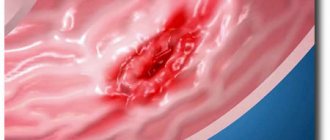
Erosive antral gastritis is a disease in which surface defects form on the mucous tissues in the final part of the stomach. This pathology is often caused by Helicobacter pylori infection. Unlike catarrhal inflammation, with erosive gastritis, in addition to edema and hyperemia of the mucous membrane, the formation of erosions occurs. Erosions can cause ulcers and lead to bleeding.
The course of erosive antral gastritis is often chronic. The acute form of the disease is observed in rare cases. The prevalence of the disease reaches 18% among patients who consulted a gastroenterologist with epigastric pain and who underwent FEGDS. This disease most often affects men, and among children the disease usually occurs in girls. What is erosive antral gastritis, how to diagnose and treat this disease, this is discussed in detail in this article.
Description
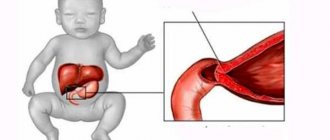
The antrum is the last part of the stomach on the path of food moving into the small intestine. Here the food ball is mechanically ground, mixed and formed. In addition, hydrochloric acid in food is neutralized for the normal functioning of small intestinal enzymes. The acid is deactivated by the protective mucus and bicarbonates secreted by the epithelium.
Erosive antral gastritis is inflammation that develops in the antrum of the stomach and causes pathologies in the mucous tissues of the gastric walls. With timely treatment, the disease will not cause serious complications. If left untreated, peptic ulcers and internal bleeding may develop.
With erosive antral gastritis, swelling of the pylorus (the muscular ring at the junction of the stomach and duodenum) occurs and its walls narrow. This leads to a slowdown in the evacuation of food from the stomach into the small intestine. The food lump stagnates, fermentation begins, and the acidity of gastric juice increases.
Another name for this disease is erosive antrum gastritis. At an early stage, the formation of superficial damage is observed that does not affect the deep layers of mucous tissue. The development of the inflammatory process leads to an increase in the production of hydrochloric acid. Areas of erosion become larger, small vessels of mucous tissues are damaged. The hemorrhagic stage begins: bleeding occurs, the intensity of which depends on the degree of damage and the size of the blood vessel.
Diagnostic measures
The diagnosis can be confirmed using fibrogastroduodenoscopy.
Erosion and papules of the antrum of the stomach can be suspected in the acute period based on the characteristic complaints of the patient. To visually detect ulcers on the gastric mucosa, fibrogastroduodenoscopy, ultrasound diagnostics and radiography with the introduction of a contrast agent are used. It is important to conduct a breath test for Helicobacter pylori contamination. A stool test for occult blood is also indicated. In severe cases, magnetic resonance imaging is performed.
Forms of the disease and types of erosions
According to the clinical course, two forms of this gastropathology are distinguished:
- Acute erosive antral gastritis, resulting from food or toxic intoxication. This form is characterized by rapid development of symptoms. Most often observed in children.
- Chronic erosive antral gastritis, occurring secretly in the early stages. The progression of the pathological process causes complications such as peptic ulcer of the stomach and duodenum or erosive antral gastropathy. This form of the disease usually occurs in adults.
Erosion of the antrum of the stomach is classified into several types:
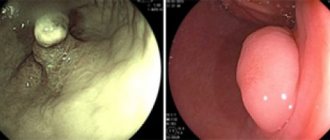
- full. They are cone-shaped outgrowths with a depression in the center. Surrounded by red and swollen mucous tissue. Usually they are numerous and are considered as evidence of chronic inflammation of the stomach;
- superficial. This is a flat overgrown epithelium of various shapes and sizes. A rim of hyperemic tissue forms around the growths;
- hemorrhagic. They are small, needle-prick-like dots on mucous tissues (can be cherry or deep red). The points are surrounded by a swollen rim of hyperemic mucosa, the edges of the erosions bleed.
