Feces are the final product of the processing of products entering the body. A healthy person who does not suffer from digestive problems has formed stools that do not contain neutral fat. The result of digestion of food and absorption of residual products in the intestine should be covered with a small amount of mucus and columnar epithelial cells. If neutral fat is present in the stool, the condition is called steatorrhea. It is considered pathological and may indicate diseases of the pancreas, bile ducts or liver.
What are fats?
Neutral fats are called esters of fatty acids and glycerol. Depending on how many hydroxyl groups of glycerol are esterified with fatty acids, the following types of lipids of this group are distinguished:
- triglycerides - three groups;
- diglycerides - two groups;
- monoglycerides are one group.
Neutral fat is found in the human body in the form of reserve material or becomes protoplasmic fat, which is part of the cells. The role of these forms is different. Protoplasmic lipids have a constant composition and exist in cells in a certain amount, which does not change with the development of obesity or in the case of a person losing weight. The amount of reserve fat tends to fluctuate.
Triglycerides
This group is the most numerous among all representatives of neutral lipids. Fatty acids included in the composition can be unsaturated and saturated. The most common are oleic, stearic and palmitic acids. If the radicals that make up a triglyceride belong to one acid, then it is called simple; if they belong to different acids, it is called mixed.
The physicochemical properties of neutral fats depend on what acids are included in the composition. Features are as follows:
- the greater the number and length of saturated fatty acid residues, the higher the melting temperature of lipids;
- the greater the amount of unsaturated fatty acids and the shorter their chain, the lower the melting point;
- triglycerides can participate in the saponification reaction, resulting in breakdown into fatty acids and glycerol;
- The saponification process is characteristic of enzymatic hydrolysis, the action of alkalis and acids.
Properties of lipids
Neutral fat is a substance that melts easily; it is lighter than water, but insoluble in it. At room temperature, lipids are solid, paste or liquid and can melt over a wide temperature range.
The substances are practically insoluble in water, but adding soap or some kind of emulsifier to them leads to the formation of persistent aqueous emulsions. Neutral fat dissolves well in alcohol and various solvents (ether, gasoline, benzene, chloroform).
Phospholipids are colorless but quickly darken when exposed to air. This occurs as a result of the oxidation of unsaturated fatty acids included in the composition. The properties of neutral fats found in the human body are as follows:
- layered structures that form upon contact with solutions make it possible for lipids to participate in the construction of cell membranes;
- entering into a close relationship with proteins located on the surface of cell membranes, they regulate the processes of entry into the cell of organic substances that participate in metabolic processes;
- are antioxidants of natural origin.
The dependence of the physicochemical properties of neutral fats on their structure explains the possibility of their participation in vital processes occurring in the human body. Especially a lot of phospholipids are found in nervous tissue, liver, and heart.
What does neutral fat mean in coprogram? Diagnostics
Feces are the final product of the processing of products entering the body. A healthy person who does not suffer from digestive problems has formed stools that do not contain neutral fat.
The result of digestion of food and absorption of residual products in the intestine should be covered with a small amount of mucus and columnar epithelial cells. If neutral fat is present in the stool, the condition is called steatorrhea.
It is considered pathological and may indicate diseases of the pancreas, bile ducts or liver.
What are fats?
Neutral fats are called esters of fatty acids and glycerol. Depending on how many hydroxyl groups of glycerol are esterified with fatty acids, the following types of lipids of this group are distinguished:
- triglycerides – three groups;
- diglycerides – two groups;
- monoglycerides are one group.
Neutral fat is found in the human body in the form of reserve material or becomes protoplasmic fat, which is part of the cells. The role of these forms is different. Protoplasmic lipids have a constant composition and exist in cells in a certain amount, which does not change with the development of obesity or in the case of a person losing weight. The amount of reserve fat tends to fluctuate.
This group is the most numerous among all representatives of neutral lipids. Fatty acids included in the composition can be unsaturated and saturated. The most common are oleic, stearic and palmitic acids. If the radicals that make up a triglyceride belong to one acid, then it is called simple; if they belong to different acids, it is called mixed.
The physicochemical properties of neutral fats depend on what acids are included in the composition. Features are as follows:
- the greater the number and length of saturated fatty acid residues, the higher the melting temperature of lipids;
- the greater the amount of unsaturated fatty acids and the shorter their chain, the lower the melting point;
- triglycerides can participate in the saponification reaction, resulting in breakdown into fatty acids and glycerol;
- The saponification process is characteristic of enzymatic hydrolysis, the action of alkalis and acids.
