Any disease of the pancreas requires a serious approach to nutrition. Improvements directly depend on the food consumed. The danger of the pathology is that beneficial substances cease to be supplied due to the lack of enzymes in the stomach, which are produced by the pancreas. This happens due to swelling of the walls of the bile ducts and stomach. At the same time, the organ continues to produce enzymes that gradually destroy it. For this reason, the main rule of nutrition in the presence of such a problem is to eat in small doses. The body should receive predominantly proteins; it is necessary to additionally compensate for the lack of useful elements through nutritional supplements.
Types of diet
There are two main types of diet - gentle or based on the 5p-1 table. It should be followed from 3 to 10 days after surgery, in the acute stage. The menu involves a sharp restriction of carbohydrates and fats. It is unacceptable to eat any food that can cause bloating or stimulate the secretion of gastric juice. Food should not be fried. Both cold and hot drinks and dishes are completely excluded.
The second option is the 5p-2 diet. It is prescribed during the period of remission, immediately after an exacerbation. Any fried foods are strictly prohibited; food must be grated, boiled or steamed. The diet includes an increased amount of protein-containing dishes and moderate consumption of carbohydrates. Salt in the menu is also reduced to almost zero.
Some dietary features
For pancreatic and stomach pain, no matter what disease we are talking about, diet is first of all indicated. It consists of avoiding heavy foods, fatty foods, and fried foods. It is recommended to eat often, in small portions, under no circumstances to overeat, to exclude alcohol, sweet and carbonated drinks.
Before consuming a product, even if it is recommended by a doctor, you should make sure that it is fresh and of high quality. Features of the diet for a sick stomach are based on the principles of healthy eating.
The diet includes a variety of foods: cereals, meat, fish dishes, soups, dairy products. Refrain from sweets, flour, fatty foods or reduce their consumption to a minimum.
How to create the right menu
Nutrition for pain in the digestive tract is divided into gentle and therapeutic. Sticking to a diet:
- They relieve the digestive tract organs that are unable to cope with “heavy” foods due to diseases or inflammation.
- Normalizes the production of gastric juice and bile production.
Products such as boiled eggs, steamed dishes (cutlets, omelettes), cereals, vegetable purees in water, lean soups, pasta contribute to these goals. But not only these products are allowed. To ensure that a person receives all the necessary nutrients, dishes are combined.
How to cook and eat
It is important not only to know what you can eat if you have a sick stomach and problems with your pancreas, but also how to prepare and eat food. For example, when pancreatitis has moved from the acute stage to the remission stage, you need to eat normally, consuming an acceptable amount of fat. You can even include sugar and salt in your diet. But if the disease is in full swing, fatty foods are contraindicated.
For problematic gastrointestinal tracts, a gentle diet is prescribed, which includes a variety of products:
- stale bread, cereals,
- lean meat, fish,
- vegetables fruits,
- dairy products,
- eggs, especially quail,
- vegetable oils,
- herbal teas, decoctions, slightly carbonated mineral water.
As for cooking methods, meat, fish, and even vegetables are boiled before consumption.
You need to make a rough meal plan. You should stick to your daily routine. It is better to eat food more often, in small portions, combining permitted foods.
What can you eat
Let's look at an approximate list of what you can eat when your stomach, pancreas, or intestines hurt:
- Bread and cereals form the basis of the daily diet. If your stomach hurts, eat dried (yesterday's) bread, crackers, preferably made from unrefined flour, with natural sourdough.
- Vegetable purees.
- Doctors recommend pureed, pureed vegetable soups because they are easily digestible and do not burden the diseased organ.
- Broths and dishes based on them. During an exacerbation and immediately after it, a second or even a third broth is consumed.
- Choose lean varieties of meat. They prefer steamed cutlets made from turkey, chicken, beef, and rabbit. It’s better to cook minced meat yourself, because store-bought ones often contain a lot of fat.
- Include low-fat fermented milk products in the diet: yogurt, kefir, fermented baked milk, buttermilk. You can treat yourself to homemade cottage cheese. To prepare it, take fresh yogurt, and the resulting product is consumed immediately.
- Fresh vegetable salads are good for people with stomach problems. Carrots, cabbage, and beets go well in a salad seasoned with a small amount of vegetable oil.
- Hard-boiled eggs are ideal for breakfast. A protein omelet would also be a good start to the day.
- You can alternate egg dishes with porridge cooked in diluted milk or water. You can add vegetable oils to the finished dish. Butter is often contraindicated; it can overload the stomach and provoke the release of bile, but flaxseed, sunflower, even pumpkin seeds will be beneficial.
- Those with a sweet tooth indulge themselves with light desserts, such as baked apples, marshmallows or fruit marmalade, fruit puree mousse, even marshmallows, if the acute stages of the disease have passed.
- Quench your thirst with herbal teas and water. Vegetable decoctions are also suitable. Together with crackers, they also serve as a snack.
Here is a lunch option that is suitable for a person with a diseased gastrointestinal tract:
- A cup of creamy zucchini soup with croutons.
- A slice of boiled chicken fillet with mashed potatoes and beet salad.
- Baked apple mousse with natural yogurt.
- Chamomile or rosehip tea without sugar, a small cup of unsweetened compote, for example, from dried fruits, without honey, jam or sugar.
All these products are included in the list of what you can eat when your stomach and pancreas hurt, which means they will saturate the body and not overload the digestive system.
What liquids can you drink?
The number of foods and drinks that are useful for pain in the gastrointestinal tract allows you to organize a complete diet.
Drinks that can be consumed by people with digestive system problems:
- unsweetened weak (herbal) teas,
- rosehip decoction,
- compotes of fruits and berries (dried, fresh),
- jelly,
- still mineral water,
- fermented milk drinks (no added sugar),
- fruit drinks.
The listed drinks quench thirst and normalize the process of digestion of food.
Forbidden food
Products indicated for people with gastrointestinal problems spare the gastric mucosa, normalize acidity levels, are easily digested and absorbed by the body. A person feels healthy, and may make the mistake of being tempted by food that looks appetizing, but is contraindicated. Such food includes all “fast” or “street” food, fried, fatty foods, sweets, flour, alcoholic drinks and cocktails, coffee.