What is erosion of the antrum of the stomach: causes, symptoms, treatment
This disease occurs against the background of changes in the gastric mucosa, morphologically similar to gastritis. When pathology is detected, there is a need for dynamic monitoring of patients, even in a state of remission.
Erosion in the antrum of the stomach is characteristic of acute and chronic gastritis, gastric and duodenal ulcers, and chronic duodenitis. But they can also have a secondary (symptomatic) nature of formation: occur in liver diseases, heart and pulmonary failure, atherosclerotic lesions of the aorta.
Table of contents
Erosion of the antrum of the stomach: what is it?
Erosion of the antrum of the stomach is a defect in the mucous membrane that does not spread beyond its boundaries (the muscle layer is not involved in the pathological process) and is localized in the lowest part of the stomach, which passes into the duodenum - the antrum.
Erosions, unlike ulcers, heal without a connective tissue scar. Depending on the quantity, multiple (more than 3 damaged areas) and single (from one to three) are distinguished.
Causes of erosions in the antrum of the stomach
Multiple erosions of the antrum of the stomach are found more often than single ones. They are caused by the following reasons:
- damage to the gastric mucosa by the microorganism Helicobacter pylori, which causes gastritis in 20–30% of the adult population and in 95% of cases is the cause of duodenal ulcers;
- prolonged violation of the diet: eating “dry food”, eating excessively hot and rough food, abuse of spices;
- uncontrolled long-term use of medications: non-steroidal anti-inflammatory drugs, sulfonamides, glucocorticoids;
- prolonged emotional stress, neuropsychic processes arising under the influence of chronic stress, difficult life situations;
- alcohol abuse, smoking.
Types of acute and chronic erosions
Acute erosions of the antrum of the stomach occur after a short-term stressful situation. They are defects of regular round or oval shape with a diameter of 0.2–0.4 cm and have smoothed edges. If the defects are covered with hydrochloric acid hematin, an endogenous pigment that colors their bottom black, then they are called “hemorrhagic erosions.”
Chronic erosions of the antrum of the stomach in 52% of cases are multiple and arranged in the form of a chain. They look like polypoid growths up to 5 mm in size with an umbilical retraction in the center.
Table 1. Types of erosion
| Types of erosion | Characteristic |
| Acute | They look like flat, aphthous (superficial) lesions of the gastric mucosa. There are both single and multiple. Epithelializes (heals) in no more than 2–7 days. |
| Chronic | |
There are mature and immature types.
|
Complete erosions of the antrum of the stomach: what is it?
Complete erosion of the antrum of the stomach is localized at the top of the folds of the gastric mucosa and is a “pseudopolyp” with a depression in the center. Such a defect can persist for about 3 years, in contrast to incomplete erosion, which has a flat shape and smooth edges. The cause of formation is chronic inflammation.
Symptoms
Symptoms of erosions include pain, dyspeptic symptoms and nonspecific signs. This pathology is characterized by intense pain, which is localized in the navel area, decreases immediately after eating and resumes after 1.5–2 hours. Night or “hunger” pain often occurs.
Causes
Erosive antral gastritis is provoked by several factors:
- Long-term use of a number of medications.
- Alcohol and drug use.
- Smoking.
- Physical inactivity.
- Mechanical injury and burns.
- Infectious and parasitic pathogens.
- Hormonal imbalance.
- Unhealthy eating, overeating.
- Prolonged stress.
- Kidney and liver pathology.
- Tissue ischemia.
- Radiation exposure.
- Duodeno-gastric reflux.
In most cases, acute erosive gastritis is provoked by toxic substances. For example, the effects of NSAIDs (Movalis, Ketonal, Diclofenac), cocaine, alcohol, diphosphonates and cardiac glycosides. The inflammatory process and damage to mucous tissues can be caused by bacterial and viral pathogens or parasites:
- bacteria Helicobacter pylori;
- cytomegaloviruses;
- streptococci;
- clostridia;
- helminths (for example, anisakiasis).