Properties of lipids
Neutral fat is a substance that melts easily, it is lighter than water, but insoluble in it. At room temperature, lipids are solid, paste or liquid and can melt over a wide temperature range.
The substances are practically insoluble in water, but adding soap or some kind of emulsifier to them leads to the formation of persistent aqueous emulsions. Neutral fat dissolves well in alcohol and various solvents (ether, gasoline, benzene, chloroform).
Phospholipids are colorless but quickly darken when exposed to air. This occurs as a result of the oxidation of unsaturated fatty acids included in the composition. The properties of neutral fats found in the human body are as follows:
- layered structures that form upon contact with solutions make it possible for lipids to participate in the construction of cell membranes;
- entering into a close relationship with proteins located on the surface of cell membranes, they regulate the processes of entry into the cell of organic substances that participate in metabolic processes;
- are antioxidants of natural origin.
The dependence of the physicochemical properties of neutral fats on their structure explains the possibility of their participation in vital processes occurring in the human body. Especially a lot of phospholipids are found in nervous tissue, liver, and heart.
Steatorrhea and its types
Neutral fat in feces is a pathological condition. Depending on the etiology, the following types of steatorrhea are distinguished:
- Intestinal type. Due to certain reasons, lipids are not absorbed in the intestinal tract, but are released with feces.
- Alimentary type. The basis of this pathology is poor nutrition. With food, the human body enters a huge amount of phospholipids, which are not able to be absorbed in full.
- Pancreatic type. Occurs as a result of disturbances in the functioning of the pancreas. There is a decrease in the synthesis of lipase, the enzyme responsible for the normal breakdown of lipids.
Steatorrhea also differs in the variety of components. Stool may contain significant amounts of neutral fats (triglycerides), soap and fatty acids, or all three.
Causes of pancreatic steatorrhea
Neutral fat in the feces of a child or adult can appear against the background of a number of abnormal conditions.
1. Diseases of the pancreas:
- acute pancreatitis during the first six months;
- inflammation of the pancreas lasting more than six months (chronic process);
- narrowing of the Wirsung duct (through which pancreatic juice enters the duodenum);
- Solinger-Ellison syndrome is a tumor process that results in ulcerations of the stomach and intestinal tract.
2. Liver pathologies:
- hepatitis of acute and chronic nature;
- hepatitis resulting from alcohol abuse;
- cirrhosis of the liver;
- cholangitis of the sclerosing type - an inflammatory disease of the intrahepatic bile ducts, which is accompanied by the formation of scars;
- hemochromatosis is a disorder of metabolic processes associated with iron, which is accompanied by its pathological accumulation in the body;
- liver amyloidosis;
- tumors and cysts.
3. Pathology of the gallbladder and ducts:
- cholelithiasis;
- inflammation of the gallbladder, acute and chronic;
- cholangitis – inflammation of the bile ducts;
- infection of the biliary tract with Giardia.
Causes of intestinal steatorrhea
Neutral fat in the coprogram with intestinal type pathology can occur as a result of the following conditions:
- with Crohn's disease - chronic inflammation of the intestinal tract, in which narrowing and ulceration develop;
- with Whipple's disease - a disease of the intestines and regional lymphatics of an infectious nature;
- with intestinal lymphoma - a tumor that consists of lymphocytes;
- in post-resection condition;
- with enteritis, enterocolitis;
- with amyloidosis;
- with diverticulosis - a pathological process accompanied by the formation of diverticula (protrusions) in the intestinal wall.
Other etiological factors
The causes of the appearance of phospholipids in feces may be diseases of the endocrine glands. The most common provoking factors are hypothyroidism and Addison's disease (adrenal insufficiency).
Abetalipoproteinemia (impaired absorption and transport of lipids), cystic fibrosis (the secretions of all glands are highly viscous and thick) and cealkia (a disease in which gluten is not completely broken down) are congenital conditions that lead to the appearance of neutral fat in the feces of infants.
The appearance of phospholipids in feces can accompany psoriasis and eczema, as well as long-term use of laxatives and drugs used for weight loss.
The first manifestation of the pathology is a frequent urge to defecate. Feces are oily and difficult to wash off the surface of the toilet. Feces leave a greasy residue. The color of stool may remain normal, or it may change towards a light or gray shade.
