Anatomy
There is a natural anatomical divider between the chest and abdominal cavities - the diaphragm. This is a muscle plate that is attached to the costal surface. It contains a natural opening - the esophagus. The esophagus and large vessels pass through it.
Normally, the stomach, intestines and abdominal esophagus are located below the diaphragm, and the thoracic esophagus is located above. For some reasons, such as increased intra-abdominal pressure, underlying organs protrude through the diaphragmatic opening into the chest cavity.
This is a pathology, since the usual activity and functioning of organs is disrupted, and a hernia of the esophageal diaphragm is formed.
Many people call this phenomenon a hernia between the esophagus and stomach. The mechanism of its formation is the same as the previous pathology.
The displaced wall of the stomach or esophagus acts as a hernial protrusion; it also exits through the diaphragmatic opening. Due to compression of the opening by the gate, a tumor-like hernia is formed between the stomach and esophagus.
Pathology is often found in elderly people over 55 years of age. More often, the disease can be found in women due to the structural features of internal organs and participation in labor.
During childbirth, intra-abdominal pressure increases, which may subsequently affect the development of the disease.
The pathology does not always make itself felt and may occur without clinical signs. Often disguised as other diseases: gastritis, gastric ulcer, pancreatitis, cholecystitis, angina pectoris.
What happens with a diaphragmatic hernia (anatomical information)
The diaphragm is a large parachute-shaped muscle that is located below the lungs and attaches to the costal arches. It has a peripheral muscle and a central tendon part. The vena cava passes through the tendon part to the heart, and in the muscular part there is an opening for the esophagus.
Click on photo to enlarge
The opening for the esophagus is the “weak spot” where diaphragmatic hernias most often form (they are also called hiatal or hiatal hernias). Through it, the esophagus, stomach, and sometimes the intestines exit into the chest cavity.
Normally, in a healthy person, the esophagus is secured by muscular and fibrous ligaments. But if muscle tone decreases, if the left lobe of the liver decreases (atrophies), or a person loses weight so much that the fatty tissue located under the diaphragm disappears, then the esophageal opening “stretches.” Because of this, the ligaments holding the esophagus weaken and the angle at which the esophagus enters the stomach increases (this causes the reflux of gastric contents upward).
The diaphragm is conventionally divided into three parts: lumbar, costal and sternal. In each of them, muscle fibers have their own direction. At the junction of these parts there are triangular sections that are quite pliable. This creates the conditions for the intestines to come out or protrude here. These are already different diaphragmatic hernias.
The structure of the diaphragm and muscles of the posterior abdominal wall. Click on photo to enlarge.
Causes of hiatal hernia
Esophageal diaphragmatic hernia occurs due to a number of factors and causes. This is not only an acquired disease; in children it can be a congenital defect.
It is formed as a result of mutations or breakdowns during the formation and laying of organs and systems. The development of the disease in adults is facilitated by atrophy, weakness and stretching of the diaphragm muscles, stretching of the diaphragmatic ring.
The main reasons for the development of diaphragmatic hernias:
- Embryonic defect in newborns and small children.
In this case, there is a shortening of the size of the esophagus or abnormalities in the development of the stomach. To eliminate the disease, early surgical intervention is required.
- Heredity.
It is observed in individuals whose relatives suffered from similar pathologies.
- With a stable increase in pressure in the abdominal cavity: straining due to constipation, pregnancy, umbilical hernia.
- For edema syndrome of certain pathologies: ascites, heart failure.
- Chronic processes of the gastrointestinal tract: gastritis, peptic ulcer, pancreatitis, cholecystitis, hepatitis and cirrhosis of the liver.
- For oncology in the abdominal cavity.
- Overeating, unhealthy lifestyle.
- Overweight.
- Massive physical activity, heavy lifting.
- Prolonged vomiting due to poisoning or toxic phenomena in the human body.
- Burns of the esophagus with acids and alkalis, and other chemical compounds.
- Abdominal injuries: blows from sharp or blunt objects.