Forbidden foods include exotic foods, spicy dishes, and salads generously seasoned with vinegar. Fatty dairy products also fall out of favor. Forbidden food provokes an attack of pain and aggravates the course of the disease.
Foods to Avoid
The basic rule to follow is to reduce to zero foods that stimulate the production of enzymes to break down incoming food. Completely prohibited foods include:
- fat;
- fried foods, such as scrambled eggs, lard;
- meat must be skinned;
- fish cannot be fried;
- sweets and baked goods;
- Ice cream and chocolates are prohibited;
- preserved, smoked and sausages, including even cod liver, due to the large amount of fat they contain;
- dairy products, especially mayonnaise, sour cream, cheeses.
Many fruits and vegetables are acceptable to eat, but some are strictly prohibited, namely:
- White cabbage;
- tomatoes;
- cucumbers;
- grape;
- oranges;
- turnip;
- grenades.
You will have to stop eating mushrooms.
There are also strict requirements for drinks. It is strictly forbidden to drink cold water and coffee. You can have tea, but not strong tea. Some juices, fresh juices and fruit drinks are prohibited: orange, apricot, apple and grapefruit. You can't drink lemonade.
Authorized Products
To reduce the pressure on the organ, therapeutic nutrition is attributed, it introduces dishes that can be eaten with inflammation of the pancreas. This table is aimed at preventing the formation of individual problems and normalizing the condition. It is based on the fact that foods for the pancreas with an increased presence of proteins - up to 130 g, in addition to foods that are rich in potassium.
What foods does the pancreas love?
- In terms of meat, the table is replenished with turkey, chicken, lamb, and lean veal.
- For fish, you can eat perch, cod, and pike perch.
- Bird.
- Flour products – bread, crackers, biscuits, regular bagels.
- Dairy products – you can have 30% hard cheese, 1% milk, 0% yogurt.
- Drinks – banana juice, strawberry juice, dried fruit compote.
In the therapeutic diet, useful foods for the pancreas include semolina, oatmeal, buckwheat and rice porridge, prepared in water.
Then they are ground and can be diluted with milk and water to achieve a semi-viscous consistency. If you prepare porridge using buckwheat and rice flour, the cooking process will be simplified.
dairy
What else can you eat if you have inflammation of the pancreas? Boil and puree potatoes, zucchini, cauliflower, carrots and other approved vegetables. Make steamed puddings from carrots and pumpkin. If we consider how many carbohydrates are in these vegetables and their nutritional value, then zucchini has fewer carbohydrates, as well as nutritional value - carbohydrates 5.99 g, calories 30.56 kcal. Vegetables, for example, such as cauliflower 4.72 g / 33.99 kcal, carrots 12.06 g / 41.07 kcal, potatoes include - 19.81 g / 85.57 kcal. After some time, it is allowed to include peeled tomatoes and grated cucumbers in the table.
Soups are prepared using vegetable broth, to which finely chopped vegetables or well-cooked acceptable cereals are then added. To season soups, use butter, cream, and sour cream.
From fermented low-fat milk products, milk is chosen, which is recommended to be added to food, since patients tolerate whole milk worse. It is also allowed to eat low-fat cottage cheese and make puddings and casseroles. If a person has a calcium deficiency, then it is better to fill the deficiency with calcined cottage cheese. Sour cream is used as a seasoning. Cheese is introduced into food grated.
Meat products are replenished with beef, rabbit, and chicken. It is allowed to eat meat dishes only as soufflés, meatballs, meatballs, and steamed cutlets. You can eat cooked rabbit and chicken meat in pieces.
It is allowed to prepare sauces using vegetable broth, seasoned with sour cream and milk. From fruits, the patient’s table with gland pathology is replenished with marshmallows, mousse, jelly, and jam. In a limited amount, it is allowed to eat berries with fruits that need to be ground in advance. Steam omelette and other dishes and side dishes are also allowed.
jelly
Acceptable food
But do not look pessimistically at the list of foods for problems with the pancreas. In fact, sometimes, but still rarely, you can give yourself a little stomach celebration.
Periodically you can eat:
- chicken and pork liver;
- olive or cedar oil;
- doctor's sausage;
- butter, but with a fat content not exceeding 60%;
- waffles, but without filling;
- marmalade;
- boiled eggs, but no more than 2-3 pieces during the week;
- cinnamon;
- vanillin.
By the way, rock salt can be replaced with sea salt.
What to eat for pancreatitis with pain
When chronic pancreatitis worsens, you should pay attention to the dietary nutrition of treatment table No. 5. This diet meets the body’s needs for this disease more than others; it helps eliminate attacks and prevents the disease from appearing again.
Experts know what you can eat if your pancreas hurts, and give recommendations to patients. The menu may consist of the following dishes:
- soup - vegetable, cream, with mucous grains (millet is an exception);
- dairy products;
- boiled eggs;
- vegetable stew, which may include zucchini, potatoes, onions, carrots, cauliflower, broccoli, fresh herbs;
- a small amount of animal fats (for example, butter);
- some fresh berries and fruits.
People with pancreatitis should not eat ice cream.
Allowed and recommended foods
To reduce the load on the organ, it is recommended to include the following foods in your diet:
- turkey and chicken meat;
- lamb;
- perch fillet;
- veal;
- cod and other low-fat seafood;
- wheat bread, but stale;
- crackers;
- biscuits;
- jelly, but in small portions;
- You can use almost any soup, but it is better to give preference to vegetarian ones;
- cauliflower;
- baked apples;
- zucchini;
- potato;
- carrot;
- hard cheese, with low fat content, up to 30%;
- yogurt and milk with fat content up to 1%.
Jelly will be useful; you can drink it throughout the day. It is permissible to drink juices, but not industrially produced ones, but freshly squeezed ones from carrots, strawberries (diluted with water 1:1) and banana. You can brew hibiscus, but not more than 2 times a day.
