Bulbitis of the duodenum: symptoms and methods of treatment in adults Few have heard of such a pathological condition as bulbitis of the stomach; they don’t know what it is. Although a disease such as bulbitis is extremely common. In fact, this pathology is just a type of inflammatory changes in the intestines.
Anatomically, in the duodenum there is a bulb into which the stomach directly passes and which can become inflamed separately. Bulbitis as a disease is diverse in morphological and clinical characteristics, but can be successfully treated with timely therapeutic compensation.
Causes
The causes of bulbitis are in many ways similar to the causes of gastritis:
- pharmaceuticals;
- chemical burns;
- love of alcoholic drinks;
- habit of eating too hot food;
- infection with helminths or lamblia (especially typical for children);
- variant of manifestation of Crohn's disease, etc.;
- poor nutrition (eating on the go, addiction to junk food, habit of eating once a day, but a lot, etc.);
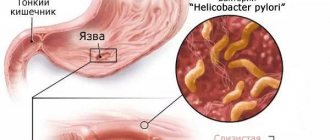
- bacteria Helicobacter pylori (especially in the case of catarrhal form or mixed bulbitis);
- mechanical trauma to an organ (swallowing an indestructible object, which can damage the walls of the organ, often leading to focal damage).
Development of erosive bulbite
The initial section of the intestinal tube is the duodenum. It borders on the pylorus of the stomach. The initial section is called the ampulla.
Duodenal bulbitis is an acute or chronic inflammation of the mucous membrane of this area.
In the erosive form of the disease, ulcerative lesions form. They often lead to intestinal bleeding.
Like erosive gastritis, this pathology occurs in acute and chronic forms.
The disease is caused by:
- Helicobacter pylori infection;
- taking aggressive medications (NSAIDs, antibiotics);
- immune disorders;
- burns;
- surgical interventions;
- poor nutrition;
- smoking;
- alcoholism.
The most common symptoms of the disease are:
- pain in the upper abdomen;
- blood in the stool;
- weakness;
- nausea;
- vomit;
- stool disorder.
With bulbitis, the symptoms are determined by the concomitant pathology and form of the disease.
Local signs
Inflammation of the duodenal bulb is manifested by pain.
It has the following features:
- dull or sharp;
- moderate intensity;
- localized in the epigastric zone;
- combined with nausea and unstable stool;
- occurs immediately after eating and on an empty stomach.
If bleeding develops, the pain syndrome intensifies. All these symptoms resemble erosive gastritis.
If duodenitis is combined with intestinal obstruction, the pain intensifies during heavy meals. In this case, it becomes paroxysmal and bursting.
The chronic form of erosive bulbitis proceeds more calmly. The pain is dull and of moderate intensity.
It may be permanent. The appearance of pain is caused by swelling and damage to the mucous membrane.
If the cause is hyperacid gastritis (inflammation of the stomach), then this symptom occurs 10-20 minutes after eating.
Acute erosive bulbitis also manifests itself as pain. It occurs during palpation of the abdomen.
Classification
Existing types of bulbitis are determined by the causes and nature of the development of the disease itself.
- Surface. With this type, the upper region of the mucosa is affected.
- Focal bulbitis is characterized by the accumulation of ulcerative formations. In this case, treatment is prescribed depending on the severity of the disease itself.
- Erosive. In this case, small ulcers may form on the mucous membrane.
- Hemorrhagic. With this type of bulbitis, inflammation of the mucous membrane, the appearance of erosions and bleeding are noted.
- Atrophic or bulbitis of the duodenum. This esophagitis causes pallor and thinning of the walls of the duodenum.
Symptoms of duodenal bulbitis
Bulbitis in adults is manifested by rather nonspecific symptoms, such as:
- feeling of nausea, bloating in the stomach;
- bitter or metallic taste in the mouth;
- headache and malaise (also with acute inflammation);
- pain in the epigastric region, more on the left, which can radiate to the left hypochondrium or umbilical region;
- rarely - vomiting (in case of acute poisoning or toxic infections, it can be repeated);
- diarrhea or loose stools.
A characteristic symptom of gastric bulbitis is the appearance of pain 1.5-2 hours after eating and at night. These are the so-called “hunger pains”, which decrease after taking milk or antacids. If bulbitis occurs as a manifestation of Crohn's disease, the severity of the symptoms evaluates the degree of activity of the inflammatory process. The following indicators are taken into account:
- frequency of diarrhea,
- intensity of abdominal pain,
- degree of weight loss, etc.
For example, with bulbitis of the 1st degree of activity, the patient’s well-being suffers little: diarrhea occurs 3-4 times a week, pain is minor and intermittent, and there is no weight loss.
Treatment
Treatment of bulbitis is complex and includes:
- medicines;
- therapeutic nutrition;
- herbal medicine.
Surgical intervention is extremely rarely used. As a rule, it is necessary for chronic bulbitis with complications (bulb ulcer, duodenal stenosis) or high activity of Crohn's disease. Also, if a foreign body enters and causes an inflammatory process, it is prescribed to remove it surgically or by duodenoscopy.