- Cough reflex in chronic lung diseases: tuberculosis, COPD.
- Diseases of connective tissue, including the muscular system: systemic lupus erythematosus, scleroderma.
- Hormonal imbalances and disorders in the body: Cushing's syndrome, Thyrotoxicosis, Hyperthyroidism.
- Surgical interventions in the chest and abdominal cavity.
Etiology
Diaphragmatic hernia can be caused by the following etiological factors:
- dyskinesia of the digestive tract;
- the presence of tumors or scars in the esophagus itself;
- narrowing of the esophagus;
- increased and prolonged flatulence;
- chronic gastroenterological diseases that are accompanied by vomiting;
- benign or malignant tumors in the abdominal cavity;
- accumulation of fluid in the abdominal cavity - ascites;
- frequent, long-term pathological processes of the upper respiratory tract;
- increased intra-abdominal pressure, which is most often caused by coughing.
Predisposing factors for the development of such a pathological process should be identified:
- violations of the structure of the connective tissue of the membrane;
- history of reflux;
- chronic cough;
- hiccups and diseases that have such a symptom in the clinic;
- upward displacement of the esophagus;
- genetic predisposition to this type of disease;
- previous injuries in the abdominal area.
Congenital diaphragmatic hernia of the esophagus currently does not have a clear etiological picture. However, many clinicians note that this type of pathology most often occurs in those children who have a history of:
- Marfan syndrome;
- flat feet.
This disease is quite often a consequence of age-related changes - people who are 50 years or older are at risk.
Diaphragmatic hernia
Degrees of diaphragmatic hernias
Scientists distinguish only three degrees of manifestation of the disease. They all differ in clinical manifestations, symptoms, extent of damage, and dysfunction. In this regard, the doctor prescribes his own treatment tactics for each degree.
1st degree
The level of damage is not significant; it occurs with a sharp increase in abdominal pressure or long-term chronic diseases. The muscles of the diaphragm are atrophied to a lesser extent.
The diaphragm ring is slightly widened. The esophagus and stomach change their localization. Normally, the abdominal part of the esophagus is located in the abdominal cavity.
With a diaphragmatic hernia of 1st degree, the abdominal part rises above the diaphragm and passes into the chest compartment. The stomach is under the diaphragm, but very close to it.
Organ functions are moderately affected. Treatment is conservative with medication, adherence to daily routine and diet.
2nd degree
The esophagus is located entirely in the chest. The upper part of the stomach is displaced to the level of the esophageal opening, the ligamentous apparatus is greatly relaxed.
Symptomatic manifestations occur in the form of pain, belching, heartburn, and heaviness in the epigastrium. The normal functioning of the stomach and esophagus is disrupted. It is treated in combination - surgically and with the help of pharmacological drugs.
3rd degree
The most advanced and severe degree. All structural parts that should be below the diaphragm are moved into the chest. Symptoms are pronounced, the patient’s condition suffers greatly.
High risk of complications in the form of strangulated hernia, bleeding, perforation. It can only be treated surgically.
Forecast
With the right medical approach, the prognosis is favorable . Strangulations of a diaphragmatic hernia with all the ensuing consequences (in particular, necrosis of the strangulated contents) occur much less frequently than strangulations with other types of hernias.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
15, total, today
( 192 votes, average: 4.65 out of 5)
Penile boils: symptoms, causes and treatment methods
Mesadenitis in children and adults: symptoms and treatment
Related Posts
Symptoms and signs of hiatal hernia
Many patients with a hiatal hernia have no symptoms or signs in the early stages. Symptoms develop at grades 2-3.
Sometimes the pathology is confused with other diseases of the digestive system due to the similarity of complaints. There are a number of general changes that are characteristic of the disease.
These include:
- Pain in the area of the xiphoid process or behind the sternum.
Patients say that the pain is somewhere in the middle of the chest or in the projection of the stomach. It is the earliest symptom. Has a burning or aching character.
In case of complications or late stages, the pain is girdling in nature. Based on this symptom, the disease can be confused with acute pancreatitis.