Nutrition depending on the cause of pain
Often pain signals developing pathological processes. Pancreatitis, an inflammatory disease, occupies a leading place among diseases of the pancreas.
The main reason for the development of the disease is a violation of the outflow of enzymes, which can destroy organ tissue and even blood vessels. Fans of spicy, fried, fatty foods, as well as people who abuse alcohol and overeat are susceptible to the disease. The main manifestations of the disease are pain and intoxication.
Acute pancreatitis
An acute process is characterized by intense pain of a dull or cutting nature. Depending on which part of the pancreas was affected, pain may appear in the right or left hypochondrium, under the stomach. If the pathological process affects the entire organ, the painful outbreak is girdling in nature. The pain can radiate to the back, shoulder blade, chest.
Lack of timely medical care is fraught with painful shock, loss of consciousness and even death. In addition to pain, patients experience nausea and vomiting, bloating, belching, heartburn, diarrhea or constipation. There is tension in the abdominal muscles. The acute process can also cause an increase in body temperature, as well as changes in blood pressure.
Acute pancreatitis is an indication for hospitalization. The main goal of treatment is to neutralize pancreatic enzymes that have entered the blood, as well as to combat intoxication. During the acute period, minimal load on the organ should be ensured. In the first days, therapeutic fasting is indicated. In this case, solutions with nutrients are administered intravenously.
In the first few days of acute pancreatitis, therapeutic fasting is indicated. Important! Fasting is considered the most effective method of therapeutic treatment of acute pancreatitis.
Fasting can be dry or with liquid intake. The first method can last no more than 24 hours, then the patient is given a small amount of mineral water without gas, gradually increasing the dosage. After two days, you can consume vegetable broth, after which the diet expands.
Dry fasting is more often prescribed for the chronic form, and fasting with liquid intake - for the acute process. It will help not only relieve the symptoms of the disease, but also speed up the healing process of the organ. In acute pancreatitis, fasting is carried out in a hospital setting. The patient is allowed to drink liquid in unlimited quantities. This can be alkaline mineral water or rosehip decoction.
In case of a chronic process, dry fasting is carried out once a week, while the person must observe strict bed rest. After the acute process subsides, it is important to continue to monitor your diet. Food should be consumed in pureed puree form. Meals should be small portions five to six times a day. Dishes should be comfortably warm.
What can't you eat? The following products are prohibited for pancreatitis:
- fatty foods, broths, smoked meats;
- seasonings, pickles, marinades;
- spicy vegetables and sour fruits;
- confectionery, baked goods;
- soda, alcohol;
- chocolate, ice cream;
- cocoa, coffee.
For pancreatitis, sour fruits are prohibited
Therapeutic nutrition includes a sufficient amount of healthy and tasty foods:
- boiled, stewed or steamed vegetables;
- lean meat, fish and poultry;
- cereals;
- vegetable soups;
- baked apples;
- jelly, compotes;
- Vegetable oil is allowed to be included in the diet, but it should not be subjected to heat treatment.
Chronic pancreatitis
In a chronic process, an attack of pain can bother a person for a long period of time. Bends and squats increase the intensity of the pain syndrome. Errors in nutrition can cause another attack.
Chronic pancreatitis is a wave-like process. Relapse is replaced by a stage of remission. During an exacerbation, patients are prescribed fasting, as well as during an acute process. Adequate nutrition can be prescribed only a few days after the onset of an exacerbation, when the activity of pancreatic enzymes decreases, the inflammatory reaction subsides and the swelling of the pancreas subsides.
Starting from the third day, additional products are introduced. Dishes should have a homogeneous and viscous consistency. This could be mashed potatoes, porridge, pureed soups, biscuits, crackers.
Although diet alone cannot cure chronic pancreatitis, it will help improve the patient’s quality of life
Pancreas and alcohol
Alcohol abuse has an extremely negative effect on the condition of the pancreas. The cells of this organ are even more affected by alcohol than the liver cells. Scientists were able to establish that alcohol causes 50% of the inflammation in the organ. It is not able to break down alcohol, and when it gets into it, alcohol causes spasms. As a result, protein plugs appear, which over time can turn into dense formations. Over time, the gland begins to become inflamed and, eventually, putrefactive processes begin.
Why does my stomach and pancreas hurt?
Pain in the stomach and pancreas can be caused by various diseases. It is important to distinguish the nature and localization of pain. Pain in the pancreas occurs against the background of the development of pancreatitis, in the presence of cysts and tumors. Stomach pain occurs when:
- poisonings,
- ulcers, gastritis and colitis,
- infectious diseases,
- tumors, polyps.
The nature of the pain is different in each case:
- Peptic ulcer disease reveals itself as spasmodic pain and a burning sensation.
- Dull aching pain indicates the presence of a tumor, and cramping pain indicates an infection.
- Colitis manifests itself as intense pain in the upper abdomen.
- With gastritis, pain appears immediately after eating or when a person is very hungry.
Pain in the abdomen, its nature and location can clearly indicate a disease. However, you should pay attention to the presence of other symptoms:
- constipation, diarrhea,
- nausea and vomiting,
- temperature,
- skin color.
It is important not to confuse gastric diseases with a heart attack or angina, because in both cases the nature of the pain may be similar.
Sample menus and recipes
You need to eat at least 5-6 times throughout the day. The menu could be like this:
| Breakfast | 200 g buckwheat porridge, croutons | 150 g pumpkin-potato puree, croutons | 200 g oatmeal, croutons |
| Lunch | Steamed chicken cutlet, toasted bread, glass of milk | Carrot soufflé, lean meat cutlets | Rice porridge, chicken soufflé* |
| Dinner | Vegetarian soup, fish cutlet | Noodle soup, chicken cutlet | Cauliflower soup**, boiled veal |
| Afternoon snack | Baked apple, kefir | Steamed omelette, fruit jelly | Biscuits, juice |
| Dinner | Cottage cheese, tea with milk, some biscuits | Vegetable stew, boiled chicken | Boiled pumpkin, chicken cutlet |
As you can see even from 3 options, the menu is not so monotonous.
