Classification of pancreatic cysts
All cysts that form on the pancreas can be classified according to two main criteria - by their structure and by location on the organ. These signs are recommended to be taken into account in clinical guidelines for surgery.
So, according to their structure, cysts are divided into:
- False formations, that is, those that began to form after any disease. These cysts do not have a glandular epithelial layer in the structure of their walls.
- True formations, that is, those that began to form during intrauterine development. These cysts have an epithelial layer, but they are found very rarely.
Based on the location of the formation on the organ, we can distinguish:
- On the body of the organ. These cysts are the most common. When they form, the position of the stomach and colon is disrupted. Prevalence percentage – 47.
- On the tail of the organ. Tail cysts are somewhat less common than body cysts. When this cyst forms, the organs surrounding the pancreas are not affected. The prevalence rate is 38.2.
- On the head of the organ, located in the cavity of the omental bursa. This is the rarest localization of formation. In this case, compression of the duodenum may occur. The percentage of prevalence is 16.8 (according to Professor G.D. Vilyavin).
Due to the fact that a true cyst is an extremely rare phenomenon, and its symptoms and treatment tactics are not much different from the symptoms and therapeutic regimen for false cysts, it is the latter formations that will be discussed further.
Traditional treatment methods
Treatment of the pancreas is possible using traditional methods of treatment.
Using Herbs
- When treating a disease, the following remedy gives an excellent effect: combine celandine, calendula and yarrow in equal quantities. 1 tsp. collection, brew 200 ml of boiling water. Leave for 2 hours. The recommended dose of the product with celandine is 50 ml before meals. The duration of therapy is thirty days. Then you need to take a two-week break. After this, you should resume treatment by preparing some other medicine. For example, you can make an infusion of plantain arrows (two parts), calendula (two parts) and tansy (one part). Take 1 tsp. collection, pour one glass of boiling water. Leave for 2 hours. You need to take 50 ml of this product before eating. These preparations must be drunk for at least four months.
- Another very useful herb for cysts in the pancreas is sedum. It's easy to use. The leaves of the plant must be cut into salads or added to dishes as greens. You can even just eat two leaves of this plant every day.
- A collection of lingonberry leaves, strawberry leaves, blueberry leaves, bean pods and corn silk helps to cope with the inflammatory process in the gland. 1 tbsp. l. Brew the mixture with 200 ml of boiling water. Leave overnight. Drink 1 tbsp. l. a couple of times a day. Duration of therapy is two weeks. Then a break is taken for seven days.
- For cysts, you can use a collection that has regenerative, antispasmodic and anti-inflammatory effects. Combine plantain, dried cucumber, mint, chamomile, yarrow and St. John's wort in equal quantities. 1 tbsp. l. collection, pour 250 ml of boiling water. Leave for 30 minutes. The recommended dose is 1/3 cup three times a day. The duration of treatment is three weeks. For frequent exacerbations of the disease, a course of therapy is recommended twice a year. If the disease occurs in a chronic form and is accompanied by frequent pain, repeat cyst on the pancreas, treatment with folk remedies is necessary once every two months.
Causes and predisposing factors
A person's age is not a risk factor for cyst formation. They can have different shapes and sizes, and when they are congenital in origin, systemic polycystic disease is often detected. That is, formations are present in the brain, on the ovaries, in the liver and kidneys.
A false cyst develops only on a diseased organ. A healthy pancreas cannot suffer from it, since it is the result of some disease.
Anatoly Alekseevich Kurygin pointed out that the most common reasons leading to the development of cysts are:
- 84.3% of cysts are formed during exacerbation of pancreatitis;
- 14% of cysts develop against the background of an organ injury;
- Blockage of the excretory duct, as well as a significant deterioration in its motility, can cause the formation of cysts;
- Infection with helminths, namely with chronic biohelminthiasis (cysticercosis or echinococcosis);
- Organ tumors.
