lump of food) into molecules.
The functions of the pancreas play the most important role in the human body. If there is a disruption in the activity of any part of the organ, the activity of the entire body is disrupted.
Functions performed and role in metabolism
The pancreas is an organ of the endocrine system that belongs to the mixed secretion glands. It performs exocrine functions (production of digestive enzymes into the cavity of the small intestine) and intrasecretory functions (synthesis of sugar-regulating hormones into the bloodstream). Playing an important role in our life, pancreas performs:
- Digestive function - participation in the digestion of food, the breakdown of nutrients into simple compounds.
- Enzymatic function - production and secretion of trypsin, chymotrypsin, carboxypeptidase, lipase, elastase, amylase.
- Hormonal function - continuous secretion of insulin and glucagon into the bloodstream.
The role of individual enzymes
Trypsin . It is initially released as a proenzyme. Activated in the cavity of the small intestine. Once activated, it begins to activate other digestive enzymes. Trypsin breaks down peptides into amino acids and stimulates the cavity digestion of food.
Lipase . Breaks down fats into fatty acid monomers. It is released as a proenzyme and is activated by the action of bile and bile acids. Participates in the absorption of fat-soluble vitamins. The level of lipase is determined during inflammation and other pathologies.
Amylase . Marker of pancreas cell damage, organ-specific enzyme. The level of amylase is determined in the first hours in the blood of all patients with suspected inflammation of the pancreas. Amylase breaks down complex carbohydrates into simple ones and helps in the absorption of glucose.
Elastase . An organ-specific enzyme indicating cell damage. The function of elastase is to participate in the breakdown of dietary fiber and collagen.
Functions
The pancreas is an organ of mixed secretion. After all, it consists of different cells, each type of which produces certain hormones or enzymes. It is the pancreatic juice released by the gland that helps digest food normally. And the hormone insulin, responsible for the absorption of glucose, is also produced by this gland.
Therefore, the pancreas performs several functions:
- participates in digestion processes;
- produces basic enzymes for the breakdown of proteins, fats and carbohydrates;
- produces insulin and glucagon to regulate sugar levels.
In order for the gland to properly perform its functions, a combination of many factors is necessary. Her health depends on the normal functioning of the liver, gall bladder, duodenum, proper blood circulation and transmission of nerve impulses. All this affects its functions, mass and structure. The normal size of the pancreas in a healthy person should not exceed 23 cm. And its enlargement may indicate some kind of pathology.
The pancreas performs very important functions in the digestive processes
Digestive function
The pancreas produces pancreatic juice, which contains enzymes necessary to break down proteins, fats and carbohydrates from food. In just a day, approximately 600 ml of juice is produced, sometimes its amount can increase to 2000 ml. And the type and amount of enzymes depend on the nutritional characteristics of a person. After all, the pancreas can adapt and stimulate the production of exactly those enzymes that are needed at the moment.
The production of pancreatic juice begins after food enters the stomach. Although this process often begins at the sight of food or from inhaling its smell. At the same time, a signal is sent to the gland cells through the nerve fibers, and they begin to produce certain substances.
The enzymes that the pancreas produces are produced in an inactive form, as they are quite aggressive and can digest the tissues of the gland itself. They are activated only after entering the duodenum. The enzyme enterokinase is located there. It quickly activates trypsin, which is an activator for all other enzymes. If, under certain pathologies, enterokinase enters the pancreas, all enzymes are activated and begin to digest its tissue. Inflammation occurs, then necrosis and complete destruction of the organ.
The main enzymes produced by this gland break down proteins, fats and carbohydrates
This gland secretes various enzymes. Some of them are able to break down proteins, amino acids, nucleotides, others help in the digestion of fats and the absorption of carbohydrates:
- Nucleases - ribonuclease and deoxyribonuclease break down the DNA and RNA of foreign organisms that enter the digestive tract.
- Proteases are involved in protein breakdown. There are several of these enzymes: trypsin and chymotrypsin break down those proteins that have already been partially digested in the stomach, carboxypeptidase breaks down amino acids, and elastase and collagenase break down connective tissue proteins and dietary fiber.