In addition, neutral fats, which contain fatty acids and glycerol, appearing in the feces can also be reflected in the following symptoms:
- dry cough;
- dizziness;
- joint and back pain;
- bloating;
- low level of performance;
- weakness;
- dry mucous membranes;
- exhaustion;
- bleeding gums.
The appearance of oily stools and at least one of the accompanying symptoms is a reason to seek qualified help.
Diagnostic measures
The collection of complaints and anamnesis is accompanied by clarification of when the symptoms appeared, what the patient associates with their occurrence, when the stool acquired an oily character.
The specialist clarifies the presence of congenital diseases or inherited pathologies among the patient’s relatives. Next, the doctor examines the patient.
The presence of exhaustion, the condition of the skin and mucous membranes are determined, and palpation and percussion of the abdominal organs is performed.
Coprology (laboratory examination of stool) consists of assessing the following indicators:
- Macroscopy - steatorrhea manifests itself in the form of lighter-colored stools with the sheen of frozen fat.
- Microscopy determines the presence of lipids, fatty acids, and soap. Normally, no more than 5 g of neutral fat should be excreted in stool within 24 hours. The results above are pathological.
If necessary, a radioisotope study, ultrasound examination of the abdominal organs, colonoscopy, assessment of the hormonal balance of the body, consultation with an endocrinologist and therapist are used.
Elimination of steatorrhea
First of all, treatment is aimed at the disease that caused the appearance of neutral fat in the stool. Individual selection of diet is also carried out based on the underlying pathology. It is mandatory to exclude fried, pickled and smoked foods.
The patient must stop drinking alcoholic beverages and get rid of bad habits. It is recommended to add to the diet those foods that contain significant amounts of retinol, tocopherol, calciferol and vitamin K. These same fat-soluble vitamins are prescribed in the form of medications.
Complications and consequences
Complications develop only if treatment is not started in a timely manner. There is a disruption in the absorption of nutrients in the intestinal tract. Against this background, hypo- and avitaminosis, protein deficiency and exhaustion of the body develop. Pathology of water and electrolyte balance is manifested by a constant feeling of thirst, edema, dehydration, and convulsive attacks.
The specialist diagnoses the appearance of oxaluria (excessive pathological excretion of oxalic acid salts from the body along with urine) and the formation of urinary stones of oxalate origin.
This pathological condition occurs because, under normal conditions, oxalates do not enter the blood from the intestinal tract, since their combination with calcium makes them insoluble.
With the development of steatorrhea, calcium is excreted in large quantities from the body along with feces. This leads to a significant release of oxalates from the intestines into the blood.
The patient loses body weight quite sharply. The normal functioning of all internal organs and systems is disrupted. Such manifestations lead to psychological problems (insomnia, changes in communication, decreased performance).
Preventive measures
Preventive measures can be divided into primary and secondary. Primary prevention is carried out to prevent the disease from appearing. It is based on preventing the development of pathologies in which steatorrhea becomes one of the symptoms. The important points are:
- cessation of smoking and excessive consumption of alcoholic beverages;
- correction of diet;
- increasing the amount of plant food consumed;
- fractional meals in small portions;
- use of multivitamin complexes;
- strengthening the body's defenses.
Secondary prevention (after the onset of the disease) is based on timely, rational treatment of the pathological condition.
Conclusion
Early diagnosis and correct diagnosis will allow the specialist to select an individual treatment regimen and avoid the development of complications of the disease.
Self-medication is not recommended, since only a highly qualified doctor can determine the true cause of the appearance of neutral fats in the stool and eliminate it.
The prognosis is favorable for those patients who follow the advice and recommendations of the treating specialist, and also engage in secondary prevention of pathology.
Source: https://FB.ru/article/276016/chto-znachit-neytralnyiy-jir-v-koprogramme-diagnostika
Steatorrhea and its types
Neutral fat in feces is a pathological condition. Depending on the etiology, the following types of steatorrhea are distinguished:
- Intestinal type. Due to certain reasons, lipids are not absorbed in the intestinal tract, but are released with feces.
- Alimentary type. The basis of this pathology is poor nutrition. With food, the human body enters a huge amount of phospholipids, which are not able to be absorbed in full.
- Pancreatic type. Occurs as a result of disturbances in the functioning of the pancreas. There is a decrease in the synthesis of lipase, the enzyme responsible for the normal breakdown of lipids.
Steatorrhea also differs in the variety of components. Stool may contain significant amounts of neutral fats (triglycerides), soap and fatty acids, or all three.
