Only a qualified doctor can determine whether the stomach or pancreas hurts based on anamnesis, clinical picture and a number of examinations. If pain occurs, it is recommended to consult a doctor immediately.
Loading …
Consult a doctor!
The site provides reference information . Adequate diagnosis and treatment of the disease is possible under the supervision of a conscientious doctor . Any medications have contraindications. Consultation with a specialist and detailed study of the instructions is necessary! Be sure to make an appointment with your doctor .
How to understand if your stomach or pancreas hurts
To understand what exactly hurts, you need to evaluate the clinical picture and conduct an adequate detailed diagnosis.
Pain caused by problems with the pancreas is localized on the right or left side of the abdomen. It can be encircling and radiate to the lower back.
A disruption in the functioning of the gland and a decrease in the synthesis of its enzymes is indicated by the appearance of symptoms such as:
- increased discomfort when eating food or drinking alcoholic beverages;
- increased body temperature;
- feeling of nausea;
- vomit;
- bloating;
- loss of appetite;
- bowel dysfunction in the form of diarrhea;
- the appearance of a bitter taste in the mouth;
- excessive sweating;
- constant dryness in the mouth.
Quite often, pancreatitis is accompanied by hormonal imbalance, and there is a risk of developing diabetes mellitus.
An informative sign is a change in the color of the skin; it becomes yellow.
When inflammation forms in different parts of the organ, pain is felt in different areas:
- in the head - bothers under the ribs on the right;
- in the body – pain radiates to the epigastric zone;
- in the tail - pain occurs under the left ribs;
- throughout the entire organ - a girdling pain, it shoots into the back.
If you have problems with the stomach, pain is felt in the epigastric region; it can have a different character and intensity.
In parallel with this, the patient complains of:
- burning;
- nausea;
- heaviness in the stomach;
- belching.
Severe sharp pain may indicate a peptic ulcer; if it appears suddenly, this often indicates perforation of the ulcer.
Aching pain combined with a burning sensation often indicates the formation of gastritis in its initial or chronic form. It appears immediately after eating or when you feel hungry.
Pain of a constant nature accompanies malignant neoplasms or polyps; if it is cramping, intestinal infections can be suspected.
Causes of pancreatic disease
According to the symptoms of imbalance in the functioning of the pancreas, there are several causes of its occurrence. Sometimes the patient himself is the culprit of the disease; in other cases, problems with the organ are hereditary or congenital.
Pain in the left hypochondrium can be caused by inflammation of the pancreas - pancreatitis. Dyspeptic signs of the disease: nausea in the morning, vomiting after eating, abnormal bowel movements. The patient complains of severe cutting and stabbing pain in the abdomen. The pain persists for a long time, and its intensity does not depend on food intake.
Doctors say the primary cause of this disease in people is alcohol abuse. Then a logical question arises: can the pancreas hurt in children? Doctors note that the course of this disease in a child is not as pronounced as in an adult. The chronic form of pancreatitis in children is often asymptomatic. It is worth noting that the pancreas can also hurt in newborn babies. However, such a disease in babies is extremely rare. A preschool child does not know where the pancreas is or how it hurts. He cannot always accurately describe the symptoms of illness, where he has colitis or pain, describe the feeling of nausea, etc. Therefore, adults need to independently monitor the well-being of their children: pay attention to the structure, color and number of bowel movements, listen to the child’s complaints of pain or burning in the abdomen, examine the condition of the skin, etc.
Other gastrointestinal pathologies can provoke the development of pancreatitis: cholecystitis, cirrhosis of the liver, hepatitis, etc. Injuries to the organ, which subsequently lead to the development of inflammatory reactions, cannot be ruled out.
Pain in the pancreas can be caused by poor diet and taking certain medications. Uncontrolled use of antibiotics by doctors often causes inflammatory processes in the organ.