*To prepare chicken soufflé, you will need one poultry breast and an egg, which are mixed in a meat grinder. Milk (150 ml) and a little salt are added to the mixture. The baking dish is treated with vegetable oil and the resulting minced meat is laid out. Bake the dish for 30 minutes in the oven at 200 degrees.
**Cauliflower soup comes together in minutes. The plant is divided into inflorescences, a little chopped carrots and chopped onions are added. All components are filled with a small amount of water and milk. The proportion should be 1:1. Place the mixture on the fire and cook until the cabbage is ready. Add a little salt and grated cheese and boil for another 5 minutes.
General recommendations
Proper nutrition in combination with a healthy and active lifestyle, as well as giving up bad habits, will help speed up the recovery process for diseases of the pancreas. If you have pancreas pain, adhere to the following principles of proper nutrition:
- Eat regularly - every three to four hours. There should not be large intervals;
- the menu should be varied and balanced. The diet should contain a sufficient amount of proteins, fats and carbohydrates, as well as foods rich in fiber;
- try not to overeat, learn to eat small portions of food;
- do not eat cold or hot food, it should be warm;
- frying food is unacceptable if you have pain in the pancreas; it is best to steam, boil, or stew foods;
- You should drink up to two liters of water per day.
Nutrition for pain in the pancreas is prepared taking into account the recommendations of treatment table No. 5. Experts say that the organ is primarily responsible for carbohydrate metabolism, and incoming proteins will not lead to its overload. That is why they recommend introducing protein foods into your diet.
Completely exclude vegetable oil and butter, although the amount of their consumption should be controlled. The diet differs slightly depending on the phase of the disease. What can be eaten during a chronic process should absolutely not be consumed during the acute phase.
If you have pancreas pain, first consult a doctor for a diagnosis
A diseased pancreas is in dire need of gentle nutrition. Let's consider a sample menu for diseases of this organ. For breakfast, it is preferable to prepare oatmeal or semolina porridge. For lunch you can eat vegetable puree or pureed soup. For dinner, cook porridge again, such as oatmeal or buckwheat. For snacks, it is best to use fermented milk products, baked fruits and biscuits.
Now let's look at examples of dishes that can be prepared for diseases of the pancreas:
Is it possible to eat bananas if you have pancreatitis?
- Meat pudding. It is best to cook it in a double boiler. To prepare it you need to take beef, milk, eggs and butter. Be sure to clean the meat from fat and veins. First, the beef is boiled and then passed through a meat grinder. Separate the yolk from the white. You need to add milk, a little salt and yolk to the minced meat. Then the protein should be whipped using a mixer and also sent to a common container. Mix all the ingredients of the dish thoroughly, you should get a paste-like mixture. Oil is necessary to lubricate the container.
- Omelette in a steamer. You will need an egg, water, butter and salt. You can also add vegetables and cottage cheese to taste. All ingredients are mixed until smooth and then placed in a double boiler for twenty minutes.
- Curd soufflé. We will need the following ingredients: cottage cheese, milk, honey, gelatin, cocoa powder. First, you must soak the gelatin in water for thirty minutes. Next, you drain the water and add the remaining ingredients to the gelatin. Then the dish is placed on low heat and brought to a boil.
When your pancreas hurts, drink enough water
Nutrition for pancreatic pain
Severe attacks are relieved with medications. But they are reducing the menu assortment, since it is impossible to do without it. First of all, you need to discard anything with a very high or low temperature. Absolutely everything should be consumed only warm. This applies to any liquid. Fats are immediately excluded; fried foods are under no circumstances allowed. Grated vegetables with a low content of oxalic acid, steamed or boiled are ideal for eating. Kissel, a small amount of puddings and jellies, also prepared in a gentle mode, slimy soups, crackers, and biscuits are introduced.
It is acceptable to eat seafood and meat dishes. However, you will have to choose based on the principle of low fat content in the products.
Recommended menu
A diet for pancreas is prescribed to reduce the secretory function of the gastrointestinal tract and prevent the development of the inflammatory process. Each exacerbation of pancreatitis causes the replacement of functioning connective tissue, provoking the appearance of exocrine insufficiency, manifested in a disruption in the production of enzymes involved in the breakdown of food.
Restricting the diet is designed to relieve the pancreas as much as possible, restore the constitution of the organ, and prevent further tissue destruction.
For chronic diseases
Most often (after the 1st exacerbation), pancreatitis transforms into a chronic pathology, turning into an acute form with a sharp violation of the dietary regime.
Nutrition principles:
- It is allowed to eat dishes prepared in a double boiler by boiling, stewing and baking.
- Vegetables and meat, chicken should be chopped before serving.
- It is prohibited to consume foods high in oxalic acid, containing coarse fiber and tanning microelements. It is dangerous to include in the menu food that causes increased secretion of digestive juice.
- Daily nutrition is based on the predominance of carbohydrates and protein products in the menu. Fats are strictly limited.
- You need to eat 5-6 times a day. It is necessary to consume liquid between meals.
Composition of the daily diet:
- proteins – 120 g (more than half should be vegetable protein);
- fats – 85 g (at least 35% of vegetable origin);
- carbohydrates – 380 g;
- liquid – 1-2 l;
- nutritional value – 2300-2900 kcal.
You should stick to the diet for 6 months. up to 2 years.
Recommended diet:
| 1st day | |
| breakfast |
|
| 2nd breakfast |
|
| dinner |
|
| afternoon tea |
|
| dinner |
|
| before bedtime |
|
| 2nd day | |
| breakfast |
|
| 2nd breakfast |
|
| dinner |
|
| afternoon tea |
|
| dinner |
|
| before bedtime |
|
| 3rd day | |
| breakfast |
|
| 2nd breakfast |
|
| dinner |
|
| afternoon tea |
|
| dinner |
|
| before bedtime |
|
| 4th day | |
| breakfast |
|
| 2nd breakfast |
|
| dinner |
|
| afternoon tea |
|
| dinner |
|
| before bedtime |
|
| 5 day | |
| breakfast |
|
| 2nd breakfast |
|
| dinner |
|
| afternoon tea |
|
| dinner |
|
| before bedtime |
|
| 6th day | |
| breakfast |
|
| 2nd breakfast |
|
| dinner |
|
| afternoon tea |
|
| dinner |
|
| before bedtime |
|
| 7th day | |
| breakfast |
|
| 2nd breakfast |
|
| dinner |
|
| afternoon tea |
|
| dinner |
|
| before bedtime |
|
In acute form
The inflammatory process in the pancreas is manifested by severe pain, nausea and vomiting. In the acute stage of the disease, fasting (2-3 days) is prescribed. In case of severe weight loss, tube feeding is performed.