The peculiarity of the pain syndrome is that it intensifies or occurs after consumption or during food intake. Pain can begin after physical activity: bending the body forward, running, lifting heavy loads. The syndrome subsides after changing body position, gag reflex, and drinking cold water.
- Belching is a constant syndrome.
Due to the fact that the position of the esophagus changes, gasroesophageal reflux disease develops. Against this background, the flow of food masses through the esophagus is disrupted.
They are often thrown into the upper sections, and a belch is formed. Unlike other stomach diseases, it is not rotten or putrefactive. There is belching of gases or food eaten, after which the patient feels better.
- Heartburn.
Develops against the background of GERD due to a hernia of the diaphragm. It is permanent and can be triggered by eating any food, especially spicy, sour, fatty, fried.
At stage 3, even drinking plain water causes heartburn and is difficult to eliminate with medication. Because of this, patients are restless, exhausted, and do not sleep at night.
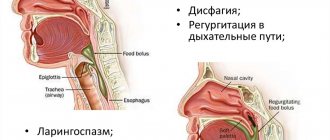
- Dysphagia.
Difficulty in passage of a bolus of food through the digestive tract. Develops due to narrowing or strangulation of the esophagus. At first, solid food is difficult to pass, then liquid food. Patients note swallowing problems and often choke on food.
- Hiccups.
Joins on an empty stomach or vice versa, after overeating. It is not a specific sign, but often accompanies pathology.
- Bitterness in the mouth
- Hoarseness of voice.
- Stool instability.
- Heart rhythm disturbance.
Based on this symptom, the disease is confused with angina pectoris. Characterized by increased heart rate and increased blood pressure.
- Shortness of breath.
Against the background of displacement of internal organs, shortness of breath develops. First it appears after exercise or eating, then at rest.
- Dry non-productive cough.
Doctors make diagnoses based on the pulmonary system, but therapy does not bring results. Then you should suspect a diaphragmatic hernia.
- In case of complications, bleeding appears and the stool turns black. Anemia, pale skin, and tachycardia occur. Blood pressure may drop progressively.
If these signs appear, you should consult a doctor as soon as possible.
Symptoms
Pain syndrome is considered a specific clinical sign of this pathological process. Pain occurs:
- with reflux, which will necessarily accompany a diaphragmatic hernia;
- when part of the stomach penetrates into the chest cavity, as its nerve endings are compressed;
- due to systematically manifested reflux, the walls of the esophagus are stretched, which leads to compression of the nerve endings;
- due to spasms of the esophagus.
The pain syndrome is characterized as follows:
- dull, moderate manifestations - severe pain with this disease is extremely rare;
- localized in the upper part of the retrosternal region;
- spreads along the esophagus, sometimes extending to the area between the shoulder blades.
Manifests:
- after eating;
- with bloating;
- after cough;
- after physical activity.
As a rule, after burping, taking a deep breath, or taking a vertical position, the pain disappears.
The signs of a diaphragmatic hernia are as follows:
- belching after eating;
- diaphragmatic hernia in children under one year of age - regurgitation during feeding;
- pain when swallowing food - the patient needs to drink food often;
- heartburn and belching;
- burning in the tongue area;
- unpleasant pressing sensation in the chest area;
- Solid food passes through the esophagus more easily than liquid or semi-liquid food.
Belching is characterized as follows:
- appears immediately after eating - it doesn’t matter whether the dish was fatty or lean;
- During belching, there is a sour, extremely unpleasant odor in the mouth.
Regurgitation during a hernia is characterized as follows:
- may bother the patient at night - the so-called “wet pillow syndrome”;
- appears after eating if a person immediately assumes a vertical position;
- A small amount of stomach contents is regurgitated, but in particularly severe cases of pathology, vomiting is possible.
It should be noted that in most cases, the symptoms of a diaphragmatic hernia are expressed in a latent form or are completely absent. Even if some of the above symptoms are noted, quite often this is attributed to minor disturbances in the functioning of the gastrointestinal tract, which leads to a delayed diagnosis or no diagnosis at all.
