When the conductive function of the esophagus is disrupted, very serious consequences occur, as with cardiospasm and achalasia of the esophagus. Food remains are retained, provoking inflammatory reactions and intoxication. Chronic starvation syndrome is formed, which leads to disruption of all types of metabolism, and therefore to disruption of the functions of all systems and organs. In addition, constant pain, dysphagia and regurgitation have a negative effect on the patient’s psyche.
ICD 10 code K22.
What is esophageal cardiospasm and its causes?
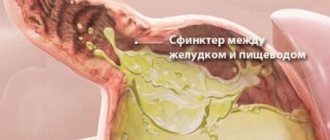
Cardiospasm of the esophagus is a persistent contraction of the muscles of the terminal (end) part of the organ, occurring against the background of dysfunction of the central parts of the parasympathetic ANS (autonomic nervous system) and accompanied by a morphological restructuring of its proximal (upper) parts.
Histological examination reveals abnormalities in the neurons of the dorsal nuclei n. Vagus, as a result, the smooth muscles of the lower sphincter become more sensitive to the tonic action of gastrin. This is a hormone and natural mediator released when the stomach is stimulated by food, its smell or sight. As a result, the distal esophagus is constantly under the influence of tonic impulses. A true spasm of the cardia develops.
The causes and mechanisms of development of the disease are not entirely clear. Now most authors adhere to the following theories of the occurrence of the disease:
- The theory of genetic mutations is the most popular. Mutations lead to insufficiency of certain enzymatic systems (NO synthetase), as a result of which the physiology of smooth muscle contractions is disrupted.
- The theory of autoimmune lesions. This theory is confirmed by the fact that antibodies that can provoke cardiospasm are detected in the blood of patients.
- The theory of viral infection. The role of viral infection with the Herpes Zoster virus (herpes zoster virus) in the development of ANS damage and the occurrence of cardiospasm is discussed.
Causes of pathology
Physiological causes of the disease may be developmental disorders that arise before the birth of the fetus. Congenital malformations of the esophagus occur during embryonic development and subsequently lead to various changes in the structure of its walls. The physiological causes of achalasia are divided into external and internal.
Internal factors include:
- neoplasms;
- esophageal injuries;
- toxic effects of smoking and alcohol;
- prolonged spasms of the cardia.
The same reasons include stenosis of the esophagus, caused by its damage due to infectious diseases.
External factors mean contributing influence from other organs and systems. These factors include the following diseases:
- sclerosis of the esophagus with adhesions;
- hepato- and splenomegaly;
- gastritis;
- peritonitis;
- aerophagia;
- gastroptosis;
- mediastinitis;
- aortic aneurysm;
- aortitis;
- pleurisy.
Contributing factors that can cause dilation of the esophageal tube are neurotrophic disorders and endocrine dysfunction. In addition, it is possible that allergies cause changes in the functioning of the neuromuscular apparatus of the esophagus.
Symptoms in adults
Achalasia and cardiospasm of the esophagus, symptoms, treatment, types of operations - all these issues have been developed in detail by the Russian gastroenterological school (Petrovsky B.V., Vasilenko V.Kh.).
When diagnosed with esophageal cardiospasm, the symptoms are as follows:
- swallowing disorder;
- thoracalgia – pain in the chest area;
- regurgitation - reflux of gastric contents into the esophagus.
The disease usually develops gradually; there are cases of acute onset, when signs of dysphagia appear at the height of severe emotional stress.
The clinic of swallowing disorder with cardiospasm has characteristic features.
Dysphagia is not constant, it occurs:
- under emotional stress;
- when swallowing solid food;
- when swallowing foods containing large amounts of fiber;
- with fast eating and insufficient chewing of food.
Sometimes paradoxical dysphagia occurs, when it is difficult to swallow liquid food, but solid food is swallowed well.
Thoracalgia occurs more often in the retrosternal region (behind the sternum), after eating. This is the result of stretching the walls of the esophagus. The pain may worsen on an empty stomach, which is associated with inflammation in the esophagus. Sometimes thoracalgia is not related to the act of swallowing, but occurs during physical activity or excitement.