In some cases, the inflammatory process develops when the functions of the pyloric sphincter are impaired, when the contents of the small intestine, along with bile and pancreatic secretions, are thrown into the stomach and irritate the mucous membrane.
Erosive antral gastritis can be primary or secondary. Secondary is caused by another disease:
- Hyperparathyroidism.
- Crohn's disease.
- Uremia.
- Diabetes mellitus type 1 and 2.
- Stomach cancer.
- Sepsis.
Causes
The causes of erosion of the stomach and duodenum are varied. Typically, several factors act simultaneously:
- with primary erosion - errors in diet, for example, abuse of hot, hot spices, alcohol, coffee; long-term use of non-steroidal anti-inflammatory drugs; severe stress; Helicobacter pylori infection;
- secondary – blood diseases, diabetes mellitus, kidney or liver failure;
- malignant - lymphoma, Crohn's disease, other oncological diseases.
In all forms of the disease, it aggravates the course of erosive gastritis and the healing of existing mucosal defects:
- smoking;
- alcohol consumption;
- excessively cold, hot, spicy or rough food;
- stress;
- duodenogastric reflux;
- taking drugs that cause inflammation and the formation of stomach ulcers, for example, glucocorticosteroid hormones, non-steroidal anti-inflammatory drugs, etc.;
- tendency to starve;
- chronic diseases of the respiratory and cardiovascular systems, which lead to oxygen starvation of tissues.
Symptoms
Chronic erosive gastritis may have nonspecific symptoms. The most commonly observed manifestations are:
- moderate pain in the epigastric region;
- nausea;
- stool disorders;
- heartburn;
- poor appetite;
- bloated stomach;
- general weakness;
- increased sweating;
- vomiting with blood.
In the acute form of erosive antral gastritis, more pronounced symptoms are typical:
- Sharp pain in the abdomen.
- Periodic pain in the lower abdomen (usually after eating).
- Feeling of stomach constriction, burning and heaviness in the abdomen.
- Belching, heartburn.
- Nausea and vomiting.
- Diarrhea followed by prolonged constipation.
If ulcers have formed on the walls of the antrum, the pain syndrome is similar to the pain associated with ulcerative gastrointestinal tract. Pain occurs in the morning on an empty stomach or 1-2 hours after eating. Signs of bleeding with erosive antral gastritis are:
- vomiting blood;
- melena (semi-liquid black stool);
- pale skin;
- cardiopalmus.
When an exacerbation of erosive antral gastritis occurs against the background of reflux, the following symptoms will be observed:
- Belching with a bitter taste.
- Unpleasant taste in the mouth.
- White coating on the tongue.
Over time, the inflammatory erosive process causes atrophy of the glands. In this case, pain may not be felt. Appetite decreases, a feeling of fullness in the stomach is felt, the person quickly becomes full and loses a little weight.
Types of erosive damage
The antrum makes up about a third of the entire stomach and is located in its lower part, separated from the duodenum by just a pyloric ring.
Erosion of this part of the organ is a violation of the surface of the integumentary tissues of the stomach, affecting mainly its upper layers without affecting the muscular layer, which is able to heal without the formation of a connective tissue scar.
Externally, erosion looks like one or several ulcers of a round or irregular shape with a diameter of 0.03 to 1.5 cm, located on the bottom or walls of the stomach. Some experts are inclined to attribute such damage to the mucous membrane to a pre-ulcer disease, while others consider it an independent nosological form.
Erosion of the antrum of the stomach can exist in such forms as:
- Acute erosion, characterized by the absence of an epithelial layer, weak infiltration by lymphocytes and the presence of small fibrin deposits at the bottom. With proper treatment, ulcers heal without scarring within a couple of weeks.
- Chronic erosion, accompanied by dystrophy of the gastric glands and consisting of granulation tissue with the presence of dilated capillaries at the bottom, which resembles the suckers of an octopus, and layering of hyperplastic epithelium along the edges. It has the shape of round defects up to 10 mm in size. Treatment may take several years.