Diagnosis of diaphragmatic hernia
Only a doctor can diagnose and x-ray a hiatal hernia. He will prescribe the necessary measures that will help establish a diagnosis.
First, the doctor talks with the patient and collects all the necessary information about his complaints. Inspection and palpation of the abdomen is mandatory, and the hernia itself can be felt.
To assess inflammatory reactions, the patient undergoes a general blood test; in most cases, it turns out to be normal. There may be leukocytosis or increased erythrocyte sedimentation rate.
To clarify digestive functions, you should submit your stool for a general analysis. Depending on the form and degree of pathology, various changes may be present: excess mucus, undigested fibers, etc.
Your doctor will help you interpret the analysis correctly. The next stage is instrumental research methods.
X-ray
It is an informative and minimally invasive way to determine pathology. An x-ray of the abdominal and thoracic organs with a contrast agent is prescribed, performed on an empty stomach, in the morning.
The contrast is administered intravenously or the patient is asked to drink it, then its settling and patency through the hollow organs is assessed.
X-ray signs of a hernia are:
- Retention of contrast agent in the hernial sac.
- Expansion of the diaphragmatic ring.
- Upward displacement of the esophagus and stomach.
- Changing the position of the diaphragm dome.
- High location of the esophageal sphincter in the image.
If there is insufficient information, they resort to endoscopic methods - fibrogastroduodenoscopy. It allows you to examine the mucous membrane, the displacement of the position of the diaphragm, stomach, esophagus, the presence of ulcerative defects, dilation of the esophageal opening, and detect the hernial protrusion itself.
The sphincter apparatus is assessed by esophageal monometry. It helps to monitor esophageal motility and evaluate conservative therapy.
For a complete examination, they can turn to computer and magnetic resonance imaging methods, which provide an idea and information about the structures in volumetric form. The disadvantage of the method is its high cost.
Causes of hernia
There are several known factors contributing to its formation:
- High pressure in the peritoneum. Provocateurs of this condition are cough, excess weight, prolonged flatulence or constipation. In rare cases, the formation of a hernia is associated with obstructive pulmonary disease, which results in expansion of the lung tissue, i.e. emphysema. All of the above phenomena provoke an increase in abdominal pressure.
- Weak ligamentous apparatus that holds the esophagus in the diaphragmatic opening. A change in the elasticity of the ligaments and the inability to perform their functions of holding the stomach and esophagus in the desired position may be due to pathologies associated with connective tissue deficiency. In some cases, such changes occur with age and the individual exhibits symptoms of a hiatal hernia.
- Impaired gastrointestinal motility, which is mainly caused by the following anomalies: gastritis with high acidity, cholelithiasis, gastric ulcer.
How to treat a diaphragmatic hernia
Complete and correct treatment for a hiatal hernia is prescribed only by a doctor. Therapy is complex and consists of several components:
- Compliance with daily routine and diet.
- Conservative therapy with pharmacological drugs.
- Surgery if necessary.
Treatment without surgery
In the absence of obvious complaints, discomfort, dysfunction and complications, conservative therapy can be prescribed. It comes down to following a diet, losing weight and taking medications regularly.
Doctors advise following simple recommendations that can provide treatment and eliminate symptoms.
Diet for diaphragmatic hernia without surgery:
- Meals should be fractional.
You should eat small portions at regular intervals up to 5 times a day. Be sure to eat breakfast, lunch and dinner. Between them, have an afternoon snack and snacks with fruit or dairy products.
- The last meal should be completed 3 hours before bedtime; it should not be dense.
- Avoid overeating and fasting.
- Avoiding lying down after eating can make reflux worse.
- Avoid overwork and intense physical activity.
- Do not wear tight clothing.
What can be included in the diet
For breakfast, porridge with water, kefir, cottage cheese, and hard-boiled eggs are allowed. For lunch, it is most rational to create a menu of soups for the first course.
The soup should not be greasy, the broth should be clear and not fried. For the second course - boiled vegetables, fresh herb salad, steamed poultry or fish.