In addition, several factors leading to the formation of pancreatic cysts have been identified and proven in percentage terms (according to the Russian Surgical Society):
- 62.3% - frequent consumption of strong alcoholic drinks;
- 32.1% - lipid metabolism disorders leading to obesity (diagnostic criterion - increased levels of cholesterol and beta fractions of lipids);
- 15.3% - diabetes mellitus, most often type 2;
- 14% - existing cholelithiasis;
- Previously performed operations on the gastrointestinal tract (not necessarily on the pancreas).
If a patient has clinical signs of damage to the pancreas against the background of one or more risk factors, then it makes sense to suspect a cystic formation.
Drug therapy for the disease
Conservative treatment of pancreatic cysts is possible only in cases where the formation is benign, has clear boundaries and dimensions of no more than 20 mm, and proceeds without complications. Medication therapy is combined with dietary nutrition. For the first 10 days, the patient is prescribed bed rest. For 45 days, the patient is under the supervision of a doctor and regularly undergoes ultrasound.
The following groups of drugs are prescribed for the treatment of pathology:
- analgesics: Baralgin, Trigan-D, Acetaminophen, Pentalgin;
- antispasmodics: No-shpa, Riabal, Papaverine, Bellastesin, Duspatalin, Meteospasmil;
- cephalosporin and tetracycline antibiotics (to prevent infection);
- medications to reduce secretion: Omez, Rabeprazole, Omeprazole;
- medicines for nausea and vomiting: Cerucal, Motilium;
- anti-flatulence drugs: Pankreoflat, Simethicone, Espumisan, Disflatil;
- enzymes for digesting carbohydrates: Creon, Pancreatin, Festal, Mezim.
The diet for pancreatic cysts is based on the same nutritional principles as for acute pancreatitis. Limit fatty and spicy foods, foods containing fiber, and sour foods. Alcohol and products that cause increased gas formation (baked goods, confectionery, carbonated water) are completely excluded. At the same time, proteins and carbohydrates are not limited. Food should be taken often, but in small portions.
The following types of dishes are recommended for the patient:
- soups with vegetable broth, pureed soups made from lean meat;
- low-fat boiled and jellied fish;
- dietary types of boiled meat (beef, rabbit, turkey and skinless chicken);
- omelet, boiled eggs;
- cereal porridge;
- boiled pasta;
- boiled and baked vegetables without coarse fiber;
- low-fat dairy and fermented milk products;
- rosehip decoction, diluted juices, weak tea.
For a cyst on the pancreas, treatment with folk remedies is permissible only after consultation with your doctor. Such therapy can complement medication and diet. The following decoctions and infusions of herbs can be used:
- anti-inflammatory: chamomile, immortelle, St. John's wort, yarrow;
- restorative: plantain, aloe, cudweed, elecampane;
- antispasmodic: oregano, valerian, mint, fennel.
If conservative treatment methods do not produce results within a month, then surgical interventions have to be resorted to.
Important information: What healthy and unhealthy foods the pancreas does not like
Symptoms of a pancreatic cyst
The fact that a patient has a cyst can be suspected by the following characteristic signs:
- An attack of acute pancreatitis, which is expressed in pain of a girdle nature (they occur less frequently in the epigastric region). Increased pain occurs after drinking alcohol or after eating. At the same time, NSAIDs and antispasmodics are not able to relieve pain. At the same time, the patient suffers from vomiting, diarrhea, flatulence and bloating. The stool becomes greasy as lipase secretion is impaired.
- After a month or 5 weeks, the symptoms of acute pancreatitis disappear. This is the so-called “light period”.
- Relapse of the disease. Moreover, each next attack becomes more pronounced and prolonged.
In parallel, the patient may complain of:
- Increase in body temperature to subfebrile levels;
- The appearance of heaviness in the area of the left hypochondrium;
- The appearance of general weakness;
- Formation of jaundice with staining of the mucous membranes and sclera (observed in 6% of cases).
A cyst can cause disruption of hormonal secretion (glucagon, insulin, somatostatin), which is expressed by:
- Constantly thirsty due to dry mouth;
- Loss of consciousness due to the development of hyper or hypoglycemic coma;
- When urination increases, the patient can produce up to 15 liters of urine per day.