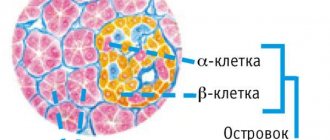
Why does a person’s pancreas hurt? The cause here may be insulinoma - a benign or malignant neoplasm that occurs on the endocrine part of the organ. The pathological growth of beta cells of the endocrine zone leads to the growth of a tumor, which puts pressure on the nerve endings of the tissues and causes pain syndromes. An aching, dull pain in the navel and right side, accompanied by dizziness, headaches, vomiting and general weakness should alert the patient and his doctor. In this case, you cannot delay with additional diagnosis of the disease and appropriate treatment. Some forms of insulinoma require some type of surgery or chemotherapy.
Important information: Where is the pancreas located in humans and how does it hurt?
A dangerous disease of the pancreas is cancer of the organ. Along with dyspeptic symptoms, severe pain occurs in the abdomen and hypochondrium. The patient's back aches, and his veins periodically swell and hurt. The pricking in the pancreas area begins especially strongly at night. It has been observed that pancreatic cancer occurs more often in men than in women.
Quite rarely, stones form in the pancreas. The reason for the appearance of stone deposits has not yet been identified. Doctors suggest that stagnation of pancreatic juice can lead to the formation of stones. A violation of phosphorus-calcium metabolism can also lead to a similar illness. The presence of stones in the gland often goes undetected. The disease may be asymptomatic. Most often, the pain syndrome occurs several hours after eating and has a paroxysmal character. If not treated promptly, the disease progresses. Stones enter the bile duct, causing it to become blocked.
What to do if you have pain in the stomach and pancreas
When diagnosing acute conditions, treatment is carried out in a hospital setting, sometimes surgical interventions are necessary.
For abdominal pain associated with impaired functioning of the stomach and pancreas, the following is considered justified:
- analgesics;
- antispasmodics;
- cytostatics;
- enzyme preparations;
- proton pump inhibitors.
To reduce the intensity of manifestations of intoxication and restore microcirculation, intravenous fluid is administered. In severe and complicated cases, antibiotics may be required.
https://gidpain.ru/bolit/zheludok-podzheludochnaya-opredelit.html
What to do if your pancreas hurts: treatment
When the pancreas suddenly begins to hurt, a person should refuse food and drink.
If possible, you should immediately go to an appointment with a local physician or gastroenterologist. The doctor will prescribe an examination, after which a health restoration plan will be formed.
Drug therapy
Only a doctor can tell you exactly how to treat pain in the digestive gland. Treating any pancreatic disease on your own is dangerous to your health. In the best case scenario, a person will experience diabetes mellitus; in the worst case, complete necrosis of the tissues of the diseased organ, followed by death. Drug therapy for pain in the pancreas depends on the type and complexity of the disease. The treatment regimen may include:
- Anticholinergics - used to relieve pain. For chronic pancreatitis, Gastrin, Pirenzepine, Gastrozipine are prescribed. In case of acute pain, as an ambulance, use Platyfillin, Metacin.
- Ringer's electrolyte solution - allows you to restore water and electrolyte balance in the body and remove toxins. Necessary if acute pancreatitis is accompanied by vomiting and diarrhea.
- Plasma substitutes (Lactasol, Ionosteril) - infused intravenously when plasma volume decreases in order to thin thick blood and restore protein metabolism.
- Antihistamines (Suprastin, Diphenhydramine, Claritin) - enhance the effect of analgesic drugs (Analgin, Baralgin), prescribed for the chronic form of the disease.
- Antibiotics (tetracyclines) are prescribed when there is a change in the structure of pancreatic tissue due to an infection that can occur as a result of injury to the abdominal organs.
- Insulin-glucose therapy - insulin is administered subcutaneously in case of insulin deficiency. This hormone is necessary for carbohydrate metabolism; it is produced by the endocrine part of the gland; intravenous glucose is needed during therapeutic fasting.
- Anabolic steroids (Methandrostenolone, Retabolil) are prescribed to patients who have suddenly lost weight in order to increase the absorption of protein by their body. The drugs increase appetite, promote weight gain, and improve overall health.
- Enzyme medications (Creon, Festal, Pancreatin) - temporarily provide rest to the pancreas and normalize the digestive process.
