Any manifestation of an attack of this disease causes sharp, unbearable pain, nausea and vomiting. The pancreas, irritated by inflammation, intensively and sharply reduces the quality of life of each patient. Therefore, it is very important to know how to soothe the pancreas at home, how to relieve pain, and what to do if it is not possible to receive emergency qualified medical care.
Causes of pain
Errors in the diet usually lead to this ending: consumption of excessively spicy or fatty foods, and especially those “rich” in preservatives and other harmful food additives such as E630, E631, or prohibited ones (E121, E123), etc.
Alcohol and overeating have a detrimental effect. The situation is aggravated by exposure to stress factors, as well as concomitant diseases of the digestive system.
Pancreatic pain can occur due to food poisoning or as a result of exposure to chemicals or even medications.
According to the mechanism of occurrence, painful attacks can occur with the following pathological changes:
- as a result of narrowing of the gland ducts;
- with insufficient oxygen supply to the organ;
- during degenerative processes in the tissues of the gland;
- with errors in the blood supply to the gland.
Attention! If you experience constant, aching or acute pain in the abdominal area, you should not self-medicate. You should definitely consult a doctor to clarify the diagnosis and treatment. In the case of an incorrectly chosen treatment regimen or lack of treatment, necrosis of pancreatic tissue (pancreatic necrosis) may develop. This threatens the appearance of severe pain, a progressive deterioration of the patient’s general condition, and can have fatal consequences in the future.
How to recognize pancreatic colic
In addition to spasms, a person may be bothered by pancreatic colic. They are quite easily confused with spasms and intestinal colic, but in terms of the degree of manifestation they are more pronounced. They can also lead to real shock and death. Colic develops against the background of acute pancreatitis. In this case, the person complains of tingling in the left hypochondrium or in the pit of the stomach. The severity of colic depends on the severity of the inflammation.
We also recommend viewing: Excretory duct in the area of the parotid gland: meaning, diseases (mumps), treatment
During the formation of pancreatic colic, excessive production of pancreatic juice occurs, as a result of which a person experiences:
- heartburn;
- sour belching;
- diarrhea;
- nausea and vomiting;
- stabbing pains.
The reasons for this condition are:
- Eating large quantities of food at night.
- Presence of fatty foods in the diet.
- Eating spicy food.
- Excessive alcohol consumption.
Important. If the disease is not treated, then sooner or later the walls of the pancreas begin to collapse.
How to relieve pain from pancreatitis
First of all, you need to remember: in this case, the patient should be given complete rest, and he also needs a “starvation” diet.
Sometimes, if only these conditions are met, it is possible to achieve a significant reduction in pain. Also read on our website: We treat pancreatitis at home using folk methods
It is allowed to drink mineral water (alkaline, still). Apply cold (ice pack) to the abdominal area.
Pancreatitis has worsened - the pain can be relieved with painkillers, which are administered by injection; tablet forms are excluded. This is explained by the fact that this pathology is accompanied by nausea and often vomiting, as a result of which the drugs do not have time to be absorbed by the body and do not have the desired effect. Taking enzymes in the acute period is strictly prohibited.
As a rule, painkillers are prescribed by a doctor, and only in complex treatment, which implies:
- restoration of water-salt balance;
- decreased activity and production of pancreatic enzymes;
- suppression of infection.
Important! You should not take painkillers for pancreatitis on your own, without medical advice, because by eliminating the pain syndrome, you will “veil” the symptoms of the disease. This will make it difficult to diagnose.
To the question: is it possible to cure a stomach or duodenal ulcer at home, a gastroenterologist, head of the gastroenterology department, Mikhail Vasilievich Arkhipov, answers.
Groups of drugs that relieve pain in the stomach and pancreas
Several groups of pharmacological drugs are used in therapy. When prescribing the drug, the doctor takes into account the patient’s general condition, the risks of side effects, contraindications, and laboratory test results.