Drug therapy
If an infection with the microbe Helicobacter pylori is detected, a combination treatment based on 2-3 antibiotics is prescribed. For superficial bulbitis (acute or chronic type) use:
- blockers of H2-histamine receptors of the stomach;
- antacids;
- proton pump inhibitors.
Such drugs help reduce the negative impact on the duodenal mucosa and reduce the acidity of gastric juice.
Sometimes treatment with hormones, immunoregulators or anthelmintic drugs is required. It depends on the specific type of bulbit.
Medicines must be prescribed by a doctor.
Folk remedies
Traditional medicine will also be effective in treating the inflammatory process. Recipes based on calendula, chamomile, St. John's wort, plantain, yarrow and other medicinal plants that have anti-inflammatory and antimicrobial properties are used. They must be combined with drug therapy prescribed by a doctor and dietary nutrition.
The most common recipes are:
- St. John's wort infusion. 2 tablespoons of the herb are infused in 1 glass of boiling water for 1–2 hours. The resulting product is taken according to? glasses 4 times a day before meals.
St. John's wort infusion is the best remedy for bulbitis, which relieves inflammation
- Plantain juice. 45 milliliters of juice must be mixed with 1 teaspoon of natural honey and take 1 tablespoon of the mixture 3 times a day. Plantain juice can be purchased at a pharmacy.
- Propolis. Fresh high quality propolis (60 grams) should be crushed and poured with 1 glass of alcohol. Leave the resulting mixture for 7 days, then strain. Take by diluting with boiled water: 5 milliliters of infusion per 150 milliliters of water. Drink in small sips half an hour before meals, 2 times a day.
- Carrot juice. To prepare fresh juice, carrots are washed, peeled and grated, then squeezed through cheesecloth. If you have a juicer, use it. Accept according to? glasses 3 times a day 30–40 minutes before meals.
Need to know! The course of treatment with folk remedies lasts 2 weeks, after which a break of one and a half weeks is taken, then the therapy is repeated.
Diagnostics
To confirm gastric bulbitis, the following methods are used:
- X-ray, which allows you to identify changes in the structure of the duodenum and stomach, confirming the existing symptoms. These are signs such as the presence of spasms turning into relaxation, instability of peristalsis, and increased size of the bulb.
- Physical examination by palpation of the abdomen. A possible diagnosis is indicated by the appearance of minor pain in the epigastric region and a tense state of the anterior abdominal wall.
- Daily pH-metry to track the dynamics of acid formation during meals, during a fasting state and in other situations.
- Electrogastroenterography, which makes it possible to detect signs of motor-evacuation abnormalities in the functioning of the stomach and duodenum.
- Duodenoscopy, which can reveal symptoms in the form of swelling and redness of the mucous membrane, its excessive bleeding, erosion areas in the lower part of the stomach and the adjacent part of the intestine. If the cause of the pathology is atrophy of the mucosa, it is possible to detect its pallor and thinning.
- Antroduodenal manometry to determine the pressure during contraction of the stomach during its operation (special sensors are placed in the antrum).
How to diagnose the disease?
Primary diagnosis is carried out using a physical examination. During the period of inflammation of the bulb, by palpation of the abdomen, you can find that the abdominal wall in the peri-umbilical region is slightly tense. During diagnosis, the patient feels mild pain. The specialist also checks the tongue, since when there is bulbitis, a specific yellow coating appears on it.
With bulbitis, the doctor first of all pays attention to the symptoms when palpating the abdomen
The next step is to take blood, urine and stool tests. It is also necessary to undergo an X-ray examination, with the help of which one can detect changes in DNA, as well as uneven and disordered peristalsis, spasms of a certain periodicity, which are replaced by moments of relaxation. You can also detect deformation of the bulb, while it becomes somewhat larger in volume.
Additionally, a bacteriological examination of the contents of the duodenal area is carried out, which makes it possible to verify whether the diagnosis was made correctly. To determine the causative agent of the disease, a bacteriological diagnosis of bile (taken directly from the duodenal bulb) should be carried out.
To identify an ulcer, fibrogastroduodenoscopy is performed
To identify the type of bulbitis, fibrogastroduodenoscopy is performed. Optics will show shiny and smooth walls of the duodenum and stomach if the mucous membrane is in order. The color of the walls is slightly brighter than the color of the esophagus. When air is blown, the folds open freely, and arteries and bluish veins are clearly visible. No reflux is observed. With bulbitis, the walls change in accordance with the specific type of disease.
Diagnosis of erosive bulbitis (video)
Attention! We warn you that the video contains disturbing images!
Drug treatment
Treatment using medications is prescribed only after determining the root cause of duodenal bulbitis. If it is focal and caused by the entry of a foreign object into the duodenum, then it is necessary to remove this object. As a rule, this can be done by duodenoscopy. When Helicobacter pylori infection is detected, combination therapy using antibiotics is prescribed. If the cause of the disease is a parasitic infestation, specialized treatment is carried out, which is prescribed depending on the type of parasite.
Steroid medications may be prescribed for Crohn's disease. Immunoregulators are used to treat follicular bulbitis. Symptomatic treatment helps alleviate the manifestation of the main signs of inflammation. Most often, antacids are used. H2 blockers and proton pump regulators may be used. If stress levels are elevated, sedatives may be prescribed to help relieve nervous tension.