Based on pathomorphological characteristics, it is customary to distinguish the following types of erosions:
- hemorrhagic, which can be both superficial and deep, with a pale edematous membrane and blood on top;
- flat (superficial), with low edges, a clean or white-lined bottom and hyperemic mucosa around the defect in the form of an edematous rim;
- complete, or hyperplastic inflammatory, with moderate swelling, externally similar to polyps and localized at the top of the folds of the stomach.
Depending on the number, erosive damage to the walls of the stomach can be not only single (from 1 to 3), but also multiple (more than 3).
Complications
The development of acute and chronic erosive antral gastritis often leads to bleeding resulting from the destruction of the walls of blood vessels in areas with erosion. In this condition, the following symptoms appear:
- dizziness;
- weakness;
- a sharp decrease in blood pressure;
- cardiopalmus;
- liquid black feces with clotted blood;
- vomit;
- confusion;
- increased sweating.
The more intense the bleeding, the more severe the patient’s condition becomes. In the absence of timely treatment, ulcers form and gastric bleeding develops. This is a serious condition that is difficult to treat and increases the risk of developing malignant tumors. In addition, erosive antral gastritis can cause the development of stenosis and deformation of the pylorus. If you do not pay attention to the symptoms of massive blood loss, anemia and shock may develop.
Classification
All erosions can be single or multiple:
- Single ones are located in different parts of the stomach, and their number does not exceed 3 pieces.
- Multiple are 3 or more located within the same department.
Erosion of the stomach or duodenum is classified according to the causes of occurrence, the nature of the course and the predominance of certain symptoms of the disease.
Types of gastric erosion
The following types of erosion exist:
- Primary – occurs with erosive gastritis in the form of single or multiple defects of the mucous membrane.
- Secondary - develops as a result of existing diseases of other organs and systems of the body, leading to a deterioration in the blood supply to the gastric mucosa and disruption of the renewal processes of epithelial cells.
- Malignant - observed in the case of various oncological diseases, Crohn's disease.
Forms of the disease
Depending on the healing time, acute and chronic forms of gastric erosion are distinguished:
- Healing of acute erosion occurs within 1.5-2 weeks (sometimes 2 months). It is located mainly in the upper parts of the stomach. The acute form is characterized by a complete absence of epithelium in the area of the defect, its bottom is slightly covered with fibrin. Microscopic examination reveals weak infiltration of lymphocytes.
- In chronic cases, the healing process can take up to 5 years or more. Its favorite place of localization is the final section of the stomach, which borders the duodenum - the antrum. The chronic form of the disease is erosion from granulation tissue, at its bottom there is dilation of the capillaries, degeneration of the gastric glands, and along the edges there are characteristic “ridges”, which are a layering of hyperplastic epithelium.
Types
Experts distinguish 2 common types of clinical picture of erosions:
- Ulcer-like.
- Hemorrhagic.
The ulcer-like clinical picture with its symptoms resembles a peptic ulcer, characterized by the following “set” of symptoms:
- heartburn;
- nausea;
- belching;
- pain that occurs after eating or on an empty stomach;
- vomiting, which may bring relief.
Hemorrhagic erosion is characterized by:
- anemia;
- positive stool occult blood test;
- periodically black feces;
- may not be accompanied by painful sensations.
The mixed type occurs with erosive-hemorrhagic gastritis. Compared to the ulcerative and hemorrhagic types, it has a more severe course.
According to pathomorphological characteristics
Hemorrhagic erosions . They are called so because the top is covered with a bloody coating against the background of a pale and swollen membrane. They can be superficial and deep.
Surface (flat) . Such erosions have a clean bottom, which can be lined with a white coating. They have low edges, outlined by a hyperemic, edematous rim.
Full (hyperplastic) . They look like edematous polyps that are located at the top of the gastric folds.
Diagnostics
To diagnose erosive antral gastritis, you need to conduct a comprehensive examination:
- External examination with palpation and identification of painful areas.
- Collecting a detailed medical history (data on lifestyle, nutrition, bad habits, concomitant diseases, medication use).