An overdose of pain-relieving drugs produces characteristic symptoms. A person feels nausea and dry mouth, sometimes on the contrary - excess salivation. Vomiting and diarrhea are common.
Medicines for pain in the pancreas and stomach are presented in the following groups:
- enzymatic;
- antienzyme;
- antiulcer;
- antacids;
- antispasmodics;
- analgesics.
Several groups of medications are prescribed simultaneously, which helps reduce muscle tissue tension, eliminate discomfort, and prevent complications.
Before using any tablets, be sure to read the instructions.
Enzymatic
These pills are often used after overeating. Basic properties:
- interfere with the production of pancreatic enzymes;
- improve digestion;
- reduce the load on the pancreas;
- eliminate the feeling of heaviness in the stomach;
- prevent gas formation and flatulence.
Most often prescribed:
- Mezim;
- Micrasim;
- Gastenorm Forte;
- Pancreatin;
- Penzital;
- Festal.
Dissolving in the intestines, these drugs send a signal to the brain that there are enough enzymes for digestion. The brain reduces pancreatic activity and enzyme production. Taking medications reduces pressure in the ducts of the gland, relieves swelling of tissues and prevents destruction of the organ.
It is advisable to use tablets in combination with antacids. Otherwise, their shell of the drug will begin to melt in the stomach, and the therapy will not have the desired effect. It is forbidden to use them before a meal, as this can provoke an attack of pain in the pancreas. Drink either during meals or immediately after. In case of chronic pancreatitis, systematic use is recommended; in the acute course of the disease, it is taken for a course of up to 1 year.
Antienzyme
They are used when it is necessary to stop the production of digestive enzymes by the pancreas and give it rest during inflammation.
This group includes:
- Contrikal;
- Trasylol;
- Gordoks;
- Pantrypin;
- Ingitril;
- Antagozan, etc.
The action of these tablets is aimed at reducing the activity of enzymes that break down protein compounds. Recommended for acute pancreatitis, which is characterized by necrotic processes - tissues literally self-digest. In the chronic form, they are recommended to eliminate swelling of the pancreas and reduce the risk of exacerbation.
It is impossible to purchase these drugs in tablets. Enzyme inhibitors are available in the form of solutions and are administered by drip in a hospital setting.
Antiulcer
Already from the name it is clear that the drugs are prescribed to patients with erosion of the stomach walls. Additional indications for use are the presence of gastritis with high acidity, duodenitis, diaphragmatic hernia, reflux esophagitis. In this case, the tablets are used as a prophylaxis for peptic ulcers.
Basic actions:
- Neutralization of hydrochloric acid.
- Prevention of erosive processes in the stomach.
- Protection of mucous membranes. The drugs increase the formation of mucus, which envelops the walls with a soft layer, preventing them from irritation by the aggressive environment.
- Absorption and removal of harmful compounds.
- Scar healing.
Frequently recommended remedies:
- De Nol;
- Kvamatel;
- Azitral;
- Sanpraz;
- Gelusil, etc.
Many medications in this group contain antibacterial components, so doctors do not prescribe such tablets to women while pregnant, or to young patients.
Antacids
For pain in the stomach and pancreas, these medications help reduce acidity and protect the organ from irritation. Such remedies for heartburn help, relieve pain, and accelerate the restoration of the mucous membrane during erosive processes.
Tablets are selected strictly individually, because pain in the pancreas is caused by various reasons. You should not take medications that have helped your friends.
The tablets contain mineral components – magnesium and aluminum salts, which significantly enhances the effectiveness of therapy. The advantages of treatment include a minimum of contraindications. It is usually prohibited to take antacid tablets if you are hypersensitive and have reduced kidney function.
The following medications are often prescribed:
- Phosphalugel;
- Gaviscon;
- Rennie;
- Rutacid;
- Almagel;
- Enterosgel;
- Maalox.
