Pancreatic failure can occur in patients of any age and gender.
Severe acute pancreatitis or complications after it can be fatal within a few hours. If a significant part of the organ is damaged (total or subtotal pancreatic necrosis), despite timely and adequate assistance provided in full, the best prognosis may be survival with subsequent disability of the patient. The gland, according to various authors, fails in cases of large-focal infection of the pancreas by more than 80%, even when treated in specialized clinics. Cell necrosis occurs at lightning speed: after an emergency operation, it is not always possible to achieve a positive result, and the chance of saving life is reduced to zero. With small focal pancreatic necrosis of a separate part of the pancreas (head, body or tail), mortality rates range from 11 to 40%.
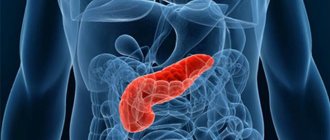
Features of the functioning of the pancreas
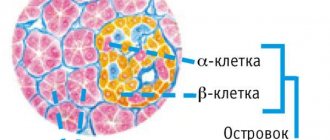
The pancreas (P) is an organ that simultaneously secretes digestive juice containing enzymes and hormones that control metabolic processes in the body. The peculiarities of its functioning are associated with the structure of the parenchyma, which consists of lobules with glandular cells that produce enzymes and islets of Langerhans that synthesize hormones.
In general, the pancreas consists of glandular tissue. It is very delicate, easily vulnerable, susceptible to external and internal factors. It is extremely difficult to operate on the gland or nearby organs: the cells are destroyed even by touch. The changes occurring in the pancreatic parenchyma are irreversible: dead pancreatocytes are not restored, the functions of the organ are lost irrevocably. If most of the normal tissue is replaced by fat or connective tissue, the pancreas will no longer function. Treatment, which in such cases is reduced to replacement therapy, leads to large physical and financial losses.
As a result of pathological processes in the pancreas, the death of all structural components of the tissue occurs with the development of:
- diabetes mellitus with an insufficient number of beta cells that produce insulin,
- acute pancreatitis with all its complications.
Malfunction and possible death of the organ can be caused by various reasons, but the pathogenesis in all cases is approximately the same and is a toxic enzymopathy due to the activation of aggressive enzymes with subsequent self-digestion of the pancreas.
With the death of pancreas tissue and the release of enzymes, hemorrhages and necrosis occur in the tissues surrounding the gland.
In more severe forms, progressive swelling develops. It leads to compression of the vessels supplying the organ, their thrombosis and the formation of significant foci of necrosis. Hypovolemia develops. The following is released from the pancreas and retroperitoneal tissue into the blood:
- toxins,
- biologically active substances (activated enzymes, kinins, histamine).
As a result of their action:
- blood vessels dilate,
- the permeability of the vascular wall increases,
- myocardial contractility decreases,
- endotoxemia occurs,
- Shock and multiple organ failure develop, which is most pronounced when an infection occurs.
Pancreas failed
The most important organ in the gastrointestinal tract is the pancreas. And if we assume that malfunctions begin in its functions, this can lead to destabilization of the entire health.
If the pancreas fails, its signs are very clear:
- severe pain in the left hypochondrium;
- girdling pain;
- bloating;
- wave-like nausea that does not stop, with intensification to uncontrollable vomiting;
- pain subsides in a bent position.
Acute attacks are difficult to relieve, antispasmodics have little effect, vomiting becomes uncontrollable, and the stomach cramps.
Symptoms of pancreas failure
During dynamic monitoring of the course of a sick person’s condition, an increase in temperature to subfebrile levels is determined.
Additional symptoms by which you can determine the failure of the pancreas and not confuse them with the manifestation of other diseases:
- diarrhea;
- increased gag reflex;
- tachycardia;
- sudden attacks of fever and sweating;
- yellowing of the skin and whites of the eyes.
Untreated pancreatitis takes a chronic form and worsens periodically, especially when the diet is violated, after a large feast or an entertainment party with a lot of alcohol. The chronic form of pancreatitis is characterized by a feeling of enlargement of the pancreas, then there is a feeling of fullness in the ribs, and breathing becomes difficult.