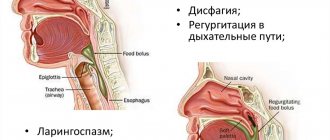
A characteristic symptom of cardiospasm is regurgitation. Active regurgitation is more characteristic of the initial stages of the disease, when emptying of the esophagus occurs immediately after eating. With severe dilatation of the esophagus, regurgitation is delayed, but of a much larger volume. Passive regurgitation occurs independently of food intake - when bending over or in a horizontal state.
Most patients experience noticeable weight loss, and some, with severe disease, experience cachexia - an extreme degree of exhaustion.
Symptoms of the disease
Diagnosis of the disease is not difficult, since the pathology is usually accompanied by severe symptoms. It is based on a survey of the patient and the collected medical history, as well as esophagoscopy and radiography.
Dysphagia is one of the very first and most striking signs of cardiospasm. In the initial stages of the disease, minor difficulties arise with swallowing a bolus of food when it lingers at chest level for a few seconds.
As the disease progresses, the symptoms of dysphagia will intensify and gradually transform into the “cardiospasm triad.” The main elements of this complex of symptoms are: regurgitation, chest discomfort and pain, dysphagia. Without adequate treatment, the pathological process will worsen, food will stagnate in the esophagus, causing it to stretch and the formation of putrefactive fermentation processes.
The long course of the disease leads to the fact that the patient, unable to swallow food, regurgitates it. He develops anemia and underweight. The patient’s psychological state causes difficulties at work and at home.
Achalasia is conventionally divided into three forms: complicated, decompensated, compensated. There are no changes in the tissue of the esophagus during the disease, or there is hypertrophy of the muscular wall of the organ.
Patients complain about:
- discomfort and pain in the chest while eating;
- difficulties with swallowing;
- occasionally – pain outside of meals. In this case, it is difficult to distinguish them from heart pain due to angina pectoris.
An important diagnostic sign of cardiospasm is the inconstancy of dysphagia, this makes it possible to differentiate the disease from oncology and esophageal strictures. The disease has a long course, the symptoms are variable (sometimes subsides almost completely, sometimes suddenly intensifies). Secondary cardiospasm disappears after the disease that caused it is cured.
Stages of the disease
There are many different classifications of cardiospasm, but the classification of Academician B.V. remains generally accepted. Petrovsky, who distinguished 4 stages in the disease.
Cardiospasm of the esophagus: stages according to B.V. Petrovsky:
- I – stage of intermittent, functional spasm of the cardia, no signs of esophageal dilatation;
- II – stage, when the spasm of the cardia becomes stable, a slight dilation of the esophagus;
- III – stage, at which the muscle layers of the cadia are scarred, the esophagus expands significantly;
- IV – stage, stenosis of the cardia is pronounced, with significant lengthening, expansion, and deformation of the esophageal tube.
Pathological picture
An expansion and change in the esophagus is noted, as a result of which it can take an S-shape. The distal area is sharply narrowed; degeneration of cells of the Auerbach and Meissner plexuses and fibers of the intramural nerve plexuses is found in it. The muscle layer in the early stages of the disease is thickened, later the connective tissue grows, especially in the wall of the lower esophageal sphincter. Signs of an inflammatory process are found in all layers of the wall and in surrounding tissues. The mucous membrane of the esophagus is hyperemic, swollen, ulcerated in places, the changes are more pronounced near the narrowed area of the esophagus.
Diagnostics
Laboratory tests do not play a significant role in the diagnosis.
Basically, the diagnosis of the disease is based on x-ray, endoscopic studies and manometry.
- X-ray with contrast of the esophagus. The main radiological sign is a cone-shaped narrowing of the esophagus with the apex in the region of the cardia, the overlying parts of the organ are dilated, sometimes significantly, the peristalsis of the organ is impaired, and there is no gas bubble in the stomach.