Decoding the coprogram of feces in an infant
A coprogram is a general examination of stool and is necessary to determine the functioning of the gastrointestinal tract and liver of children.
Decoding the results shows information about the presence of parasitic organisms or inflammation in the body in children.
Special attention is paid to collecting the material for analysis correctly, as this directly affects the accuracy of the results.
Analysis collection rules
If the biomaterial was collected incorrectly, the study will give false indicators. Therefore, when collecting analysis, the following recommendations should be taken into account.
- It is necessary to use a sterile container sold in a pharmacy.
- Before collecting material, such a container should not be washed or wiped.
- At least 2 tsp must be provided for analysis. feces
- The material should be collected from a clean diaper, and not from a diaper, as it will absorb the liquid necessary for the study.
- You need to bring the biomaterial to the laboratory for coprogram in fresh form. It can be stored in a closed container for no more than 8 hours.
- It is necessary to ensure that there are no urine impurities in the stool.
- Defecation should be natural, and material obtained through an enema or laxatives is not suitable.
Preparing for analysis
In order for the result to reflect reality as much as possible, the analysis must be collected after proper preparation.
- 2 days before the test, you should stop taking medications that affect the child’s stool.
- The day before the test, it is necessary to limit the consumption of meat, fish, vegetables, fruits and herbs.
- 4 days before the analysis, the basis of nutrition should be cereals, eggs, fermented milk products, bread and butter.
For a few days it is strictly prohibited:
- use of rectal suppositories;
- the use of substances that color the mass of feces;
- the presence of allergenic foods on the menu, as well as foods with simple carbohydrates and high fat content;
- smoking and drinking alcoholic beverages.
It is allowed to eat steamed cutlets, vegetable soups, liquid porridges made from rice and oatmeal. A nursing mother should also adjust her diet.
If you follow all the rules, you can be sure that the coprogram will show the results correctly.
Indicators
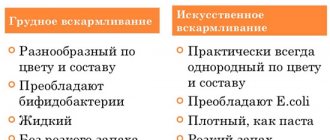
The norm is different for infants compared to older children. The interpretation of the analysis also takes into account the child’s nutritional type.
- For children fed with breast milk, the amount of feces per day should be 40-50 g of a porridge-like consistency of yellow-green or golden color, and for those fed with a formula - 30-40 g of yellow-brown color and putty-like condition.
- The normal fecal acidity for babies fed on breast milk is 4.8-5.8 with a sour odor, and for bottle-fed babies it is 6.8-7.5 with a putrid odor.
- Protein, blood and mucus, as well as ammonia, fiber and starch should be absent in infants.
- Stercobilin and bilirubin should be present in stool.
- Muscle fibers, neutral fats, fatty acids, and soaps may be present in small quantities. The norm also determines that leukocytes in children can be present in small quantities.
- If the analysis shows the presence of red blood cells, you need to urgently consult a doctor, who will determine their number and tell you whether this is normal or not.
Meaning of indicators
If the resulting transcript does not correspond to the norm, this indicates disturbances in the functioning of the child’s gastrointestinal tract or an ongoing illness.
- If the volume of feces does not match, this warns that the baby is prone to diarrhea or constipation. Its density shows the volume of fluid in the stool: with high fluid levels, increased secretion occurs, with medium levels - loose stools and colic, with low levels - constipation and intestinal spasms.
- The diet of the baby or mother affects the color of children's stool. The norm does not allow the presence of black or dark brown color, which indicates putrefactive processes in the body. An exception is taking iron-containing medications. Green indicates increased peristalsis, and red indicates ulcerative colitis. If whitish shades occur, you should sound the alarm, as they are a consequence of hepatitis and pancreatitis . The norm can be represented by green discharge if it appears in the first 4 months of the baby’s life.
- Acidity analysis helps determine the quality of the microflora: with a high level, fermentation takes place in the body, and with a low level, a putrefactive process takes place.
- Only a coprogram can detect red blood cells and blood in the stool. The norm does not imply their presence in the mass, which indicates polyps or bleeding. Sometimes in healthy children the analysis reveals red blood cells, but their norm will be in the range of 2 to 3 units. However, even with such indicators, it is necessary to see a doctor.
- There should be no protein in the biomass. Protein present in the results indicates inflammation and digestive difficulties.
- If mucus is present in infants who are exclusively breastfed and under 5 months, this is normal. Also here you should pay attention to the content of leukocytes: normally they are absent or there should be a minimum number of them.
- If, before the introduction of complementary foods, the analysis shows the presence of starch or fiber, this indicates poor absorption of food by the baby.