- Blood tests (general, biochemical and for Helicobacter pylori infection).
- Enzyme immunoassay test.
- FEGDS.
- Polymerase chain reaction.
- Analysis of stool for blood.
- Breath test.
- Ultrasound.
- Biopsy with histology.
- X-ray (simple and contrast).
- pH-metry.
Carrying out a set of studies is necessary for differential diagnosis with diseases such as peptic ulcer, cholecystitis, cancer, pancreatitis and functional disorders.
Erosion of the stomach
On the mucous membranes, due to a number of reasons, lesions of the upper integumentary layer may be detected that do not penetrate into the depths of the muscle wall.
Outwardly, they look like round or oval areas with a complete absence of integumentary epithelium; sometimes their surface can bleed, but in this case, erosion is understood as a clean defect, not covered by a clot. The term “aphthous” (forming a discolored spot with a yellowish rim) is often used to describe the lesion.
Ulcers have a diameter of 0.5 to 15 mm and can be found in any part of the stomach. Attitudes towards erosion vary - some experts consider it an independent disease, others - a condition preceding an ulcer. In practice, specialists often encounter the manifestation of both erosion and ulcerative lesions in the same areas of the gastric and duodenal mucosa.
The condition is detected in every sixth patient with complaints of indigestion and stomach pain, more often in people over 30 years old, and the older the patient, the more often the disease is detected.
What is gastric erosion and why does it occur? The mechanism of development of the pathology is not fully understood. Most experts believe that, for certain reasons, some of the cells in the gastric mucosa experience oxygen starvation. Under the influence of this factor, the reproduction of mucosal cells is disrupted, the integumentary layer becomes completely thinner, gradually forming areas lacking protection.
Bare areas are exposed to gastric juice and die, forming areas of necrosis. After 10-15 days they heal without forming scars.
Erosion can be:
- primary, which are formed in young people without serious illnesses under the influence of external stimuli;
- secondary, and are determined in elderly people against the background of underlying pathologies.
The chronic course of the process is influenced by a hereditary predisposition to dysfunction of the mucous membrane. Clinical experience shows that most gastric erosions remain unrecognized during life (in approximately 15% of people).
Treatment
Therapy for erosive antral gastritis consists of the following therapeutic measures:
- elimination of pathogens;
- eliminating the inflammatory process;
- pain relief;
- stopping bleeding;
- reducing acidity levels and restoring the composition of enzymes.
The most effective two-stage therapy is aimed at eliminating pathogens and restoring tissue damage:
- The first stage is aimed at therapy using potent drugs.
- The second stage is aimed at restoring mucosal tissues that are affected by erosion.
When treating antral gastritis, drug therapy is prescribed, including drugs such as:
| Group of drugs | Name |
| Antibiotics (eliminate pathogenic microflora) |
|
| Bismuth salts |
|
| Antacids (reduce stomach acidity, neutralize acid by reacting with or absorbing excess) |
|
| Proton pump inhibitors (antisecretory, block acid production) |
|
| Gastroprotectors (envelop and protect the mucous membrane) |
|
| Antispasmodics (eliminate painful contractions of the stomach muscles) |
|
| Analgesics (pain relief) |
|
| Enzyme preparations (improve digestion) |
|
It is not enough to treat erosive antral gastritis with medication alone. A radical restructuring of diet and food preferences is needed.
Diet
For erosive antral gastritis, it is necessary to follow the basic principles of a therapeutic diet:
- prepare dishes from foods that are easy to digest and do not irritate the mucous membrane of the gastric walls;
- eat food warm. Food that is too hot or cold should be avoided, as it has a negative effect on damaged stomach tissue;
- You should eat at least five times a day. It is necessary to rationally create a menu consisting of complete and healthy dishes, and also avoid snacking;
- eat without haste and chew food thoroughly;
- a single amount of food should be 250-300 g;
- in the chronic form of the disease, it is allowed to eat some fruits and berries;
- During treatment, any sweets are excluded from the diet. Honey and dried fruits are allowed in small quantities.