- Vitamins - in the chronic form of the disease, vitamins of group B, A, C are prescribed orally or intravenously.
After relieving pain in the area of the digestive gland, the patient is recommended, in order to increase the duration of remission, to go to a sanatorium-resort treatment or to a gastroenterological sanatorium.
Diet
In the first days of the disease, the patient is prescribed therapeutic fasting with drinking still mineral water and rosehip decoction. As soon as the patient begins to recover, he is allowed oatmeal. When the pancreas stops hurting, he is switched to a diet containing only dietary fats.
The menu for a person with a diseased pancreas includes:
- first courses with vegetable broth,
- slimy porridges (oatmeal, rice, barley),
- dietary meat (veal, rabbit, chicken), low-fat fish (cod, pollock, flounder),
- stewed vegetables (potatoes, pumpkin, zucchini, carrots, beets, cauliflower),
- low-fat fermented milk products (cottage cheese, kefir, fermented baked milk, hard cheese), unsalted butter, skim fresh milk for making porridge,
- dried wheat bread,
- fruit and berry juices (currants, cherries, pomegranates), weak black or herbal tea without sugar.
Coffee, baked goods, fatty and fried foods, smoked foods, marinades and pickles, and sorrel are excluded from the menu. A diseased organ can begin to hurt even from mushrooms and root vegetables. For pancreatic diseases, drinks that contain alcohol are strictly contraindicated.
Traditional medicine methods
Traditional methods of treating pancreas are best used after consulting a doctor. When using home remedies, there is always the possibility of side effects, which usually include an itchy rash on the skin and deterioration of the digestive tract. The kidneys may suddenly begin to hurt or liver failure may occur.
Milk for pain in the pancreas
How to prepare: rinse 100 g of oats, fill completely with warm water, place in a warm, dark place for 2 days. The oats will sprout. It needs to be dried and ground into powder, then dried again. Then 1 tbsp. l. oatmeal pour 200 ml of cold water. Bring the thoroughly mixed mixture to a boil over medium heat.
How to use: the medicine from sprouted oats should be taken warm 20 minutes before meals (2 times a day).
Result: with regular consumption of oat milk, the pancreas stops hurting. Oats have an anti-inflammatory and antispasmodic effect and help improve carbohydrate metabolism in the gland.
Curdled milk compress for acute pain
How to make: a thin cotton sheet is soaked in cold curdled milk.
How to use: the compress is placed so that it covers the epigastric region and left hypochondrium. The compress is covered with a plastic bag. Wrap the painful part of the body with a warm scarf. The duration of treatment for the digestive gland is at least 4 weeks.
Result: the compress relieves pain, inflammation, and helps restore gland function. It stops hurting due to irritation of the skin with a compress, against the background of which vascular tension in the diseased organ changes, secretory activity is normalized, and metabolism in cells improves.
Medicinal porridge for breakfast
How to cook: in the evening 1 tbsp. l. buckwheat flour (you need to grind the buckwheat yourself), pour in 250 ml of low-fat kefir, mix thoroughly, cover and leave until morning.
How to use: medicinal porridge should be eaten for breakfast. Also during the day you need to drink tea, which is prepared from the same parts of elecampane root, St. John's wort, peppermint, dried cucumber, dill seeds, coriander (pour 1 tablespoon of the mixture into 250 ml of boiling water).
Result: a therapeutic breakfast and herbal tea relieve acute pain in the pancreas and provide long-term remission. The recipe is used until the gland stops hurting completely.
Treating pain with singing
Singing has a positive effect on the condition of the whole body. It helps to get rid of stress, because during singing there is an active production of endorphins. Thanks to him, a person experiences joy, pleasure, and peace. He manages to escape from everyday problems and forget about pain.
The voice vibrates as it sounds, each sound is accompanied by vibrations of high frequencies - overtones. Due to the location of the larynx close to the brain, they resonate with it, affecting the immune system.
A wide range of voice vibration frequencies stimulates blood circulation and tissue nutrition, thereby accelerating the regeneration process and reducing the pathological manifestations of diseases.