Based on visual and palpation examination, the doctor may suspect a cyst, since a protrusion of the abdominal wall may be detected in the area under the sternum. However, this symptom is characteristic of a cyst, which is located on the head of the organ, and its volume reaches 200 ml. However, according to Kurygin, this sign can be detected in 56% of patients.
Symptoms
The presence of the disease can be manifested by the following symptoms:
- Tumor-like compactions appear in the abdominal cavity.
- There is pain in the upper abdomen.
- Vomiting and nausea appear.
- Disturbances in the functioning of the digestive tract appear.
- Body temperature often rises.
- A number of signs of decreased appetite.
- General weakness appears.
These are the main pancreatic cyst symptoms treatment.
Diagnosis of pancreatic cyst
Ultrasound is the standard method for examining the pancreas, including for the detection of cysts. If the patient has a cyst, then on the screen the diagnostician will see an object with a rounded shape, which has reduced echogenicity, that is, it will look like a light spot against the background of a dark organ. The restriction in the form of a smooth contour most often represents a cystic wall. If there are no formations on the organ, then the pancreas is visualized as a dark (echoic) spot with a bumpy surface. There will be no bumps at the site of the localization of the formation, since they are smoothed out.
If for some reason an ultrasound cannot be performed, the patient may be sent for a CT scan or MRI. X-ray examination will not provide information about the cyst.
As for laboratory tests, a cyst may be indirectly indicated by a prolonged increase in amylase in the blood, which can be determined based on a biochemical blood test.
Diagnostics
Pathology in the digestive tract can be detected by chance if it does not cause concern and is congenital. In case of typical complaints, you should contact a specialist.
Visual inspection
Imaging diagnoses a cyst if it has reached a large size. An experienced doctor can identify a protrusion at the location of the formation. An asymmetric abdomen indicates the possible presence of a pancreatic cyst and fistulas in the pancreas.
An asymmetric abdomen indicates the possible presence of a pancreatic cyst and fistulas in the pancreas.
Laboratory examination
It is not possible to detect specific changes in urine and stool tests. A slight increase in leukocytes, red blood cells and other blood parameters does not directly indicate the cause of poor health and a cystic tumor.
Instrumental methods
Highly informative instrumental examinations associated with cyst complications reveal comprehensive information about the size, location, local connections through ultrasound, magnetic resonance imaging (MRI).
Conservative treatment of pancreatic cysts
You can get rid of the formation without surgery under the following conditions:
- The volume of growth does not exceed 20 mm.
- Single cyst.
- Education has clear limitations.
- There is no obstructive jaundice.
- The patient does not suffer from severe pain.
For the first 3 days, the patient must adhere to a fasting diet. Next, the diet should be as gentle as possible. Everything salty and fatty, as well as fried, is excluded from it. This will reduce the enzyme secretion of the organ, which stimulates the destruction of gland tissue. Bed rest must be adhered to for a week (up to 10 days). Smoking and drinking alcoholic beverages is prohibited during this time.
To exclude the possibility of suppuration of the cyst and penetration of a bacterial infection into the peritoneal cavity, the patient is prescribed a course of antibiotics. If this is not done, then the bacterial process that has begun can spread not only throughout the gland, but also through nearby organs. For cysts, drugs from a number of cephalosporins and tetracyclines are prescribed.
To prevent the patient from suffering from severe pain, he may be recommended to take drugs - proton pump inhibitors. Among these are Rabeprazole, Omeprazole, Omez, etc.
Enzyme therapy is carried out using drugs such as Pancreatin and Creon. It is designed to improve the digestion of carbohydrates and fats. It is important that the preparations do not contain bile acids, but contain enzymes - amylase and lipase.
When, after a month's therapeutic course, the desired effect cannot be achieved, surgery is necessary.
On the subject: The most effective recipes for restoring the pancreas!
Treatment methods
The choice of priority direction of therapy will depend on the obtained diagnostic picture. Conservative treatment is indicated in the following cases :
- the cyst has clear boundaries;
- the neoplasm is single;
- the cavity size is small - fits into a circle with a diameter of up to 20 mm;
- There is no significant pain syndrome and icteric manifestations.