When the pain is girdling, the pain is so severe that it can easily be confused with manifestations of osteochondrosis, cholecystitis, pyelonephritis, and appendicitis. It is not difficult to confuse the failure of the pancreas, because with all the strength of the pain, they are quite varied - dull pulling, sharp cutting, strong spasms, or pain of medium intensity continuously lasting for several days.
What to do if the pancreas fails?
In any case, the first actions in case of pancreatic failure are taking antispasmodics, painkillers, anti-inflammatory drugs, switching to a starvation diet, and alkaline drinking. When laboratory confirmation of abnormalities in sugar levels occurs, the patient is prescribed insulin, along with medications containing enzymes.
Causes of pancreas failure
Acute pancreatitis is the main disease of the pancreas and is severe and with complications. The rapid development of the disease is difficult to predict: the patient may die within a few hours or within the first week after the first symptoms appear. The main reasons leading to the occurrence of the disease and its consequences:
- alcohol abuse (25–30%) – causes acute damage to the pancreas in men,
- cholelithiasis (40–70%) - leads to the death of the pancreas in women.
In addition to them, profound changes in the tissues of the pancreas lead to:
- trauma in the area where the organ is located, including surgery on the gland itself or neighboring organs,
- complicated peptic ulcer of the stomach or duodenum with penetration into the head of the pancreas,
- atherosclerotic vascular lesions, leading to the development of ischemia - disruption of the blood supply to the gland and necrotic changes in its tissues,
- Virsungolithiasis - stones in the main duct, disrupting its patency and the secretion of pancreatic juice,
- severe food allergies,
- viral infections,
- hypoparathyroidism.
People at risk are:
- those who abuse fatty, fried and spicy foods,
- with a hereditary predisposition,
- with obesity (the risk of severe pancreatitis increases by 3 times, mortality - by 2).
In total, more than 40 causes that initiate the development of an acute inflammatory process in the pancreas are described in the literature. The largest number of cases is recorded in winter; in summer, their number (especially destructive forms) decreases due to changes in nutritional patterns. In the summer, the consumption of vegetables, fruits, and herbs increases, and fats and meat decreases.
Why does the pancreas become inflamed?
First of all, she takes revenge on us for our own mistakes. The first place in the ranking of “provocateurs” is shared by alcohol and cholelithiasis: this is more than 70% of cases. By the way, acute pancreatitis can suddenly begin in a non-drinker if he has “too much.” In general, experts say, there are more than a hundred reasons for the development of the disease. The most common:
● diseases of the duodenum (duodenitis, peptic ulcer);
● taking certain medications (diuretics, sulfonamides, etc.);
● infections (viral hepatitis B, C);
● metabolic disorders;
Symptoms and signs of pancreatic failure
The main symptoms of pancreatic failure include:
- pain,
- nausea,
- repeated vomiting that does not bring relief,
- diarrhea,
- weakness,
- bloating.
The location of abdominal pain varies, but in 95% it is localized in the epigastrium and may be of a girdling nature. In 50%, the pain symptom is of high intensity and is accompanied by collapse. Abdominal bloating at the onset of the disease is associated with paresis (paralysis) of the transverse colon.
Upon objective examination, both an adult and a child have a severe general condition after failure of the pancreas. Detected:
- marbling of the skin,
- cyanosis,
- dyspnea,
- tachycardia,
- drop in blood pressure to the point of collapse.
Palpation of the abdomen reveals sharp pain in the hypochondrium and epigastrium, and sometimes muscle tension. When pancreatic necrosis has developed, an infiltrate is palpable in the epigastric region. A breakdown, accompanied by an extensive necrotic process in the pancreas, is characterized by symptoms of multiple organ disorder and affects the disorder:
- respiratory,
- cardiovascular,
- hepatorenal function.
Frequent exacerbations of chronic pancreatitis also lead to disruption of the pancreas. With each relapse, the symptoms increase, the person begins to lose weight, diarrhea of a characteristic appearance (gray with a greasy sheen and undigested food residues) becomes constant, the pain becomes more frequent and intensifies, appetite disappears, the gland begins to gradually die and soon stops working. If emergency medical measures are not carried out in a timely manner, this may result in the death of the patient.