During singing, the diaphragm is activated, which massages the liver and prevents congestion in the gallbladder. There is an improvement in the functioning of the abdominal and intestinal organs.
Diagnosis of the disease
Even an experienced doctor is not always able to determine what hurts a person – the stomach or the pancreas. The fact is that the symptoms of diseases of these organs are often difficult to differentiate; they are very similar. Ailments that affect both the pancreas and stomach can manifest as high fever, nausea, stool disorders, and loss of appetite. In addition, each patient feels pain individually: for some, the spasm may be unbearable, for others it is practically unnoticeable and does not interfere with life.
Even a doctor cannot always immediately determine whether the stomach or pancreas hurts.
If moderate pain haunts a person for more than a couple of days, he needs to make an appointment with a therapist or a gastroenterologist directly. If the pain is acute and continuous, it cannot be tolerated. It is recommended to call the emergency team so that doctors can conduct an examination and decide whether hospitalization is necessary.
In any case, whether during an outpatient appointment or upon admission to a hospital, the patient must undergo a series of studies aimed at identifying the diagnosis. As a rule, if a stomach disease is suspected, and if there are symptoms characteristic of pancreatic pathology, approximately the same diagnostic methods are prescribed.
Listen to your doctor and undergo all prescribed tests and procedures
The patient must undergo blood tests, and, if necessary, urine tests and a coprogram. Next, you need to visit an ultrasound room to examine the abdominal organs in real time, detect abnormalities in the contours of the pancreas or stomach, changes in tissues and mucous membranes. Ultrasound diagnostics will reveal an unhealthy organ; to clarify the diagnosis, the following may be prescribed:
- Computed tomography or MPT.
- Endoscopic and laparoscopic studies.
- Tests for tumor markers.
- X-ray diagnostics with contrast.
- Studies of gastric or pancreatic juice and the like.
What does dull, pulling, pinpoint or cutting pain in the stomach indicate?
Dull pain syndrome indicates the following conditions:
- slight spasms of the muscle wall;
- hunger due to lack of contents in the stomach;
- gastritis – inflammation of the mucous membrane of the gastric wall;
- peptic ulcer – deep tissue ulceration due to the proliferation of the bacterium Helicobacter pylori;
- development and reproduction of other bacteria, viruses;
- damage to surface layers under the action of mechanical, physical, chemical, toxic factors;
- allergic reaction, individual intolerance to foods, medications, and other components that penetrate the digestive tract;
- food poisoning, chemicals;
- frequent stress, nervous tension, nervousness;
- benign neoplasms, leading to pain due to proliferation and compression of surrounding tissues;
- flatulence with the formation of gas bubbles that pass through the tract, causing irritation of the walls;
- cancer is a malignant neoplasm that grows and causes metastases in neighboring organs when atypical cells penetrate the systemic bloodstream.
Reasons for the formation of nagging uncomfortable sensations:
- minor injuries without bleeding;
- excessive consumption of alcoholic beverages;
- unhealthy diet with consumption of fatty, spicy, fried, smoked, salty foods;
- long-term drug therapy with nonsteroidal anti-inflammatory drugs that cause damage to the epithelial surface;
- the initial phase of gastritis development.
Point pain syndrome is formed under the influence of the following factors:
- focal damage to different parts of the stomach, pain appears in the area of their localization;
- the initial formation of an injury that extends only to one part of the organ.
Cases of cutting sensations:
- perforation of an ulcer with the formation of bleeding into the abdominal cavity;
- wall rupture due to excessive growth of the tumor;
- exacerbation of gastritis, gastrointestinal tract;
- acute intestinal infection;
- dysfunction of the gastric region;
- heartburn when stomach contents backflow into the esophagus (can develop with a single reflux or gastroesophageal reflux disease).
All types of negative sensations are formed in the stomach not only with its disease, but also with pathologies of neighboring organs. For example, the pancreas, small or large intestine, cardiovascular system.
Spasms of any abdominal organs may occur. Often stomach pain is confused with appendicitis. It is necessary to promptly determine the root cause using diagnostic tests.
Where is the pancreas located and where is the pain localized?