- An endoscopic examination allows one to determine how dilated the upper parts of the esophagus are and the severity of inflammatory and metaplastic changes. Although the cardiac sphincter is closed, in case of cardiospasm it is usually possible to enter the stomach during endoscopy; if the fiberscope does not pass into the stomach, then it is necessary to exclude oncological pathology.
- Manometry can confirm the diagnosis. The main manometric syndrome is the absence or decreased relaxation of the LES during swallowing. The study reveals an increase in pressure in the area of the lower sphincter and impaired peristalsis.
Drug treatment
At an early stage, the disease can be treated with medication. The treatment is carried out comprehensively, it includes several groups of drugs with different spectrums of action.
The first group of medications is aimed at relaxing the muscles in the lower esophagus. This group of medicines includes:
- Isosorbitol;
- Dinitrate;
- Nitroglycerine.
Relaxing the muscles will ease the spasm and make it easier for food to pass through.
The group of myotropic antispasmodics includes:
- Papaverine;
- Halidor;
- Drotaverine.
These drugs reduce pain caused by muscle spasms.
The medication regimen and dosage are developed by the attending physician. The therapeutic course is planned taking into account the stage of the disease, its severity and the individual characteristics of the patient.
In order to speed up recovery, restorative therapy is necessary. In order to strengthen the body and immune system, the following should be included in the course of treatment:
- B vitamins;
- vitamin C;
- glucose solution.
Treatment should be accompanied by a gentle diet. The tablets are selected in such a way that if they get stuck in the esophagus, they do not irritate the mucous tissues. In some cases, the medicine is administered into the body by injection.
Cardiospasm and achalasia of the esophagus: differences
Cardiospasm and achalasia of the esophagus are two different nosologies. Esophageal achalasia is a disease characterized by persistent loss of the LES relaxation reflex in response to the act of swallowing. Motility of the esophagus is sharply reduced. The cardiac sphincter expands only under the influence of the gravity of swallowed food and liquid. Histologically, a disorder is detected only in postganglionic neurons. Since the central sections of the ANS are not changed, increased sensitivity to gastrin is not observed.
Cardiospasm and achalasia of the esophagus, their differences are that these diseases affect different levels of the parasympathetic ANS.
Treatment of achalasia
Treatment of cardiospasm depends on its degree. As long as scar tissue has not formed in the wall of the esophagus, conservative therapy is possible. The following medications are prescribed:
- nitroglycerin preparations (cause relaxation of smooth muscles not only in blood vessels, but also in internal organs);
- sedatives (to normalize nervous regulation and eliminate stress);
- prokinetics (promote normal motility of the digestive tract);
- calcium antagonists (relieve muscle spasms);
- enveloping drugs (to protect the mucous membrane from inflammation).
For achalasia cardia, treatment is often carried out with botulinum toxin. Small doses of this nerve poison are injected into the wall of the esophagus at the site of narrowing. After some time, the effect of the drug wears off, and the procedure is repeated again.
Minimally invasive interventions
When there are clear signs of cardiospasm, balloon cardiodilation is sometimes used. A special balloon is placed through the mouth into the opening of the esophagus and air is pumped into it to stretch the sphincter. The procedure is carried out several times with an interval of 3-4 days until the desired result is obtained.
Treatment regimen for cardiospasm using a pneumodilator
Another minimally invasive treatment for achalasia is the installation of an absorbable esophageal stent. It is a mesh tube that is inserted into the lumen of the cardiac region and does not allow it to close. Such devices have anti-reflux valves that prevent the backflow of stomach contents.
Surgery
For stage 3-4 achalasia cardia, an operation is performed, the essence of which is to cut the mucous membrane and intersect the muscle fibers of the esophageal wall.
Traditional treatment
To normalize the tone and motility of the esophagus, general strengthening agents are used: tincture of ginseng, eleutherococcus, Rhodiola rosea extract, etc. To reduce the neurological component of pathogenesis, plants with sedative properties are used. This is a tincture and decoction of motherwort and valerian.