Foods that are useful to eat for erosive antral gastritis, and which should be excluded from the diet:
| Allowed | Excluded |
| Viscous porridge with water, you can add a little milk and honey | Fried and fatty foods |
| Vegetables are eaten only when thermally processed: stewed or boiled. | Alcoholic and carbonated drinks, coffee |
| Fresh fruits in small quantities: persimmons, watermelon, bananas. Other fruits cannot be eaten fresh. | Very hot or cold food. For example, ice cream |
| Dairy products: kefir, fermented baked milk, yogurt, cottage cheese, milk | Sweets, chocolate, baked goods |
| Lean meat and fish, boiled or stewed | Fresh bread. Exception: wheat germ bread |
| Quail egg omelettes and casseroles | Fresh vegetables and fruits |
Folk remedies
Complex therapy of erosive antral gastritis is well complemented by proven traditional medicine recipes that have an anti-inflammatory, enveloping and healing effect:
- Fresh potato juice. Drink 3 times during the day, gradually increasing the dose (from 25 ml to 100 ml.). Duration of treatment – 2 weeks.
- Infusion of sea buckthorn berries. Pour boiling water (1:5) over sea buckthorn and leave for 2 hours. Add a little honey. Drink up to 1 liter during the day.
- Sea buckthorn oil. Take 1 tbsp. spoon 3 times a day.
- Cabbage juice. Drink 1/2 cup of freshly squeezed juice throughout the month.
- Honey. Can be used as a stand-alone remedy, or added in small quantities to any recipe.
Treatment options
Therapy for erosions in the antrum should be comprehensive, because this will help introduce the disease into a long period of remission. Therefore, it is recommended to use medications that are aimed at eliminating the main symptoms and possible irritants to the mucous membrane. Diet and proper nutrition with the absence of bad habits are important. If it is impossible to eliminate or reduce the manifestations of the disease, surgical removal of the stomach is performed to prevent the development of complications, leaving the organ stump. Sometimes folk remedies are used.
Treatment with medications
Traditional methods of therapeutic intervention consist of eliminating the symptoms of pathology. When Helicobacter pylori is detected, it must be eliminated, which is done with the help of antibacterial drugs. It is recommended to take antacids, proton pump inhibitors and H2-histamine receptor blockers, which reduce the secretion of hydrochloric acid, irritating erosions and papules in the stomach. In case of severe nausea, antiemetic drugs are used that act on the vomiting center of the medulla oblongata, eliminating this impulse. If the evacuation of gastric contents is impaired, take Immodium or Motorix.
Folk remedies
Sea buckthorn oil will help heal wounds on the organ mucosa.
Treatment of erosion is possible using non-traditional methods. To do this, use a calamus decoction of 50 ml before each meal. Chamomile decoction is also a good remedy, which has an enveloping and wound-healing effect. You can use immortelle tincture, which is taken before meals. It helps restore mucous membranes and increases appetite. Sea buckthorn oil will be useful. Treatment with folk remedies is effective and widely available, so it is used very often.
Therapeutic diet
Its use is recommended for severe symptoms and during remission. Proper nutrition will help avoid injury to the gastric mucosa and will promote the healing of erosions and prevent the formation of new wounds. It is important to avoid eating fatty, fried and spicy foods, and avoid alcoholic beverages and coffee. Preference should be given to boiled food, especially liquid food. Healthy dishes include soups, grated porridges, and boiled vegetables. You need to eat regularly and in small portions, without overeating.
To treat erosion, you must follow a diet.
Prevention
To prevent the development of erosive antral gastritis, a number of preventive measures must be observed:
- timely treatment of gastrointestinal diseases and infectious diseases;
- maintaining sanitation and hygiene;
- avoiding unhealthy diets;
- adherence to a therapeutic diet and a regular diet (at least five times a day with an interval of 3 hours);
- giving up bad habits (smoking, alcohol and drug abuse);
- maintaining an active lifestyle;
- exclusion of stressful situations and strong radiation.