- Fatty acids appear during a disease accompanied by putrefactive dispersion, and neutral fats appear when the functioning of the gallbladder or pancreas fails. If the analysis reveals fatty acids or neutral fats in the test material, you should consult a doctor as soon as possible.
- Increased intestinal motility is manifested by the presence of bilirubin in the stool. Determining bilirubin only for children under 8 months is the norm.
- The absence of soaps in children indicates dispersion.
- The norm dictates that an increased number of leukocytes can signal colitis, dysentery or hemorrhoids.
- Stercobilin first appears in the analysis when positive beneficial microflora is established in the baby’s intestines - by about 5-6 months of life. Therefore, in infants up to 5 months of age, stercobilin is absent in the feces. In children under 8 months of age who are breastfed or bottle-fed, stercobilin should already be detected. At 8-9 months, the analysis will normally show only stercobilin, and bilirubin will be absent. Thus, stercobilin gradually replaces bilirubin in the child’s body.
Stercobilin, present normally, is characteristic of healthy children. If stercobilin is shown in reduced quantities, this may indicate diseases such as:
- obstructive jaundice;
- inflammation of the bile ducts;
- hepatitis.
If stercobilin is not detected, this indicates underdeveloped bile ducts or their complete blockage. In this case, you should pay attention to the age of the baby.
If stercobilin is present in increased quantities, this indicates:
- hemolytic anemia;
- excessive secretion of bile;
- increased spleen function.
Due to the collection of material for a coprogram, the doctor may recommend special preparation in order to carry out the analysis correctly and obtain accurate results. The analysis needs to be deciphered only by a pediatrician, who, if necessary, can prescribe effective treatment for the baby.
Source: https://grudnichky.ru/zdorove/koprogramma-kala-rasshifrovka-u-grudnichka.html
Causes of pancreatic steatorrhea
Neutral fat in the feces of a child or adult can appear against the background of a number of abnormal conditions.
1. Diseases of the pancreas:
- acute pancreatitis during the first six months;
- inflammation of the pancreas lasting more than six months (chronic process);
- narrowing of the Wirsung duct (through which pancreatic juice enters the duodenum);
- Solinger-Ellison syndrome is a tumor process that results in ulcerations of the stomach and intestinal tract.
2. Liver pathologies:
- hepatitis of acute and chronic nature;
- hepatitis resulting from alcohol abuse;
- cirrhosis of the liver;
- cholangitis of the sclerosing type - an inflammatory disease of the intrahepatic bile ducts, which is accompanied by the formation of scars;
- hemochromatosis is a disorder of metabolic processes associated with iron, which is accompanied by its pathological accumulation in the body;
- liver amyloidosis;
- tumors and cysts.
3. Pathology of the gallbladder and ducts:
- cholelithiasis;
- inflammation of the gallbladder, acute and chronic;
- cholangitis - inflammation of the bile ducts;
- infection of the biliary tract with Giardia.
Features in children
Steatorrhea in children develops somewhat differently than in adults. To a greater extent, the causes of this condition in a child are a lack of pancreatic enzymes and the general immaturity of the enzyme system.
Enzymes that take part in lipid metabolism in a newborn begin to be produced in sufficient quantities only when the child reaches 3 months. Until this time, there will be inadequate digestion of fats. What is not considered pathological.
But at the same time, salts of fatty acids in the feces of an infant can be detected even if the liver is not functioning properly. This is in most cases due to genetic disorders. They can be both metabolic and structural in nature.
As for weakened infants, their normal metabolism (metabolism, including fat) is established a little later - by 4-5 months of life.
Causes of intestinal steatorrhea
Neutral fat in the coprogram with intestinal type pathology can occur as a result of the following conditions:
- with Crohn's disease - chronic inflammation of the intestinal tract, in which narrowing and ulceration develop;
- with Whipple's disease - a disease of the intestines and regional lymphatics of an infectious nature;
- with intestinal lymphoma - a tumor that consists of lymphocytes;
- in post-resection condition;
- with enteritis, enterocolitis;
- with amyloidosis;
- with diverticulosis - a pathological process accompanied by the formation of diverticula (protrusions) in the intestinal wall.
Other etiological factors
The causes of the appearance of phospholipids in feces may be diseases of the endocrine glands. The most common provoking factors are hypothyroidism and Addison's disease (adrenal insufficiency).