In order to eliminate inflammation in the esophagus, it is useful to drink a decoction of chamomile, calendula, infusion of St. John's wort and other anti-inflammatory and antibacterial herbs.
Important: for achalasia cardia, treatment with folk remedies is predominantly auxiliary. Therefore, you should not completely rely on them, ignoring your doctor’s recommendations.
Cardiospasm of the esophagus: treatment
Conservative treatment is ineffective for cardiospasm, but patients are often prescribed: nitrates (nitroglycerin), calcium antagonists (nifedipine), antispasmodics (no-spa), prokinetics (domperidone). These drugs are not able to cure this pathology. But in stages I-II of the disease, nitroglycerin can temporarily relieve cardiospasm.
For what types of cardiospasm is surgical treatment indicated?
The indication for surgical intervention is a narrowing of the cardia with an S-shaped elongation of the esophagus.
The operation is carried out:
- if it is not possible to perform cardiodilation (especially in pediatrics);
- in the absence of results from repeated courses of cardiodilation;
- with rupture of the esophagus caused by cardiodilation.
Balloon dilatation
Drug therapy for cardiospasm is rarely successful. The main method of treating cardiospasm is balloon dilatation. The operation is performed using a soft probe with a balloon at the end. Balloon dilatation is a forced stretching of the lower esophagus with partial rupture of its muscle tissue.
After anesthesia, under X-ray or endoscopic control, a probe is inserted into the esophagus, the balloon is inflated with air to a certain level, and the exposure of the procedure is determined individually. In most cases, after such manipulation, the act of swallowing in patients becomes easier.
Surgery
If there are no results from conservative treatment and bougienage, patients are prescribed surgical treatment.
Currently, laparoscopic myotomies are used. In the terminal stage, extirpation or subtotal resection of the esophagus is performed.
Recovery period after surgery
After the operation, the patient is placed in the intensive care unit, where he is constantly monitored throughout the day. The patient is prescribed a complex of sedative, restorative and analgesic therapy. Diet therapy is being developed. In case of uncomplicated course of the disease, after a few days the patient is transferred to the ward mode. In order to prevent complications, early physical activity is practiced: the patient sits in bed, gets up, and walks around the ward. Here it is important to provide the patient with good care, including proper nutrition, hygiene standards, and psychological peace.
After discharge from the hospital, the patient is sent to outpatient treatment. He is supervised by a gastroenterologist for a year. It is mandatory to regularly examine the surgeon.
A person with esophageal cardiospasm must follow dietary and lifestyle recommendations for the rest of his life, otherwise the consequences can be very unpleasant.
Treatment
Treatment methods depend on the stage of the disease: in the initial period, conservative treatment will be effective; advanced cardiospasm requires surgical intervention.
Conservative methods
Non-operative therapy includes general strengthening measures, organization of a diet, and drug treatment.
Psychotherapy
Patients must be convinced that their illness can be cured, comfortable nutritional conditions must be created, and the consequences of the nervous shock that caused the disease must be removed. Methods of suggestion and hypnosis will help restore emotional and mental health. Excessive physical activity and nervous tension are contraindicated.
Diet therapy
For spastic pathologies of the esophagus, small, frequent meals are necessary (4-5 times a day). It is served pureed and should be consumed slowly, chewing each portion thoroughly before sipping. Diets No. 1, 1a, 1b are recommended. It is necessary to exclude sour, spicy foods, dishes that provoke dysphagia.
There are rules to facilitate the passage of food into the stomach:
- after eating you need to drink a glass of liquid in one gulp;
- After eating, you need to strongly bend your chest and neck back, this helps straighten the esophagus and increase pressure on the cardiac valve. Dinner should be no later than 3-4 hours before bedtime, otherwise food will linger for a long time in the upper gastrointestinal tract and begin to ferment and decompose in it.