Clinical picture of acute and chronic pancreatitis
Sugar level
Man
Woman
Enter your sugar or select your gender to get recommendations
The leading sign of acute inflammation of the gland is “drilling” pain. Initially, they are localized in the epigastric region and in both hypochondriums. Then discomfort may be felt in the back and abdomen.
Common symptoms of acute pancreatitis include frequent vomiting leading to dehydration, belching, flatulence, diarrhea, sudden weight loss, and dry mouth. When the patient's condition worsens, a temperature appears (up to 40 degrees), hypotension develops and the heartbeat quickens.
Often the course of the disease is accompanied by blanching of the integument. And if the face turns blue, then this indicates a severe form of the disease, in which severe poisoning occurs with peripheral circulation disorder.
A third of patients with acute pancreatitis develop a symptom such as jaundice. Sometimes spots that look like petechiae or areas of hemorrhage form on the buttocks, face and abdomen. Large round rashes can also appear on the back, stomach and chest.
The chronic form of pancreatic inflammation is characterized by the replacement of healthy organ cells with connective tissue. The course of the disease is divided into 2 periods - acute and remission. Therefore, depending on the phase of the disease, the intensity of symptoms varies.
Symptoms indicating gland failure in cancer, cysts, diabetes, stones and pancreatic necrosis
With cysts localized in the pancreas, a capsule is formed in the organ where fluid accumulates. The formation can appear in any part of the gland. Its symptoms often occur when the tumor becomes large and displaces nearby organs.
With a cyst, the patient may experience pain in the upper abdomen. It is not uncommon for a person to suddenly lose weight and suffer from indigestion.
A large formation can be felt during palpation. The tumor compresses nearby organs, which impedes the flow of bile. Therefore, the patient may change the color of stool and urine.
If there is a cyst in the pancreas, a person constantly feels weak. If an infection occurs, then signs such as muscle pain, fever, migraines and chills appear.
Symptoms of pancreatic failure due to the formation of stones in the organ:
- paroxysmal pain that occurs in the upper abdomen and radiates to the back;
- when stones move into the bile duct, manifestations of obstructive jaundice appear;
- sometimes there is indigestion.
With pancreatic necrosis, when organ tissue dies, sudden, severe pain occurs in the epichondrium or behind the sternum, often radiating to the collarbone, lower back or back. The pain can be so severe that the person loses consciousness.
Other signs of pancreatic necrosis include dry mouth, tachycardia, shortness of breath, constipation, attacks of vomiting and nausea, and flatulence. The patient suffers from chronic fatigue. A characteristic sign of pathology is the appearance of cyanotic spots on the peritoneum and hyperemia of the facial skin.
Pancreatic cancer is a rare phenomenon, but quite dangerous, so the prognosis for recovery is often unfavorable. The tumor grows rapidly, affecting the upper veins, arteries and vessels of nearby organs.
Since cancer affects the nerve plexuses, the patient experiences severe pain. In the presence of a tumor, rapid weight loss, constant thirst and vomiting are observed, caused by the pressure of the tumor on the gastrointestinal tract.
Patients also complain of dry mouth, a feeling of heaviness in the right hypochondrium and stool upset (liquid stool with an unpleasant odor). In some patients, the mucous membranes and skin turn yellow, which is due to disruptions in the outflow of bile.
If a pancreatic tumor produces an increased amount of glucagon, the patient will experience dermatitis, and glucose levels in his blood will increase. Cancer of a parenchymal organ is dangerous because it gives early metastases to the tissue of the lungs, liver, lymph nodes, etc. Therefore, it is important to diagnose the disease in a timely manner and provide effective treatment to save the patient’s life.
The presence of diabetes mellitus can be determined by a number of characteristic symptoms:
- frequent urination;
- sudden weight loss without changing your diet;
- insatiable hunger;
- numbness of the limbs;
- abdominal pain;
- decreased vision;
- nausea and vomiting;
- dry and itchy skin;
- thirst;
- slow healing of wounds.