During the fasting period the following are allowed:
- mineralized water without gases;
- unsweetened tea drink;
- herbal decoction of rose hips;
From the 4th day the patient can eat. You should eat food in small portions (no more than 100 grams at a time) 5-6 times a day.
Nutrition Basics:
- Only boiled and steamed foods are shown.
- Porridge, meat, and vegetable dishes are thoroughly ground.
- You can only eat warm food.
Daily ration:
- from 1st to 3rd day – 0 kcal;
- from 4th to 7th – 80 g protein, 60 g fat, 90 g carbohydrates. During treatment, a strict ban on the consumption of simple carbohydrates was imposed, due to the possible appearance of digestive secretions.
Suggested meals:
| from 1st to 3rd day |
|
| 4th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
| 5th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
| 6th day | |
| 8:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 20:00 |
|
| after 21:00 |
|
| 7th day | |
| 8:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
In recovery
After completing inpatient treatment, for 14-18 days it is necessary to adhere to a gentle diet aimed at:
- improvement of the gastrointestinal tract;
- preventing increased secretion of gastric juice;
- to exclude a possible exacerbation of the disease.
Nutrition Features:
- Predominance of protein foods. In case of animal protein intolerance, soy products are used.
- Mandatory thermal and mechanical treatment. Only boiled and steamed dishes are allowed. Root vegetables and fruits are used to prepare mousses, baked, and necessarily grated with a blender or using a grater.
- Limit salt (6-7 g).
- Complete exclusion of alcohol, sugar, root vegetables rich in coarse fiber.
- You need to eat 4-5 times a day. Food is served freshly prepared and warm (+ 37 °C).
- Drinking regime – up to 1.2 l.
Food Energy:
- proteins – 100-110 g;
- fats – 70-80 g (up to 20% vegetable origin);
- carbohydrates – 250-350 g (30% simple);
- daily diet – 2590-2790 kcal.
Acceptable menu for a 7-day period:
| 1st day | |
| 8:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
| 2nd day | |
| 8:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 20:00 |
|
| 21:00 |
|
| 3rd day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
| 4th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
| 5th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
| 6th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| 21:00 |
|
| 7th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
During the period of exacerbation
A stay in a hospital setting is indicated. Drug therapy is accompanied by a 3-day exclusion of food followed by a transfer to a diet. Fasting is carried out to prevent the production of enzymes necessary to restore the functions of the pancreas. From the 4th day, the consumption of liquid, ground food is allowed. Shown are jelly containing starch.
Diet basics:
- Strict restriction in food aimed at restoring the functioning of the gastrointestinal tract and relieving pain symptoms.
- Thermal and mechanical processing of manufactured food. Only warm dishes served in ground form, liquid, dairy-free porridges are allowed for consumption.
- The diet is carried out 5-6 times a day.
- A complete exclusion of prohibited foods from the diet is indicated.
Menu for 7 days:
| from 1st to 3rd day |
|
| 4th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| 5th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| 6th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| 7th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
Daily consumption:
- proteins – 65 g;
- fats – 25 g;
- carbohydrates – 350 g (simple quantities are strictly limited);
- water – 1.2 l;
- total – 1000 kcal.
The duration of the strict diet is 10-14 days with a gradual expansion of the daily diet. At the end of the restrictions, the patient is transferred to table 5B.
During remission
Nutrition during the period of stable remission is aimed at:
- prevention of acute attacks of pancreatitis;
- stabilization of the pancreas and gastrointestinal tract;
- maintaining a proper diet.
Diet features:
- You should eat 4-5 times a day.
- Food is boiled, steamed, stewed, baked.
- It is recommended to grind food, but eating soft pieces is acceptable.
- Elimination of fatty, sweet, spicy foods.
Daily diet:
- proteins – 1105 g;
- fats – 95 g;
- carbohydrates – 350-450 g;
- daily consumption – 2700 kcal.
7-day diet:
| 1st day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
| 2nd day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
| 3rd day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
| 4th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
| 5th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| 21:00 |
|
| 6th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
| 7th day | |
| 7:00 |
|
| 11:00 |
|
| 14:00 |
|
| 16:00 |
|
| 19:00 |
|
| after 21:00 |
|
The inflammatory process in the pancreas is an unpleasant pathology that can lead to disruption of digestion and metabolic processes in the body. During therapy, it is necessary to follow a diet aimed at preventing spasms, unloading the gastrointestinal tract and restoring its full functioning.
Article design: Mila Friedan
General tips for organizing nutrition for pancreatitis and gastritis
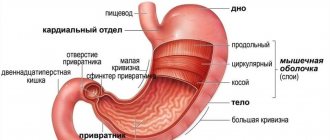
Advice for illnesses is similar. When considering the anatomical location of the internal organs, it is noticeable that the pancreas is located directly above the stomach. Poor functioning of the pancreas causes inflammation of the stomach, the balance of alkali and acids is disturbed - the result is a deterioration in the functioning of the pancreas.
With such a cycle of processes in the digestive system, we will highlight the main recommendations for exacerbation of gastritis and pancreatitis:
- It is necessary to thoroughly grind food when cooking, and chew thoroughly when consuming.
- When cooking, preference is given to steamed, baked, boiled or stewed dishes. Lovers of dishes with a golden crust should forget about their own weakness for such food and use foil when baking.
- You should eat often, eat small portions about the size of your palm.
- The food consumed is received warm.