When a person stands upright, the organ is located at the level of 1 lumbar vertebra. It has 3 sections: body, head and tail:
- The body is located behind the stomach;
- The head is located near the duodenum;
- The tail is next to the spleen.
Pain can manifest itself in the hypochondrium or be localized on the right under the scapula. Pain syndrome may appear in the upper abdomen, intensify and spread throughout the abdomen. It is this location of pain that indicates inflammation of the pancreas tissue or pancreatitis: pain is most often associated with this disease.
When do you need to see a doctor urgently, and which doctor will help?
If the pathology is mild or moderate, you can cope at home yourself. In case of prolonged absence of treatment or the development of serious diseases, a doctor will help.
Cases to contact:
- constant feeling of dyspeptic disorders - nausea, vomiting, impaired stool formation (diarrhea, constipation), heartburn, abdominal pain, increased gas formation;
- change in tongue color - yellow, white, gray, black, brown coating;
- a specific odor from the mouth that does not belong to the normal variant - rotten, acetone, egg;
- acute pain attack that occurs suddenly, without an obvious reason;
- ingestion of a foreign object of any size and shape;
- blood in stool or vomit;
- mucus, pus in feces;
- chronic pain for unknown reasons;
- acute pain that is not relieved by analgesics;
- deterioration of health, accompanied by elevated body temperature, especially to critical limits;
- loss of consciousness, sudden drop in blood pressure;
- severe poisoning with manifestations of intoxication of the body, especially from the liver and kidneys.
Doctors to contact when negative clinical signs appear:
- gastroenterologist – pathologies localized in the digestive tract;
- infectious disease specialist – development of infection of any origin;
- neurologist – damage to nerve endings, fibers of the peripheral or central nervous system;
- surgeon – detection of conditions requiring surgery or procedure;
- endocrinologist – diseases of the endocrine glands;
- psychologist, psychotherapist – eliminating frequent worries, worries, and other stress;
- therapist - the development of painful symptoms that cannot be identified during a general examination (after the examination, he sends the patient to other doctors, depending on the data obtained).
The selected doctor prescribes additional tests to help identify the diagnosis. Treatment begins immediately so that the disease does not progress.
Top medications to reduce stomach pain, painkillers
For therapy, drugs of different therapeutic groups are prescribed. Their choice depends on the main diagnosis identified during the examination.
The pain disappears if the following medications are used to eliminate the root cause of the disease:
- antacid substances to reduce the acidity of gastric contents - Maalox, Almagel, Renny, Taltsid, Hefal, Phosphalugel, magnesium or aluminum hydroxide;
- gastroprotectors that envelop the surface layer to reduce the influence of damaging factors - De-nol, Smecta, Sucralfate, Dalargin, Vikair, Biscolcitrate, Misoprostol, bismuth subnitrate or subsalicylate;
- antibiotics (preliminary bacteriological culture is done, with the help of which a number of antibacterial groups are identified to which the microbe is highly or moderately sensitive) - penicillins alone or together with clavulanic acid, aminoglycosides, tetracyclines, erythromycins, cephalosparins;
- antiseptics for the destruction of bacteria contained only in the gastrointestinal tract - Enterofuril, Enterol, Ftalazol;
- antispasmodics for relieving muscle wall tension - Spazmalgon, Spazgan, Papaverine, Halidor, No-shpa;
- sorbents that bind and remove toxins before spreading into the blood - Enterosgel, Polysorb, activated carbon, Polyphepan, Peksesorb, Sorbex, Sorbolong;
- H2-antihistamines to inhibit the secretion of gastric juice - Ranitidine, Famotidine, Cimetidine;
- proton pump inhibitors for the treatment of acid-dependent pathologies by reducing the production of gastric juice - Omez, Losek, Ultop, Lanzoptol, Sanpraz, Pariet, Nexium;
- antidiarrheal medicine to reduce the activity of the intestinal muscle wall - Imodium, Diara, Loperamide, Lopedium, Diasek;
- laxative tablets or suspensions to relieve constipation - Guttalax, Lavacol, Microlax, Dulcolax, Slabilen, Senade;
- products that normalize the microflora of the gastrointestinal tract - Linex, Acipol, Normobakt L, Laktofiltrum, Bifiform, Normoflorin, Bifidumbacterin-forte;
- motor stimulants - Motilium, Motorix, Itopra, Simethicone, Motilak, Trimedat, Domrid.