Reference! In all other cases, various types of surgical intervention are used.
Conservative treatment
For the first 7–10 days, the patient will have to remain in bed . You will also need to follow these recommendations:
- fasting diet for 2–3 days;
- restrictions in the diet - refusal of fatty, salty and fried foods, alcohol and cigarettes;
- taking antibiotics - tetracyclines or cephalosporins - to prevent the development of a bacterial infection in the cystic cavity;
- Enzyme therapy will help the body cope with the digestion of fats and carbohydrates. Medicines containing lipase and amylase, but not bile acids, are indicated;
- prescription of proton pump inhibitors (Omeprazole, Rabeprazole), designed to reduce pain and normalize gland secretion.
Treatment is continued for 1 month. If there are no results, the choice is made in favor of surgical intervention.
Surgery
Surgical operations can be performed using various techniques. The optimal choice should take into account the level of invasiveness and the nature of the pathology (reasons for development, size, condition of the tissues and the organ as a whole).
Percutaneous manipulations are considered the most minimally invasive and are highly effective in solving the problem of cysts in the body or head. The essence of the intervention is to insert the instrument through a puncture in the epigastric cavity.
The size of the cyst dictates the following surgical options:
- percutaneous puncture drainage of a pancreatic cyst - first, all fluid is removed from the cavity, then a drainage tube is installed, which is removed when the exudate stops. Manipulation is indicated for small cysts (up to 100 ml volume) that do not block the ducts of the organ;
- percutaneous sclerotherapy - similar to the previous one, however, a special solution is additionally injected into the cavity. As a result, it is cleansed and overgrown with connective tissue.
Attention! Despite the insignificance of the intervention, such operations can have complications such as blood poisoning or the formation of external fistulas.
The next most invasive procedures are laparoscopic operations. Their technique involves inserting endoscopic instruments into the abdominal cavity through two small incisions. These include:
- laparoscopic resection of part of the gland – recommended in the presence of a single space-occupying formation. For example, a vocal cyst measuring 50–70 mm - in this case, the entire affected part of the organ is removed through incisions;
- internal drainage - consists of dissecting and puncturing the cavity, followed by the imposition of an anastomosis (communication) between the cyst cavity and the stomach, small or duodenum. This is a complex, but effective and physiological operation.
If the course of the disease is complicated, the patient’s condition is serious, or it is impossible to perform other types of manipulations, an intervention with dissection of the abdominal cavity is performed. These operations require a long recovery, but make any action related to the removal of a cyst on the pancreas possible. In this group the following types are distinguished:
- excision – the cyst and part of the organ are removed. This is the only solution for malignant neoplasms;
- excision with external drainage (if there are complications) - only for benign pathologies.
Folk remedies
Alternative therapy can complement conservative therapy in the presence of small uncomplicated cysts or a tendency to their occurrence.
It does not replace medications and diet, but is extremely useful for prevention and general strengthening of the body (in the absence of allergic reactions). Therefore, it makes sense to purchase the following herbs:
- St. John's wort, burdock (juice), yarrow, chamomile - will help prevent inflammatory processes;
- elecampane, plantain, aloe (juice) - promote the restoration of organ tissue;
- acacia, mint, valerian - have a calming and antispasmodic effect.
Fees are also effective, for example:
- celandine, yarrow and calendula;
- mint, chamomile, cucumber, plantain, yarrow, St. John's wort;
- mint and dandelion.
The collection allows you to get a comprehensive result, but the risk of developing an allergy to the components increases significantly.
Important! Treatment with folk remedies is unacceptable in the absence of diagnosis of the disease and consultation with a doctor.
Classification
It is customary to distinguish the following types of pancreatic cysts.
True cysts:
- Congenital (single/multiple cysts, localized in the pancreas itself; combined with cysts in the liver/kidneys and other organs; cystic fibrosis of the pancreas).
- Acquired (retention cysts caused by retention of pancreatic secretions; parasitic cysts (for example, hydatid cysts); primary tumor cysts - cystadenomas/cystadenocarcinomas and metastatic ones.