The afternoon snack consists of dairy products, cottage cheese, and fruit salad. For dinner you should prepare everything steamed or boiled: potatoes, poultry, rice or buckwheat porridge. Boiled fish is recommended.
Drinks allowed: tea, jelly, compote. Fried, spicy, fatty, smoked, and canned foods are strictly prohibited. Carbonated drinks, alcohol, tobacco, and juices are prohibited.
To treat a hiatal hernia without surgery, medications are prescribed; there are several main groups of them. Each patient must have an individual approach. All medications are prescribed taking into account symptoms and adverse reactions.
- Proton pump inhibitors are included in the standard of treatment, these include Omeprazole. They reduce gastric motility and the secretion of hydrochloric acid. Eliminate inflammation and pain.
- Antacids: Maalox and Almagel. Relieves heartburn, coats the esophagus, and protects the mucous surface from inflammation.
- Prokinetics: metoclopramide. Relieves muscle spasms, relieves nausea and vomiting.
- Antispasmodics: drotaverine, duspatalin. Relieves pain, heartburn, improves intestinal motility.
Causes of a sliding hiatal hernia
The causes of the disease are congenital (natural) and acquired factors. Of the latter, it is worth highlighting:
- increased abdominal pressure;
- age-related changes in the diaphragm;
- cholecystitis, ulcerative lesions and strong contractions of the esophagus;
- relaxation or injury to the nerve tissue of the diaphragm.
Congenital factors include:
- untimely fusion of the diaphragm;
- insufficiently rapid descent of the stomach during the embryonic period;
- underdevelopment of the muscles of the diaphragmatic legs and an enlarged esophageal opening.
In addition, symptoms of a diaphragmatic hernia can be triggered by obesity, pregnancy, and stomach diseases, which increase pressure in the peritoneum.
Surgery
Surgical methods of treatment are used in cases where long-term conservative treatment does not help and complications arise. This is achieved in two ways.
Open - through an incision in the abdominal wall. Laparoscopic - punctures into the abdominal cavity. It is used more actively nowadays.
During the operation, the hernial sac is excised, its contents are examined, and returned to its anatomical location. The diaphragmatic hole is sutured. A retaining mesh is placed on it, which will prevent the hernia from forming again.
Operations are distinguished:
- Crurorrhaphy – suturing of the diaphragm and its ligaments;
- Gastropexy – the stomach and its ligamentous apparatus are fixed in place;
- Fundoplication is surgical intervention on the fundus of the stomach.
Symptoms
Symptoms of a hiatal hernia in many cases are mild or absent altogether. This is explained by the small size of the protrusion. Most often, the manifestation of pathology is observed in patients with large hernias.
Signs of the disease include:
- heartburn (occurs after eating);
- pain in the sternum;
- belching, feeling of fullness in the stomach;
- prolonged hiccups;
- difficulty passing food through the esophagus.
Symptoms of a hiatal hernia such as burning of the tongue (glossalgia), sour taste in the mouth, pain when bending or turning the body are often observed. Many patients complain of a feeling of a lump in the throat, increased salivation, and sudden coughing attacks, especially at night. The appearance of hernias can provoke pain in the heart area. Such signs make it difficult to diagnose the disease, as patients mistake the pathology for cardiac disorders.
Treatment with folk remedies
It is better to carry out herbal medicine in combinations and decoctions. All herbs can be collected independently or purchased at pharmacy chains.
For the first collection, you will need dried herbs: leaves of coltsfoot, peppermint, dandelion, angelica root. An average of 30 grams of each drug.
Mix the ingredients, pour 500 ml of warm water, up to 80 degrees, cover with a lid, leave for 2-3 hours. Drink 150 ml 4 times a day.
Chamomile tea relieves symptoms and relieves inflammation. Dry the chamomile flowers and chop them. Pour boiling water over 1 teaspoon of the mixture, leave for 30 minutes, strain, and drink as tea. Ready-made tea is sold in pharmacies.