Medications
Medications for cardiospasm include drugs with various therapeutic effects:
- antispasmodics (Nitroglycerin, Amylnitrite) are taken before meals, which facilitates the passage of food into the stomach. Relaxation of the cardiac sphincter is facilitated by Papaverine, No-shpa, and belladonna preparations;
Important! Taking antispasmodics is justified in the initial period of the disease; in the later stages they inhibit esophageal peristalsis and can completely stop the movement of food.
- calcium antagonists (Nifedipine, Verapamil) relieve attacks of dysphagia;
- antacids (Maalox, Phosphalugel) are indicated for gastritis with high acidity, which provokes spasms of the esophagus;
- Atropine relieves gastrointestinal spasms well, but has an undesirable side effect on the central nervous system: it depresses consciousness, causes anxiety or drowsiness;
- enhanced vitamin therapy is necessary in advanced stages of the disease; to improve well-being, take B vitamins, which strengthen the nervous system.
Cardiospasm of the esophagus in children
In children, as in adults, the basis of the pathological process is the spastic contraction of the LES and an increase in the diameter of the proximal parts of the organ. This disrupts the tone and motility of the esophagus. In children, organic stenosis and hypertrophy of the muscles of the abdominal esophagus are not detected.
Causes
Histological studies in children with cardiospasm reveal a congenital deficiency of intermuscular neurons, resulting in congenital denervation of the smooth muscle fibers of the esophagus.
Cardiospasm of the esophagus: treatment in children
Children of any age are affected, including infants, but the majority of patients are preschoolers. The disease develops gradually, but with a clear tendency towards chronicity.
Cardiospasm of the esophagus, the symptoms of which are pronounced, is diagnosed quite easily.
The clinical picture of the disease in children is dominated by two symptoms: dysphagia and regurgitation.
Regurgitation is not detected after every feeding. This is vomiting of food eaten without any admixture of gastric juice, or vomiting of mucus.
Dysphagia in infancy and toddlerhood is determined by a number of indirect signs: the baby refuses the breast, chews food for a long time, and often resorts to washing down food with water.
How to treat cardiospasm of the esophagus in children
The main methods of treatment in pediatrics are: cardiodilation and surgical treatment. Medications are ineffective. Pediatric cardiospasm surgery has been thoroughly developed. During surgical treatment, cardiomyotomy according to Geller or diaphragmocardioplasty according to Petrovsky is most often performed.
The results, both immediate and long-term, for children are good. The symptoms of the disease pass, but it is not possible to completely cure; the esophagus, as a rule, remains dilated.
The disease is very serious, entailing not only somatic, but also mental disorders, therefore esophageal cardiospasm, symptoms, treatment are priority areas of global pediatrics.
Causes of cardiospasm
The exact causes of the disease are still unknown. It is believed that the following factors play a significant role in the development of achalasia of the esophageal cardia:
- neurological disorders (psycho-emotional stress, mental disorders);
- dystrophic changes in the nerve fibers and Auerbach plexuses of the esophagus, regulating its tone and motility.
As a result of the action of these factors, the muscle fibers of the esophageal wall contract chaotically and cannot ensure the normal movement of food into the stomach. This pathology is facilitated by increased tone of the cardiac region. You can learn more about the essence of the disease and its pathogenesis from the video at the end of the article.
Preventive measures for cardiodilation
Dilation of the left atrium, right atrium, left and right ventricles, and aortic walls can appear from birth (congenital form) or during life (acquired form). Therefore, the general recommendations of doctors look like this:
- Give up bad habits: smoking, alcohol abuse and use of narcotic (psychotropic) substances.
- Follow your daily routine, eat right, eat enough fresh fruits and vegetables that contain a lot of useful vitamins and microelements, don’t overdo it. Nutrition should be moderate, but at the same time complete.
- Try to do everything to remove yourself from stress, negative emotions and significant physical activity. But this does not mean that physical exercise is prohibited. On the recommendation of the attending physician, light loads are permissible.
Left Atrial Dilatation and Surgery
This is important! If you follow these simple recommendations, you will be able to reduce the number of complications of cardiac pathology and the severity of the disease.