Treatment of erosive bulbitis
If the small intestine is affected, treatment is required. It begins after diagnosis.
The erosive form of bulbitis can be identified during fibroesophagogastroduodenoscopy.
If secondary erosive bulbitis of the duodenum is suspected, the cause must be determined.
In case of acute inflammation, it is necessary to be treated, otherwise this pathology can develop into an ulcer and take a chronic course.
Therapy has the following objectives:
- elimination of symptoms;
- healing of the mucous membrane;
- prevention of complications (bleeding, shock, ulcers).
In some cases, hospitalization is required. This is possible during the period of exacerbation, when the person’s condition is serious and there is bleeding. Most often, patients are treated on an outpatient basis after a medical consultation.
The following components of therapy are known:
- diet;
- taking medications;
- quitting smoking and alcohol;
- physiotherapy.
In advanced cases, surgical intervention is required. Timely and adequate treatment is important to prevent the formation of an ulcer.
In case of bleeding, emergency assistance is required. This may be clipping or coagulation of damaged vessels.
Treatment of erosive bulbitis with drugs
The treatment regimen involves taking medications.
Most often, when erosive bulbitis is detected, the following medications are prescribed:
- antibiotics (macrolides, penicillins, nitroimidazoles);
- proton pump inhibitors;
- antacids;
- prokinetics;
- antispasmodics;
- analgesics;
- enzymes.
Drugs such as M-anticholinergics and histamine receptor blockers are used less and less.
Ulcers and erosion can form against the background of increased production of hydrochloric acid.
Such patients are prescribed proton pump inhibitors. They suppress the formation of gastric juice.
The most commonly used:
- Khairabesol,
- Sanpraz,
- Works, Razo,
- Zulbex,
- Beret, Omez.
They are produced in the form of capsules and tablets. For erosions of the stomach and duodenum, a healing agent is used.
This could be sea buckthorn or rosehip oil. Actovegin is often prescribed.
In case of severe pain syndrome against the background of erosive bulbitis caused by gastritis with increased secretion, antacids are used.
If Helicobacter bacteria are detected in the body, antibiotics are indicated. The most effective are macrolides and penicillins.
In the acute period of the disease, antispasmodics are used. They relax the smooth muscles of the organ, eliminating pain.
In order for food to leave the duodenum faster, prokinetics are used.
These medications normalize the motor function of the stomach and intestines. Many prokinetics have an antiemetic effect.
After eliminating the pain, multienzyme drugs are used. These include Creon 10000.
It normalizes the process of digesting food. Enzymes are indicated only outside the acute stage.
Nutrition rules
Diet is the key to the effectiveness of treatment and the absence of relapses in the patient, so you need to pay special attention to nutrition. In severe advanced cases and in the acute stage, it is better to completely eliminate food intake for a while until pain, swelling and inflammation decrease, and then gradually add porridge with low-fat milk and water.
In the non-acute stage, nutrition for bulbitis includes fermented milk products, vegetable broths, and white bread crackers. All products must be boiled or steamed. The beneficial effects of natural jelly and enveloping cocktails. As a sweet treat, oatmeal cookies are perfect for such patients.
You should forever give up carbonated drinks, spicy and fried foods, and smoked foods. A patient with a predisposition to gastrointestinal diseases should never stop eating properly.
How to treat chronic bulbitis?
For chronic and catarrhal bulbitis, antibacterial therapy is prescribed, since this type of bulbitis develops, as a rule, due to Helicobacter pylori infection. Antibiotics are prescribed taking into account the sensitivity of the pathogen to them. These can be certain groups of antibiotics that act on the cell of the pathogen itself - Amoxicycline, Vilprafen, Summed, De-nol and others. Sometimes Metronidazole can be prescribed, but nowadays its effectiveness among potential “killers” of Helicobacter is disputed.
Also, with this type of bulbitis, a long-term diet is prescribed. In addition, you must stop smoking. Avoid stressful situations whenever possible. It is necessary to stop taking all kinds of food additives; they can also be a provoking factor for the exacerbation of catarrhal and chronic bulbitis. Also, in stressful situations, during the treatment of this type of bulbitis, sedatives and sedatives are prescribed.
You should understand and be psychologically prepared for the fact that you will have to reconsider your usual way of life, since the treatment will be complex and long-term.
Prognosis and prevention
If you seek specialized help in a timely manner, prescribe adequate therapy for bulbitis and eradicate Helicobacter, the prognosis is favorable. Patients must follow dietary therapy recommendations and, if necessary, adjust their lifestyle. You should stop smoking and drinking alcohol.
Prevention of bulbitis involves timely treatment of gastritis with mandatory post-therapy tests confirming the eradication of the pathogen. Even without exacerbations, it is necessary to regularly attend medical examinations. Many drugs are aggressive to the mucous membrane of the stomach and duodenum, therefore, for bulbitis, all drugs should be used only after consultation with a doctor.
To prevent infection with Helicobacter, you should maintain food hygiene and wash your hands thoroughly before eating.