- It is better to give up the habit of drinking liquid with food, it is better to drink an hour after the main meal.
- You will need to develop a certain diet and strictly adhere to it, without giving concessions.
- You should not overeat before going to bed; it is better to organize your last meal a couple of hours before rest.
Nowadays it is much easier to lead a healthy lifestyle, eat right, kitchen appliances come to the rescue - a blender and a steamer, it’s just a matter of the desire to eat right.
Diet therapy implies a specific list of permitted and prohibited foods. Limited consumption of certain foods will be beneficial for any disease of the digestive system.
What foods are allowed to be consumed?
Acceptable products for exacerbation of pancreatitis and gastritis:
- Lean meat, such as chicken, rabbit, turkey or veal. For gastritis, it is possible to eat a small piece of beef; for pancreatitis, tough meat is not recommended
- Liquid soups (with meatballs, chicken, buckwheat, vegetable, vermicelli). The diet for exacerbation of gastritis is slightly different; broths are included in the list of recommended foods; for pancreatitis, only light vegetable-based decoctions are allowed to be eaten.
- It is allowed to eat yesterday's bread, preferably from whole grains; it is recommended to dry it slightly or eat it in the form of crackers.
- Low-fat fish varieties.
- Fermented milk products: kefir, cottage cheese, cheese. For gastritis with high acidity, it is better to avoid dairy products.
- Eggs.
- In small doses, a teaspoon each, refined sunflower, pumpkin, and olive oils are acceptable; you can add 30 grams of butter, for example, to porridge.
- Cereals – buckwheat, oatmeal and barley, rice and semolina.
- Pasta in small quantities.
- Fruits - apple, pear, banana, for example, in the form of jelly, compote or jelly; the apple can be baked in the oven.
- Vegetables – pumpkin, zucchini, tomato. In case of pancreatitis, fiber-rich vegetables cannot be eaten; in case of exacerbation of gastritis, vegetables, on the contrary, are recommended for consumption.
- As for sweets, the main allowed product is honey and dry biscuits.
Honey for gastritis, enveloping the walls of the stomach, has a beneficial effect in any form of exacerbation. It has antibacterial, healing, anti-inflammatory and soothing properties. Honey components improve the digestive process and reduce acidity. Honey is a permitted product; you can only consume it one spoon a day on an empty stomach.
What foods are prohibited to eat?
The diet for gastritis and pancreatitis is more than strict; in justification, we note that compliance will show a fruitful result after a short period of time.
Prohibited products:
- fatty fish and meat;
- mushrooms;
- cabbage, sorrel, spinach, radish, radishes, beans;
- corn;
- seeds and nuts;
- sausages, smoked, canned, pickled products;
- spices;
- black bread;
- butter and confectionery products, baked goods;
- alcoholic drinks;
- coffee;
- ice cream;
- milk.
The menu seems to be varied, when eating monotonous food, nutritional deficiencies occur, and there is a deterioration in overall health. There is no need to stop following the diet when the first improvements appear.
After the necessary examinations, the doctor will establish the correct diagnosis and prescribe treatment, including proper nutrition. It is acceptable to eat a product from the permitted list, but you should not choose your own diet.
When preparing a diet, gastroenterologists initially rely on the level of acidity in the stomach. If it is elevated, you should limit the consumption of foods that provoke an increase; if the level is reduced, you should give preference to what will increase acid production.
How long to diet
The duration of the diet for patients with gastrointestinal problems depends on the specific disease and its stage. In acute periods of some diseases (for example, pancreatitis or ulcers), hunger is indicated in the first days. Only after an exacerbation can you switch to a gentle diet.
By the way, people who have a sensitive stomach should also follow a diet and pay attention to the foods they eat. The principles of healthy eating are shown to all those who want to be healthy and remain productive.
Symptoms of pancreatic damage are as follows:
- Vomit;
- Nausea;
- Constipation;
- Pain in the projection of the pancreas, radiating to the left hypochondrium.
What you can and cannot eat when your pancreas hurts
What can you eat when your pancreas hurts? This question is often asked by people diagnosed with pancreatitis (inflammation of the pancreas). This is a fairly common illness that forces a person not only to reconsider their diet, but also to make serious adjustments to it. Moreover, there is a reason: eating the “wrong” food always causes a new exacerbation of the disease. What is a healthy food for pancreatitis, and what is it better to abstain from?
Prohibitions on table No. 5
Diet No. 5 is one of 15 nutritional systems that is prescribed for diseases of the gallbladder, bile ducts and liver. In addition to the fact that it provides the body with everything necessary and normalizes the functioning of the affected organs, the processes of bile secretion improve, fat metabolism is unloaded, and most importantly, which is extremely important for pancreatitis, the functioning of the gastrointestinal tract returns to normal.
In case of exacerbation of the disease, this treatment table excludes a number of products:
- fried foods;
- meat and fish with high fat content;
- mushrooms and broths made from them;
- meat and fish broths, especially rich ones;
- fresh baked goods;
- confectionery and chocolate drinks;
- alcoholic drinks;
- spices and herbs.
If a child suffers from pancreatitis, the list of prohibited foods expands, and a more strict diet is recommended.
Avoid the use of:
- any baking;
- sweets;
- eggs, except raw;
- canned and smoked products.
Approximate diet of a child during exacerbation of pancreatitis
It may seem that the table of a small patient becomes very meager, because most of the goodies that children love so much are excluded from the diet. However, the menu still contains useful components that can improve not only the condition of the inflamed gland, but also the general condition of the body.
The daily diet may look like this:
- Breakfast: steam omelette or dairy-free oatmeal porridge.
- 2nd breakfast: carrot and pumpkin pudding, dried fruit compote or rosehip broth, drinks with a little sugar.
- Lunch: for starters - pumpkin soup, lean fish fillet - boiled or steamed, side dish of boiled potatoes; as a dessert you can eat a baked apple; tea.
- Afternoon snack: low-fat cottage cheese casserole and herbal tea;
- Dinner: you can offer your child steamed chicken breast cutlets, carrot or pumpkin juice, or biscuits.