The therapeutic effect is achieved in a short time, but pain is reduced only for a short period of time. Antacids in tablets are divided into groups:
- Non-absorbable. Medicines do not penetrate into the bloodstream, have a local effect, and practically do not provoke side symptoms. Some tablets perfectly absorb toxins, so they are recommended for food poisoning.
- Absorbable. They penetrate from the intestines into the blood, so they have wider contraindications for use.
Sometimes antacids are combined with other medications. For example:
- Almagel Neo contains simethicone, a substance that prevents increased flatulence. And when acid is neutralized, gas formation always increases, which can cause stomach pain if used incorrectly.
- Gaviscon contains alginates. These components form a film on the contents of the stomach, which prevents the reflux of semi-digested ingredients into the esophagus and prevents the development of heartburn.
- An analgesic is added to Almagel A, so the product is especially effective against pain.
In most cases, these drugs are sold without a prescription.
Antispasmodics
These painkillers are often recommended for treating the stomach and pancreas. Effective drugs:
- No-shpa;
- Spasmomen;
- Papaverine;
- Trimedat;
- Papazol.
Divided into the following groups:
- Neurotropic. Simulation of the work of muscle tissue is achieved by influencing nerve impulses.
- Myotropic. Affect intracellular processes.
Only a doctor can choose truly useful antispasmodics to eliminate pain based on diagnosis.
Analgesics and others
Effective painkillers recommended for pancreatic pathologies:
- Acelizin;
- Analgin;
- Promedol;
- Morphine;
- Omnopon.
These medications reduce irritation of pain receptors. Among them are non-narcotic and narcotic. The use of the latter should be treated with caution, as addiction is possible.
Analgesics are used as a last resort when the use of astringents and tablets that relax muscle tissue and neutralize acidity does not give a positive result.
Pain relief for acute pancreatitis
If the pain is moderate, medications from the group of analgesics (Baralgin, Acetamifene) or antispasmodics (Buscopan, Papaverine, Mebeverine, No-shpa, Platyfillin) are prescribed.
Ketanov is an effective non-narcotic pain reliever. In some cases, novocaine blockades are carried out. If the drugs outlined above are ineffective, narcotic drugs can be used as prescribed by a doctor: Omnopon, Promedol, Tramadol.
Since therapy for acute pathology is carried out in a hospital, the attending physician will prescribe detoxification therapy in the form of intravenous drips, antibacterial agents (usually Ceftriaxone), as well as drugs that reduce pancreatic secretion.
First aid for an attack
The first thing the patient must do is follow three important rules: “Hunger, cold and rest.”
Hunger: you should not eat any foods during an attack, including drinking a lot of water, as this will lead to complications.
Cold: due to the fact that the pain attack intensifies each time, it is necessary to put a cold heating pad in the epigastric region at home.
How to properly place a heating pad? Fill with cold water and place the heating pad in the freezer. Wrap the heating pad in a cloth before placing it on your abdomen.
Some patients think that if the heating pad is placed on the stomach for a long time, then there will be no pain. In fact, cold treatment should not exceed 20 minutes. Note that during these same 20 minutes the patient still needs to take a break.
Also read on our website: Antibiotics for pancreatitis in adults, for acute pancreatitis, for exacerbation of chronic
Benefits of cold treatment:
- Reduces pain.
- Eliminates swelling of the pancreas.
- During cold treatment, inflammation decreases.
If the methods described above do not bring a positive result, then it is necessary to take medications. In case of a severe pain attack, you can take medications from the group of antispasmodics or analgesics.
The most bladeless medicine is “No-shpa”. In order to normalize the flow of bile, it is necessary to take a choleretic drug, for example Allohol.
Now you know how to relieve an attack of pancreatitis at home.
Remember, you should not bring yourself to a burdened state, it is better to call an ambulance. What are they doing in the hospital? Emergency assistance during an attack necessarily includes:
- IV with saline solution, Cerucal.