The condition of the mucous tissues of the stomach walls and their protective properties largely depend on a person’s lifestyle and his immune system. To prevent complications of gastritis, when the first manifestations of the disease are detected, you should urgently seek medical help.
List of references: https://sakhalinmedia.ru/news/23.11.2015/erozivniy-gastrit—kachestvennaya-diagnostika-i-effektivnoe-lechenie-za-rubezhom.html msdmanuals.com/ru/professional/diseases-gastrointestinal- tract/gastritis-and-peptic-ulcer/erosive-gastritis https://www.obozrevatel.com/health/bolezni/antralnyij-gastrit.htm https://kiozk.ru/article/cto-takoe-erozivnyj-gastrit- simptomy-i-lecenie-bolezni https://www.passion.ru/health/zhkt/antralnyy-gastrit-simptomy-i-lechenie-85966.htm https://www.promedicina.clinic/adult/gastrit-erozivnyj/ med.vesti.ru/articles/zabolevaniya/erozivnyj-gastrit-zheludka-simptomy-lechenie-dieta/ https://www.wmj.ru/stil-zhizni/zdorove/erozivnyy-gastrit-simptomy-lechenie-pravilnoe-pitanie. htm https://atvmedia.ru/materials/gastrit-antralnogo-otdela-zheludka Notes from the author of the article, based on personal experience. This material is purely subjective and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/16/2020
Features of treatment
Treatment of gastric erosion is complex and necessarily includes diet therapy, cessation of smoking and alcohol, and the fight against stress factors. If necessary, pharmacological drugs, physiotherapeutic procedures are prescribed, and in case of severe disease, endoscopic coagulation of bleeding vessels and even removal of part of the stomach in the classical way.
Complex treatment of gastric erosion necessarily includes:
- lifestyle correction;
- special strict diet;
- taking medications.
Drug treatment
For gastric erosion, taking into account the nature of the disease, medications are prescribed:
- reducing the acidity of gastric juice and the production of hydrochloric acid - antacids (Rennie, Almagel), proton pump inhibitors (Omeprazole), H2-blockers of histamine receptors (Kvamatel);
- agents that have a healing and restorative effect (bismuth preparations - De-Nol, Vikalin, synthetic prostaglandins - Misoprostol, if there is no pregnancy);
- antispasmodics (No-shpa);
- if Helicobacter pylori is present, antibiotics (watch the video);
- in case of bleeding - hemostatic drugs, hemostatics.
Etiology and pathogenesis
The occurrence of erosions in the antrum of the stomach is associated with significant thinning of the membranes and walls, while the muscle layer remains completely intact. Healing of the wound surface leads to the formation of scars on the wall and disruption of normal digestive function in this area. Scars are formed as a result of long-term damaging effects on the mucous membrane of various factors.
The most common causes of erosion in the antrum of the stomach include the following:
- diseases of the heart and blood vessels;
- hormonal imbalance;
- taking aggressive medications;
- terminal stages of cirrhosis or nephritis;
- smoking;
- drinking alcohol in large quantities;
- poisoning with chemical compounds or heavy metals;
- stress;
- excessive activity of the vagus nerve and the release of excess hydrochloric acid;
- errors in diet;
- Helicobacter pylori infection;
- consumption of excessively hot or cold food;
- binge eating;
- eating fast food.
The development of gastric erosions is a hereditary pathology.
As a result of the irritating effects of various factors, single hyperplastic aphthous papules are formed on the surface of the membrane, from which multiple superficial ulcers are formed over time. The acute process causes significant inflammatory symptoms, and when it subsides, chronic mucosal erosion occurs. It consists of areas containing flat and dense scars in which epithelization has occurred. They alternate with foci containing an ulcer. Acute gastric erosions are characterized by areas with absent epithelium, and the gastric mucosa looks like a gaping wound.
Nutrition and diet for gastric erosion
A properly organized menu helps to get rid of this pathology even without drug treatment. Eating for gastric erosion should be frequent and regular. Meals should be taken approximately 3.5 to 4 hours apart. The serving should be between 250 and 300 ml. Larger amounts of food can aggravate the disease.