Important information: How to make your pancreas work better
How to set a holiday table with pancreatitis?
Sick people feel awkward during the holidays because the table is full of unhealthy high-calorie foods and alcohol. But a festive dinner with pancreatitis can look solemn and beautiful, and will be healthy. We present unusual dishes that will decorate the holiday and bring joy to the soul and body.
Okroshka for the pancreas
Ingredients:
- kefir – 1 l,
- water – 1 l,
- potatoes – 4 pcs.,
- fresh cucumber – 200 g (1 large),
- quail eggs (chicken can be used, but 4 times less) – 8 pcs.,
- boiled chicken breast fillet – 200 g,
- green onions - a few feathers,
- dill - several sprigs.
Okroshka recipe:
- Boil potatoes, eggs, peel and chop.
- Cut the boiled breast into pieces.
- Peel the cucumber and cut it.
- Wash the greens, remove the hard parts, chop, put in a bowl, add salt.
- Crush the greens so that there is no mechanical damage to the gastrointestinal tract, and also for a greater aroma of the okroshka.
- Combine the chopped ingredients, add kefir and boiled chilled water.
This recipe is unusual, but tasty and healthy.
Veal zrazy stuffed with omelette, with vegetable puree and milk sauce
The dish contains the following ingredients:
For zraz:
- veal – 300 g,
- loaf – 40 g,
- milk – 2 tbsp. l.,
- egg – 1 pc.
For the omelet:
- eggs – 2 pcs.,
- milk - half a glass,
- salt - on the tip of the knife.
For garnish:
- carrots – 1 medium,
- zucchini – 200 g,
- potatoes - 4 medium pieces,
- butter – 20 g.
For the sauce:
- butter – 1 tbsp. l.,
- premium flour – 1 tbsp. l.,
- milk 1.5% – 1 glass,
- a pinch of salt.
The holiday recipe is prepared as follows:
- Beat eggs with milk and salt in a blender for an omelet.
- Grease the frying pan with oil, heat it up, pour in the eggs and milk, cover with a lid.
- Cook the omelette over low heat, cool, and cut into pieces.
- Pour milk over the bread to soften it.
- Grind the meat and bread through a meat grinder, add the egg, salt and mix the minced meat.
- Make 1 cm thick cakes from the minced meat, place an omelette in the center of each, gather the edges of the minced meat up to form balls. Place the zrazy on the grill of the multicooker, pour 2 cups of water into the bottom of the bowl, and close the lid.
- Set the “Steamer” program for 20 minutes.
- For garnish, cut vegetables into pieces and boil in salted water until soft.
- Use a blender to puree the vegetables, add butter, and blend again.
- To make the sauce, fry the flour in oil (or in a dry frying pan) until creamy.
- Pour milk in a small stream while stirring continuously, add salt.
- Cook the sauce over low heat, stirring continuously, until it thickens.
Vegetable puree is placed on beautiful plates, immediately poured over with sauce, and garnished with dill and parsley.
Important points for a festive evening
The holiday will not be a torment for a person suffering from pancreatitis if you follow some rules:
- Set the table with small plates to avoid overeating. A healthy person will add food to himself if he does not eat 1 serving.
- Take breaks between different dishes to allow the previous food to digest.
- Try not to mix several dishes in your stomach so as not to overload your digestive tract.
- Distract yourself for entertainment, communicate more, dance, move. A good mood is good for digestion.
- A beautifully decorated table improves appetite and gives pleasure.
- Remember: alcohol is not a guarantee that the holiday is a success. People who lead a healthy lifestyle have a wonderful time spending their free time without strong drinks.
Menu for acute and chronic forms
http-equiv=”Content-Type” content=”text/html;″>href=”https://diabetik.guru/wp-content/uploads/2017/09/%D0%BE%D1%82%D0% B2%D0%B0%D1%80%D0%BD%D0%B0%D1%8F-%D1%82%D0%B5%D0%BB%D1%8F%D1%82%D0%B8%D0%BD %D0%B0-%D0%BF%D1%80%D0%B8-%D0%BF%D0%B0%D0%BD%D0%BA%D1%80%D0%B5%D0%B0%D1%82 %D0%B8%D1%82%D0%B5.jpg" data-slb-active=»1″ data-slb-asset=»2048761947″ data-slb-internal=»0″>
In case of an acute inflammatory process, eat a steamed protein omelet for breakfast, steamed buckwheat porridge, and drink tea. Steamed curd soufflé is good for second breakfast.
For lunch they eat slimy rice soup with croutons, skinny steamed fish, strawberry jelly with a sugar substitute. For an afternoon snack, prepare a soufflé from dried fruits (preferably dried apricots), and drink a glass of tea without sugar. For dinner, it is recommended to prepare a soufflé from boiled chicken meat, steamed carrots, and drink a glass of rosehip infusion before going to bed.
Causes of stomach pain
In order to understand why your stomach hurts, you must first understand how pain occurs in general. Painful sensations appear when nerve endings are irritated through mechanical damage, inflammatory reactions or spasms caused by nervous stress. This is a kind of signal from the body about pathological processes that it is not able to cope with on its own.
The main factors in the development of pathological processes in the stomach are:
- Poor nutrition:
- dry food (sandwiches, fast food);
- diets that limit the diet (mono-diets) and those that involve a sharp limitation of the daily calorie content of the menu;
- eating food that is too hot or cold causes stomach cramps;
- violation of the regime (two meals a day, overeating in the evening, eating food at night);
- eating rough, fibrous foods;
- a large amount of animal fats, as well as preservatives in the diet;
- carbonated drinks containing sodium benzoate, large amounts of sugar and dyes;
- preference for sour or spicy foods.
- Taking medications that irritate the mucous membranes:
- medications containing acetylsalicylic acid (aspirin);
- paracetamol and ibuprofen, especially in syrup form;
- preparations containing motherwort.
- Constant use of chewing gum stimulates excessive production of gastric juice.
- Intolerance to a certain group of foods, for example, dairy (milk contains lactose), grains (indigestibility of gluten).
- Intestinal infections.