Painkillers can be taken in a short course, no more than 7-10 days. Otherwise, side effects and addiction will form.
The following groups are used:
- analgesics – Pentalgin, Baralgin, Analgin;
- non-steroidal anti-inflammatory drugs - Ibuprofen, Meloxicam, Diclofenac, Ketoprofen, Lornoxicam, Nise, Nimesulide, Ketanov, Nurofen;
- salicylic acid derivatives – Acetylsalicylic acid, Citramon.
NSAIDs are used by patients who do not suffer from inflammatory pathology of the gastrointestinal tract, otherwise the lesions will develop into ulcers, especially with prolonged use.
Different dosage forms can be used. If they are oral, it must be remembered that some of the substance will be eliminated as it passes through natural physiological barriers.
Injections have a quick effect. But if this remedy is prescribed only for the gastrointestinal tract, it is used orally or rectally. This reduces the risk of side effects, since the active component is not absorbed into the blood and is completely excreted in feces.
Preventive measures to avoid stomach pain
It is easier to prevent a disease than to undergo long-term treatment.
Therefore, the following prevention principles are used:
- frequent hand washing with soap;
- using proper nutrition and avoiding unhealthy foods;
- compliance with the diet, it is not recommended to eat food after 6 pm, motor skills slow down at night;
- eliminating carbonated drinks from the diet, reducing coffee consumption;
- Overeating is not recommended, it puts a strain on digestion and heaviness in the stomach;
- drinking at least 2 liters of water per day;
- reducing the consumption of alcoholic beverages or completely eliminating them, for example, with ulcerative disease, pancreatitis;
- complex treatment of infection with antibiotics and drugs to normalize microflora;
- taking medications only as prescribed by a doctor, excluding self-medication, increasing the dosage or course of therapy;
- drink water from proven sources, do not use liquid from rivers, lakes, or other natural areas;
- timely treatment of abnormal bowel movements to eliminate the risk of severe pathologies;
- complete completion of therapy to prevent residual effects;
- body weight control, absence of excessive overweight or obesity;
- adequate physical activity commensurate with the state of health;
- quitting smoking, nicotine penetrates the respiratory and digestive tract;
- eliminating stress on your own or when contacting a psychotherapist;
- lack of contact with people infected with infections.
Compliance with safety measures will not completely eliminate the risk of pathology. But they will lower it.
Preventive measures are used when you feel normal. If the disease has already formed, they will not help. It will require the use of medications, surgery, and physical therapy.
What does sudden aching pain in the stomach indicate?
When a damaging factor acts on the walls of the stomach, a protective mechanism is activated.
Pain speaks about the processes:
- activation of the immune system, sending a large number of leukocytes to the lesion;
- immune cells release inflammatory mediators (bradykinin, histamine), leading to expansion of the lumen of the vessel with the formation of pain and swelling;
- specific symptoms of dyspeptic disorders occur, characteristic of different types of pathologies;
- if the damage is neutralized, the inflammatory response gradually ceases.
The sudden onset of discomfort occurs for the following reasons:
- exacerbation of a chronic disease;
- intensification of acute illness due to additional factors - poor diet, alcohol consumption, stress;
- the formation of pathology outside the digestive tract, but creating abdominal pain due to the location or passage of a pain impulse along adjacent nerve fibers;
- improper use of medications with the appearance of adverse reactions.
The patient can use the treatment independently, without a doctor's instructions. For example, if he has developed a similar condition before, he knows what to do about it.
If the symptom appears for the first time, the person does not know about the principles of treatment, it is better to consult a doctor. Emergency first aid may be necessary. They call an ambulance.
In a clinical institution, a person is given pain relief and basic medications are prescribed. But specific therapy is carried out after diagnosis.