Pseudocysts (extrapancreatic/intrapancreatic):
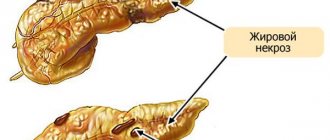
- Being predominantly the outcome of pancreatic necrosis ;
- Post-traumatic cysts (open/closed injuries of the pancreas, operations on the pancreas and adjacent organs).
- Idiopathic.
- Cysts communicating/not communicating with the pancreatic ducts.
According to course/clinical signs
By degree of formation:
- The first stage is acute (the cyst is not formed, the time period is up to 1.5 months from the moment of occurrence).
- The second stage is subacute (a cyst wall has been formed, which consists of loose granulation tissue), over a time period of 2-3 months.
- The third stage - the cyst wall is closely connected with the surrounding tissues.
- The fourth stage - the cyst wall is finally formed and is represented by a dense fibrous capsule, over a period of more than a year.
By location (pancreatic head cyst, pancreatic body cyst, and pancreatic tail cyst).
According to the morphological characteristics of the cysts (intrapancreatic/extrapancreatic; single/multiple; single-chamber/multi-chamber).
According to the severity of the course : simple and complicated (malignancy, suppuration, bleeding, fistula formation, perforation, compression of surrounding organs).
Histological classification (table below).
What symptoms indicate a cyst?
Until a significant increase in diameter, the neoplasm does not reveal itself in any way. The patient may periodically experience discomfort in the left hypochondrium and attribute it to neuralgia or muscle pain. Problems arise when the tumor becomes larger - the growth of cysts triggers the next (or first) exacerbation of pancreatitis.
Pain
The patient experiences sharp pain in the left hypochondrium or in the stomach area, most often after eating. The intensity depends on the size of the tumor. If the solar plexus nerves are pinched, sharp, burning pain occurs immediately under the sternum, shooting into the back. If the cyst puts pressure on the urinary organs, the patient feels nagging pain in the lower back and lower abdomen.
A characteristic feature is that painful attacks are not relieved by analgesics or antispasmodics. Medicines only temporarily relieve discomfort, but do not eliminate them completely. If the cyst does not provoke tissue necrosis, the pain subsides after a few days. Relief can last up to a month, after which the attacks resume.
Dyspepsia
Due to impaired pancreatic drainage, the functioning of the entire digestive tract suffers. The patient is bothered by heaviness in the stomach after eating (even with tiny portions), and nausea occurs. With irreversible damage to the gland, uncontrollable vomiting develops, which does not bring relief (the result of intoxication of the body).
Intestinal function changes. Due to a lack of enzymes, the process of digesting food is disrupted, flatulence occurs, and the patient develops severe diarrhea. The stool contains impurities of undigested food and inclusions of fat (steatorrhea).
Other signs
Against the background of nausea and weakness, the patient loses appetite, and impaired breakdown of food leads to nutritional deficiency and weight loss. Due to inflammation and intoxication, the temperature rises. Indicators rarely exceed subfebrile values, however, with complications, fever and severe hyperthermia are observed.
Large cysts cause compression syndrome of internal organs. Additional symptoms depend on the strength and location of the pressure:
- if the kidneys are compressed, the outflow of urine is disrupted;
- with pressure on the intestines, there may be stool retention and symptoms of obstruction (pain, cramps, abdominal asymmetry);
- the effect on the liver provokes stagnation of bile and the appearance of jaundice.
When palpating the area of projection of the pancreas onto the anterior abdominal wall, tuberosity or protrusion of individual sections of the gland may be detected.
Consequences and complications of cysts on the pancreas
If not detected in a timely manner, a cavity formation of a solid size poses a danger due to complications, which, according to statistics, account for 10-55% of all cases in the form of:
- suppuration,
- perforations,
- bleeding,
- fistulas,
- peritonitis.
If it is not treated in a timely manner, severe consequences may develop:
- the cyst may burst:
- education becomes malignant.
Even if the cyst is removed surgically, there remains a risk of recurrence.