- Painkillers, for example: Ketorolac, Kvamatel.
If necessary, doctors perform other injections to alleviate the patient's condition. The first action of medical workers in a hospital is to exclude the pancreas from the digestive process.
Therefore, in a hospital, the patient is prescribed fasting for 3-7 days. But this does not mean that during this time you will not eat at all. You will be able to drink water in small quantities.
After 7 days, doctors carry out diet therapy and then cleanse the patient’s body. With severe intoxication, purulent processes can occur, and the level of enzymes in the blood increases.
That's why doctors prescribe Creon and Pancreatin.
If the patient continues to vomit, the drug Metoclopramide is prescribed. Additional medical assistance:
- In the acute phase, Contrical and Gordox are prescribed.
- Intravenous Omeprazole.
- For swelling of the pancreas, Furosemide (Lasix) is prescribed.
To eliminate acidity in the stomach, Famotidine and Cimetidine are prescribed.
Drug pain relief for chronic pancreatitis
Chronic forms of the disease are characterized by less intense pain. This is explained by the fact that the inflammation process occurs in a more erased form. However, the affected pancreatic parenchyma gradually undergoes cicatricial changes. It grows with connective tissue, its coarse fibers compress blood vessels and nerve endings.
Chief gastroenterologist of the Russian Federation: “PANCREATITIS does not go away?! A simple treatment method has already healed hundreds of patients at home! To cure the pancreas forever you need...” Read more »
As a result, the function of the organ is disrupted, all this is accompanied by aching and dull pain in the hypochondrium area. During periods of exacerbation, the pain intensifies, but usually does not reach the intensity as with acute pancreatitis.
Also read on our website: Herbs for pancreatitis of the pancreas
How to relieve pain from pancreatitis if it occurs in a chronic form?
As with acute manifestations of the disease, painkillers are used. In this case, on an outpatient basis, it is allowed to take drugs in tablets as prescribed by a doctor.
In order to relieve pain and alleviate the patient’s condition, the following are used:
- non-steroidal anti-inflammatory drugs: Diclofenac, Nimesil, Ibuprofen, Voltaren;
- antispasmodics and analgesics: No-shpa, Buscopan, Meteospasmil, Trigan, Pentalgin.
In addition to targeted pain relief, medications are used to “unload” the gland. Some of them relieve swelling, others partially restore its functions, thereby participating in the relief of pain. These include:
- proteinase inhibitors: Kontrikal, Gordox, Kontriven;
- Somatostatin drugs (Octreotide), which can suppress the secretory function of the gland;
- enzyme preparations to restore digestion: Mezim, Pancreatin, Festal (not used in the acute period);
- antihistamines: Suprastin, Diphenhydramine, Pipolfen (participate in relieving swelling and inflammation, reduce allergic reactions);
- diuretics: Furosemide, Hypothiazide, Spironolactone (reduce tissue swelling).
Symptoms
Often, clinical manifestations alone may indicate a completely different disease. And the person is in no hurry to see a doctor, but in the meantime the disease progresses, and the person learns about a completely different pathology while already in a hospital bed. If a person complains of pancreatic spasm, the symptoms in this case are:
- cramping pain in the upper part of the stomach;
- nausea and vomiting;
- violation of stool, calla stool acquires a liquid structure;
- diarrhea;
- a sharp increase in body temperature.
We also recommend viewing: Is it possible to cure the pancreas with the help of marigolds: benefits of the plant and application
Vomiting usually worsens as pain increases. The higher they are, the more often vomiting occurs. Symptoms worsen with any human movement and subside slightly when the person is immobilized.
Other methods of pain relief for pancreatitis
What methods and techniques exist to relieve pain from pancreatitis? The mechanism of pain occurrence plays an important role here.