- Pregnancy - hormonal changes affect the production of gastric juice and enzymes, and an enlarged uterus can put pressure on this organ.
- Stress - in stressful situations, the autonomic nervous system slows down intestinal motility and stops the production of gastric juice.
- Drinking alcohol and smoking.
With periodic pain in the stomach, gastroduodenopathy is diagnosed - inflammation of the gastric mucosa, which precedes gastritis. This condition does not require drug treatment and is corrected with the help of a special diet, which involves the consumption of neutral foods and those that eliminate inflammation. However, if the problem is ignored for a long time, complications may arise in the form of gastritis or ulcers.
Often the cause of pain in the stomach can be associated with pathological processes occurring in other organs of the digestive system:
- pancreatitis - inflammation of the pancreas, which is characterized by stomach pain localized in the right hypochondrium, occurring immediately after eating salty, smoked or spicy food;
- cholecystitis - inflammation of the gallbladder, accompanied by cramps and pain in the stomach after eating too fatty or smoked foods;
- duodenal ulcer is accompanied by hunger pains during a long break between meals, mainly at night.
For stomach pain, one of the treatment methods is a special diet that allows you to provide the body with the necessary amount of calories, vitamins and microelements, without overloading the digestive organs. A gentle diet helps restore digestive functions, relieves inflammation, and prevents further damage to the mucosa.
Decoctions, tinctures of herbs and mixtures for the pancreas
Common and readily available herbs for the treatment and prevention of pancreatic diseases are presented below. These herbs have protective and antioxidant properties.
- Birch
- Celandine
- St. John's wort
- Elecampane
- Burdock
- Dandelion
- Chicory
- Mint
- Linen
- Dill
- Plantain
- Sagebrush
- Corn
- galangal
To improve the general condition of these herbs, decoctions, mixtures and tinctures are prepared.
Anti-inflammatory decoction
- To prepare an effective decoction we take in equal proportions herbs listed below:
- Elecampane - 1 tbsp.
- Burdock (root) – 1 tbsp. l.
- Dandelion – 1 tbsp. l.
- Chicory – 1 tbsp. l.
- Boil a teaspoon of the mixture in a glass of water for 15 minutes.
- Leave for 1 hour
- Strain and take 20 ml. before eating
The decoction has anti-inflammatory and analgesic effects.
Choleretic decoction
- We take the following herbs in equal proportions
- celandine
- hop
- dill
- knotweed
- dandelion root
- mint
- linen
- corn silk
- St. John's wort
- Highlander
- immortelle
- Add four tablespoons of the mixture per liter of boiling water
- Take 3 times a day 30 minutes before meals 1/3 cup
- The course lasts 8 weeks. Then a week break. And again the course is repeated. The decoction has anti-inflammatory, analgesic, choleretic, antispasmodic effects
Therapeutic diet according to Pevzner
In medicine, this diet is known as treatment table No. 5 according to Pevzner. It regulates what to eat for inflammation of the pancreas and various diseases of the hepatobiliary system. It is used both in the acute course of the pathology and in the onset of remission.
Important. A feature of chronic pancreatitis is the need to comply with menu restrictions throughout life
Since the diet for acute and chronic disease has certain differences, table No. 5 was divided into additional components. In addition to the standard diet, there are options No. 5a and No. 5p. All three variations should be considered in more detail and their main differences should be highlighted.
In case of exacerbation of pancreatitis, it is recommended to consume jelly and puree side dishes
Table No. 5
The peculiarity of this table is the exclusion of harmful components of the diet of an ordinary person. The total calorie content of the daily menu is limited to 2500 kcal. The amount of protein, carbohydrates and fats is distributed approximately in the following proportion: 4.5:1:1. This system is based on the basic principles described above. It is best to use it in the transition period - after the exacerbation of pancreatitis or cholecystitis has been eliminated.
Sample nutrition menu for inflammation of the pancreas:
- Breakfast: oatmeal with berries and nuts/steamed or baked omelette, compote.
- Second breakfast: baked apple/toast.
- Lunch: steamed vegetables, low-fat sea fish.
- Afternoon snack: berry jelly/rice porridge.
- Dinner: low-fat cheese, chicken breast, broth or green tea.
- Second dinner: fermented baked milk.
The amount of liquid is limited to 1.5-2 liters; its excess will not benefit the body.
Important components of the menu are dried bread, soups and pureed side dishes
Important. In case of exacerbation of pancreatitis, the amount of fluid is reduced for 3-4 days to 1.2-1.5 liters. It should be borne in mind that the dishes on the menu also contain a lot of water.
Table No. 5a
This diet is used for inflammation of the liver and pancreas. It has more stringent requirements than the previous version, so it is usually used only for the period of elimination of an exacerbation, and then switches to a standard therapeutic diet.
Recipes for dishes useful for intestinal pain
There are no particular difficulties in preparing dishes indicated for people with diseases of the gastrointestinal tract. But there are some nuances that you should remember when starting to cook and planning your diet. It is quite possible to take ordinary recipes as a basis. For example, baked apple mousse is prepared as always, but reducing the amount of sugar, or simply doing without it.
The recipe for steamed cutlets includes several ingredients and is easy to prepare:
- any dietary meat – 500 g;
- rice - 2 tablespoons;
- one medium carrot, finely grated;
- salt;
- parsley dill;
- egg;
- a slice of white stale bread soaked in milk or water.
Meat, rice, carrots, herbs and bread are passed through a meat grinder, preferably twice, and mixed with a raw egg. This way the minced meat will come out tender and the cutlets will be softer. Cutlets or meatballs are formed from the minced meat and cooked in a double boiler. The finished dish must cool down. You can add potato or vegetable puree to the cutlets, but seasoning them with tomato paste or hot sauce is contraindicated.
Eating only cutlets is boring, so you can diversify the table with fish dishes. Skinless white fish fillets can also be easily boiled or steamed. Omelettes and light cottage cheese casseroles, porridges, and pureed soups are suitable. Vegetables for soups are boiled in water, the dish is seasoned with herbs, and spices such as pepper are avoided.