Dry collection. You will need: flaxseed, marshmallow root, anise fruit. Dry everything, take equal proportions, grind in a coffee grinder. Use 1 teaspoon of dry mixture 3 times a day.
Signs in adults
In adults, DH is found much more often than in children. The reason for this may be the complex impact of provoking factors on the body throughout life. The most common signs of DH in adults include:
- chest pain resulting from compression of organs;
- the appearance of heartburn, which increases when bending forward and after meals;
Heartburn
- frequent belching containing air;
- bloating;
Bloating
- difficulty breathing.
If left untreated, the disease can become more complicated. In this case, there is a high probability of developing esophagitis or bleeding from the perforation of the hernial sac.
Esophagitis is a disease of the esophagus accompanied by inflammation of its mucous membrane
Signs of acute DH include the following manifestations:
- sharp pain in the stomach;
- nausea and vomiting;
- stool retention;
- deterioration in general health.
Nausea and acute pain in the stomach - symptoms of a hernia
Such symptoms indicate severe damage and require immediate medical intervention. In the absence of medical care, the likelihood of developing peritonitis is high.
Treatment options
Therapy directly depends on the patient's condition. In non-exacerbated cases, treatment is symptomatic. It includes taking medications. Their list is presented in the table.
| Group of drugs | Examples |
| Acetylcholine blockers | "Platifillin", "Atropine", "Hyoscyamine" |
| Antispasmodics | "No-shpa", "Drotaverine" |
| Sedatives | "Validol", "Valocordin" |
| Antiallergic drugs | "Diazolin", "Suprastin" |
| Mineral water | "Esentuki", "Borjomi" |
"Platifillin"
"Drotaverine"
Mineral water
Additionally, diet correction is carried out. Meals should be at least 4 times a day. Reduce portion sizes to reduce stress on the stomach. Foods that can irritate the gastric mucosa and stimulate the release of bile are completely excluded from the diet: fried, fatty, salty, smoked, spicy foods.
Surgical intervention is performed in acute conditions:
- large size of the hernial sac;
- infringement of internal organs;
- lack of response to standard treatment.
Emergency surgical intervention is performed in case of bleeding, perforation of the ulcer, or perforation of the hernial sac. Surgical treatment consists of excision of the sac and elimination of the hernial opening. If there are perforations in the diaphragm itself, it is possible to apply special surgical patches made of artificial material.
Treatment of diaphragmatic hernia
Diaphragmatic hernia, when minimizing the impact of provoking factors, does not pose a threat to the patient’s life. But such patients require regular examinations in order to exclude exacerbations. Read about anti-ulcer therapy on our website.
Diagnostic methods
As mentioned above, DH is most often detected in patients during examination, and they themselves may not even be aware of its presence. There are two main types of diagnostics that can confirm the diagnosis.
X-ray of the stomach
X-ray of the stomach
The principle of operation of this technique is that the contrast agent settles on the walls of the stomach. For this purpose, the patient is given a special barium suspension on an empty stomach. It tastes like chalk. The patient drinks the suspension and in 1-1.5 hours will be ready to perform the study.
X-ray of the stomach with barium
An x-ray shows the shape of the stomach and the presence of hernial sacs. The suspension is naturally washed out of the stomach with further food. It does not have any negative effect on the body and does not cause any inconvenience. Therefore, this method is often used to diagnose DH in children.
Radiography. Diaphragmatic hernia
Fibrogastroduodenoscopy (FGDS)
The most informative diagnostic method. This is an invasive technique during which the doctor can not only check for bags and protrusions, but also assess the condition of the walls. This technique is relevant for checking the presence of ulcerative and erosive lesions.
Fibrogastroduodenoscopy (FGDS)
FGDS is performed on an empty stomach; no preliminary preparation for the analysis is required. A special probe equipped with a camera is inserted into the patient's stomach. With the help of air flow, the walls of the stomach are cleansed from juice and food debris. The use of FGDS, despite its informative nature, is a rather unpleasant procedure, and therefore it is prescribed mainly to adults.
How is FGDS performed?