If obstruction of the gland ducts predominates, the following surgical procedures will be effective to restore the patency of its ducts:
- stenting of the gland duct: allows you to “straighten” its lumen, which relieves pain;
- lithoextraction: surgical removal of common bile duct (glandular duct) stones;
- intraductal lithotripsy: laparoscopic surgery during which the ducts of the gland are dilated mechanically.
If the disease is autoimmune in nature, the analgesic effect will be achieved by using duct stenting, taking corticosteroids and ursodeoxycholic acid drugs (Ursosan, Ursoliv, Ursodex).
If a patient has biliary pancreatitis associated with disturbances in the outflow of bile, inflammation of the gland and the formation of stones in its ducts, then ursodeoxycholic acid preparations, increased dosages of pancreatic enzymes, and the use of antispasmodics will be quite effective.
Also read on our website: Symptoms, treatment recommendations and medications for acute pancreatitis
Does your pancreas really hurt?
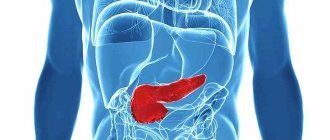
Before taking any measures to eliminate an attack, you need to know exactly how the pancreas hurts, because the symptoms that arise from its inflammation also often appear in diseases of other internal organs. The pancreas in humans is located behind the stomach. It has several sections - the tail, head and body.
The body of the pancreas is located directly behind the stomach, the tail is on the left side of the abdominal cavity, near the spleen, and the head is located on the right side and covers the duodenum. Considering that all these parts of the gland are closely adjacent to other organs, when they are inflamed, a person may think that it is the pancreas that is hurting, but in reality this may not be the case.
If the pancreas hurts, a person experiences acute pain that is girdling in nature. At the same time, other symptoms characteristic of pancreatitis appear. Namely:
- nausea, which often provokes vomiting;
- a feeling of bitterness in the mouth, which indicates a violation of the outflow of bile from the duodenum (the work of this organ is closely related to the pancreas, and when it becomes inflamed, its functionality is also impaired);
- bowel dysfunction;
- paleness of the skin;
- weakness;
- increase in temperature (if this symptom occurs, then this already indicates a complicated course of the disease);
- cardiopalmus.
Inflammation of the pancreas causes pain
In this case, painful sensations can occur in various parts of the abdomen, depending on which part of the organ is inflamed. As a rule, when the tail of the pancreas is affected, the pain is localized in the left hypochondrium, and if the head is inflamed, in the right hypochondrium. When the body of the gland is affected, there may be a feeling that the stomach hurts, but in this case they can radiate to the lumbar region or sternum.
If a person experiences pain in the upper abdomen, radiating to the back, the intensity of which does not depend on food intake, then this indicates the development of inflammatory processes in the gland, accompanied by severe swelling of the organ, damage to the nerve endings and increased pressure inside the pancreas.
If painful sensations occur in the right or left upper abdomen, radiating to the lumbar region, which become less pronounced when bending forward, this already indicates the development of pancreatic neuritis. And in cases where the pain is supplemented by attacks of nausea and vomiting, after which the patient does not experience any relief, this already indicates increased pressure in the pancreas, which occurs against the background of the formation of cystic formations in the organ.
Before taking any medications to relieve pain, you must first establish the cause of its occurrence. After all, if the negative factor is eliminated, it will be much easier to overcome pain in the pancreas.
This organ can become ill not only due to the development of inflammatory processes in it, but also against the background of:
- modifications of the gland;
- an increase in pressure in it;
- fibrotic changes affecting sensory nerves;
- formation of cystic formations or cancer in the tissues of the gland;
- ischemia;
- modifications of nearby organs, increasing their size.
The cause of pain in the pancreas and the development of diseases of the digestive system in 80% of cases is poor diet and alcohol abuse.
Since there are many reasons for the occurrence of pain in the pancreas, it is necessary to first establish the exact factors that provoked their occurrence. Without this, it is impossible to carry out any treatment, since inadequate measures can only aggravate the development of pathological processes.