- Enzymes that break down fats are very important. This is a lipase, which is also involved in the production of fat-soluble vitamins, and a phospholipase, which accelerates the absorption of phospholipids.
The pancreas secretes a lot of enzymes to break down carbohydrates. Amylase is involved in the absorption of glucose, breaks down complex carbohydrates, and lactase, sucrase and maltase release glucose from the corresponding substances.
Special cells located in the islets of Langerhans produce insulin and glucagon
Hormonal function
Few people realize what the pancreas is for. Usually they find out about it when some pathologies appear. And the most common of them is diabetes mellitus. This disease is associated with impaired glucose absorption. This process is ensured by insulin, a hormone produced specifically by the pancreas. If its production is disrupted, the amount of glucose in the blood increases.
Certain pancreatic cells located in the islets of Langerhans produce hormones to regulate the absorption of carbohydrates, as well as to normalize metabolic processes.
- Insulin promotes the conversion of glucose into glycogen. This substance can accumulate in muscle tissue and the liver, being consumed as needed.
- Glucagon has the opposite effect: it breaks down glycogen and converts it into glucose.
- Somatostatin is necessary to block the excessive production of certain other hormones and enzymes.
- Pancreatic polypeptide stimulates the production of gastric juice.
Every person needs to understand what important functions the pancreas performs. It participates in metabolic processes, maintains normal sugar levels, and ensures digestion. Various disruptions in its functioning affect the general state of health and reduce a person’s quality of life.
Inflammation of the pancreas (pancreatitis)
A common pathology among the adult population, in which inflammatory damage to the stroma and parenchyma of the pancreas occurs, accompanied by severe clinical symptoms, pain and disruption of the structure and functions of the organ.
How the pancreas hurts and other symptoms of inflammation characteristic of pancreatitis:
- Pain of a girdling nature, radiating to the right or left hypochondrium. Less commonly, the pain occupies the entire upper floor of the abdominal cavity. The girdling nature of the pain is due to the close location of the superior mesenteric nerve plexus. Due to its structure, irritation of one section of a nerve leads to the spread of a nerve impulse to all neighboring nerve fibers. The pain feels like a hoop squeezing the upper abdomen. Pain occurs after a heavy meal or after a fatty meal.
- Dyspeptic disorders: nausea, vomiting, loose stools (diarrhea) mixed with fat. There may be a decrease in appetite, bloating, and rumbling.
- Symptoms of intoxication: headache, weakness, dizziness. In an acute process, low-grade body temperature is observed. Febrile fever is not typical for pancreatitis.
These signs are characteristic of the edematous (initial) form of inflammation. As the disease progresses, inflammation affects deeper and deeper areas of the tissue, which ultimately leads to necrosis and necrosis of individual lobules, disruption of the structure and functions of the organ. The clinic for this condition is bright, the patient needs immediate medical attention. This is due to the fact that the pain is more pronounced, the patient rushes about and cannot find a comfortable position.
Internal location of the gland in humans
People do not always know what can hurt in one side or another, so it is necessary to know about the topographical location of this important tissue in the body. The head and body of the pancreas are visually located between the 4th lumbar vertebra and the 12th thoracic vertebra. The tail is located between 2 lumbar and 11 thoracic. On average, the size of the gland should not exceed 18 centimeters in length, 3 in width and 2 centimeters in thickness.
Any changes in the size of the pancreas indicate the presence of deviations from the norm. During inflammatory processes it increases, and during atrophy, on the contrary, it becomes less. All these changes can be easily recognized using an ultrasound examination, which will give a visual picture of the size.
How to detect inflammation of the pancreas
To identify a particular pathology of the pancreas, including inflammation, one symptom of pain is not enough. Laboratory and instrumental examination methods are prescribed.
Laboratory methods include:
- Clinical blood test to detect the presence of signs of inflammation and intoxication. Inflammation is supported by an acceleration of the erythrocyte sedimentation rate, an increase in the number of leukocytes, and qualitative changes in the leukocyte formula.