A special diet for gastric erosion provides for a large amount of protein, which is necessary for tissue regeneration. What can you eat if you have stomach erosion - list of foods and dishes:
- slimy porridges (rice, semolina, oatmeal, wheat);
- jelly, compotes, herbal teas;
- vegetables and fruits with the exception of cabbage, radish;
- boiled chicken and lean beef (pork is excluded);
- boiled, steamed fish;
- butter, olive oil;
- only freshly squeezed juices with the exception of orange;
- fermented milk products, cottage cheese, kefir, whey, sour cream, low-fat yogurt;
- no more than 1 egg per day, boiled or as part of an omelet;
- puddings, soufflés, steamed cutlets, slimy and pureed soups, mashed potatoes.
Depending on what patients eat during gastric erosion, the process of restoration of the mucous membrane may be slower or faster. Completely exclude coffee, alcohol, cabbage, chocolate, and foods containing artificial colors and preservatives from your diet. You should avoid smoked meats, pickles and jams. Use honey and other bee products with caution. Although propolis has excellent restorative properties. Sometimes it is recommended by gastroenterologists for the treatment and prevention of peptic ulcers.
Treatment of erosions
Treatment of the pathology depends on the symptoms detected and the presence of concomitant diseases, and is similar to the treatment of gastritis and peptic ulcers. The goal of treatment is to relieve painful symptoms and bleeding by restoring the integrity of the gastric mucosa. The complexity of the disease requires systemic multicomponent treatment:
- conservative, which includes medication and physiotherapeutic treatment, diet;
- surgical, which is prescribed for massive bleeding in which it is impossible to determine the cause of the condition.
In many cases, treatment requires changes in lifestyle - giving up alcohol and smoking, changing work to reduce the level of nervous tension.
Drug treatment is aimed at:
- elimination of Helicobacter Pylori using complex treatment with De-Nol, Clarithromycin and Amoxicillin, Metronidazole, Omez;
- protection of the stomach walls from the aggression of hydrochloric acid Famotidine, Ranitidine, Omeprazole;
- regulation (reduction) of the level of gastric juice production Pantoprazole, Rabeprazole;
- lowering the level of acidity in the stomach (antacids) - Gastal, Reni, Almagel, Maalox;
- coating agents to protect the walls of the stomach (gastroprotectors) Gelusil, Cytotec;
- stimulating organ motility with constant nausea - Motilium;
- calming – motherwort, valerian;
- general strengthening agents - complex vitamin preparations with the inclusion of microelements (Duovit), vitamin complexes B1-B12, PP.
A necessary component of treatment is the establishment of a diet. Table No. 1 is usually used; in case of concomitant diseases, correction is carried out.
Surgical treatment is used in case of severe bleeding. The patient must be hospitalized in a hospital; to stop bleeding, the stomach is washed with ice water.
To relieve the consequences of blood loss, plasma is prescribed; bleeding is stopped using hemostatic agents - Vikasol, Amincaproic acid. To regulate the process of gastric juice production, Pepsidin and Kvamatel are prescribed.
To stop bleeding in hemorrhagic erosions, cauterization with a laser or radio wave treatment is used. As a radical measure, abdominal surgery (removal of part of the stomach) is performed.
Physiotherapeutic treatment is carried out if bleeding is not observed. Depending on the condition, the following is prescribed:
- modulated currents;
- electrophoresis;
- oxygenation;
- thermal procedures;
- various baths (radon, pine, mineral);
- acupuncture.
Control examinations are carried out monthly, hardware diagnostics - once every 2 months. Signs of cure are:
- improvement of well-being;
- no pain;
- reduction of swelling and redness in the lining of the stomach;
- restoration of mucous membranes.
After restoring the functions of the mucous membranes and relieving the symptoms of erosion, the patient must adhere to a certain lifestyle that will prevent exacerbations of the condition.