- Blood chemistry. Inflammation is indicated by an increase in total protein and qualitative changes in the protein composition of the blood. If a high content of amylase and other organ-specific enzymes is detected in the blood, then we can speak with complete confidence about damage and destruction of glandular cells.
- Biochemical urine analysis. Damage and inflammation of the gland is signaled by the appearance of diastase (amylase) in the urine.
- Functional tests that evaluate the functioning of the pancreas based on the level of secretion of hormones and enzymes.
- Stool analysis to detect the presence of undigested fats and soaps - steatorrhea. This is an indirect sign of inflammation and dysfunction of the pancreas.
Instrumental methods:
- Ultrasound examination of the abdominal organs. A visual examination method that allows you to evaluate the structure and structure of the pancreas. When inflammation occurs in the parenchyma of the gland, structural changes will occur, which a specialist can clearly see even with the naked eye.
- Magnetic resonance imaging is an x-ray examination method based on contrasting areas of lower density. MRI is performed before surgery to assess the extent of the lesion and the structure of the organ, and the extent of the surgical intervention.
- Fibrogastroduodenoscopy (FGDS). Allows you to assess the condition of the stomach, duodenum and the structure of the duodenal papilla. It is also carried out for differential diagnosis and a more accurate diagnosis.
If necessary, laparoscopy, ERCP, plain radiography of the abdominal cavity, and MSCT can be performed. These methods are necessary for differential diagnosis and more accurate establishment of the etiology and topical diagnosis of the disease.
Where is it located, what is it, what parts does it consist of?
The name of the gland directly indicates its location in the abdominal cavity. The gland is located behind the stomach in the abdominal cavity, although it may move slightly with different body positions. For example, when a person stands, the stomach and gland are approximately at the same level, but in a lying position the stomach hangs over it.
If we consider the position of the organ according to symmetry, then the body of the glandular tissue is located in the center, moving slightly to the left side of the hypochondrium.
The entire gland is anatomically divided into three parts: head, body, tail. It is closely surrounded by the duodenum - this is due to its functional characteristics. The duodenum wraps around the head of the pancreas like a crescent. The glandular tissue is connected to the duodenum by the duct of Wirsung, through which enzymes are supplied to the digestive tract.
The tissue of the gland is a bit like an inverted pyramid, where the head is the thickest, then gradually decreases and goes into the body, and the top of the pyramid is the tail. It is the tail that is responsible for the production of insulin. If pathologies affect this area, the patient may develop a terrible disease called diabetes mellitus.
All parts of the organ are held together by connective tissue called the pancreas capsule.
Endocrine role of the pancreas
The role of the gland is also important in diabetes mellitus. With this pathology, the level of insulin production decreases, and the level of glucose in the blood increases. This leads to the formation of glycated hemoglobin. Ultimately, all transport and metabolic processes in the body are disrupted, immunity and protective forces are reduced. This condition can be compensated by parenteral or enteral administration of exogenous insulin, which compensates for the lack of its own hormone.
Thus, pancreas, performing important functions in our body, contributes to normal digestion and digestion. Maintains blood sugar at a constant level and participates in metabolic processes. When it is damaged, serious disturbances in homeostasis occur, and the level of health and lifestyle decreases. Monitor the condition of the pancreas and do not let the course of possible diseases take their course in order to avoid unpleasant consequences.
Treatment of dysfunction
The functioning of the pancreas can be restored with the help of medications and an appropriate diet. To improve the functioning of the digestive tract, enzyme preparations are prescribed - Creon, Pancreatin, Festal.
If pancreatitis is accompanied by frequent vomiting, then means are used to normalize the water-salt balance, for example, a solution of Sodium Chloride. An integral part of treatment is vitamin therapy. For severe digestive disorders, parenteral or intravenous nutrition is prescribed.
Treatment of acute pancreatitis is carried out only in a hospital setting, therefore, if characteristic signs appear, it is necessary to call an ambulance team. Before the doctors arrive, you should not eat; it is recommended to drink 1/4 cup of water every 30-60 minutes. You can alleviate the condition by sitting with your knees pressed to your stomach. A cold compress applied to the back in the projection of the pancreas will help reduce pain.