Abetalipoproteinemia (impaired absorption and transport of lipids), cystic fibrosis (the secretions of all glands are highly viscous and thick) and cealkia (a disease in which gluten is not completely broken down) are congenital conditions that lead to the appearance of neutral fat in the feces of infants.
The appearance of phospholipids in feces can accompany psoriasis and eczema, as well as long-term use of laxatives and drugs used for weight loss.
Reasons for the content of fatty acids and neutral fats in feces
Reasons for insufficient absorption of fatty acids by the body:
- dysfunction of the pancreas . To break down neutral fats in the intestines into glycerol and fatty acids, the pancreas synthesizes a water-soluble enzyme - pancreatic lipase. A decrease in the activity of the pancreas leads to a deficiency of lipase in the body and a disruption of its digestive action. In this case, triglycerides cannot be completely broken down, neutral fat appears in the feces;
- Bile acid deficiency . Insufficient flow of bile into the intestines leads to impaired breakdown and absorption of fats. Fats are accessible to digestive enzymes only in the form of a thin emulsion. Bile performs the function of mixing fat masses with water, which is necessary for their digestion. If there is a lack of bile, the fat droplets remain so large that aqueous solutions of enzymes cannot mix with them. As a result, fats are not completely digested and are found in feces;
- malabsorption (malabsorption) of fat in the intestine and accelerated evacuation from the rectum. The movement of the food bolus (chyme) occurs due to wave-like contractions of the intestinal walls. Violations of its motor function, accelerated movement and evacuation of food masses from the intestines lead to the fact that fats do not have time to be completely absorbed. As a result, the general appearance of feces changes, they acquire a light, grayish tint, a greasy sheen and an unpleasant odor that is not typical for them;
- excessive fat content in the diet , especially refractory fat (for example, lamb fat);
- taking castor oil and using rectal suppositories;
- a large amount of fatty components with impaired patency of the lymphatic ducts.
Absorption of fat-soluble vitamins occurs predominantly in the small intestine, therefore, in pathological conditions accompanied by atrophy of the mucous membrane of the small intestine, the process of their assimilation is disrupted.
Digestion, absorption disorders and constant loss of fat lead to a decrease in serum levels of all lipid components, primarily cholesterol and fatty acids.
The causes of disorders of fat metabolism and the appearance of fatty acids in feces can be diseases of the small intestine (ulcerative colitis, Crohn's disease, enteritis), liver pathologies (hepatitis, cystic fibrosis, cholecystitis), cholestasis, dyskinesia of the gallbladder and biliary tract, pancreatic insufficiency, chronic alcoholic pancreatitis, cardiospasm. The appearance of fatty acids in feces is characteristic of celiac disease, pancreatogenic malabsorption syndrome, biliary dysfunction, enterokinase deficiency, excessive colonization of the small intestine by bacterial microflora, and conditions after resection of the small intestine. The mechanisms responsible for digesting fats can be affected by certain medications. The syndrome of accelerated evacuation of intestinal contents can be observed after excessive use of laxatives and anti-obesity drugs.
Clinical picture
The first manifestation of the pathology is a frequent urge to defecate. Feces are oily and difficult to wash off the surface of the toilet. Feces leave a greasy residue. The color of stool may remain normal, or it may change towards a light or gray shade.
In addition, neutral fats, which contain fatty acids and glycerol, appearing in the feces can also be reflected in the following symptoms:
- dry cough;
- dizziness;
- joint and back pain;
- bloating;
- low level of performance;
- weakness;
- dry mucous membranes;
- exhaustion;
- bleeding gums.
The appearance of oily stools and at least one of the accompanying symptoms is a reason to seek qualified help.
Diagnostic measures
The collection of complaints and anamnesis is accompanied by clarification of when the symptoms appeared, what the patient associates with their occurrence, when the stool acquired an oily character. The specialist clarifies the presence of congenital diseases or inherited pathologies among the patient’s relatives. Next, the doctor examines the patient. The presence of exhaustion, the condition of the skin and mucous membranes are determined, and palpation and percussion of the abdominal organs is performed.
Coprology (laboratory examination of stool) consists of assessing the following indicators:
- Macroscopy - steatorrhea manifests itself in the form of lighter-colored stools with the sheen of frozen fat.
- Microscopy determines the presence of lipids, fatty acids, and soap. Normally, no more than 5 g of neutral fat should be excreted in stool within 24 hours. The results above are pathological.
If necessary, a radioisotope study, ultrasound examination of the abdominal organs, colonoscopy, assessment of the hormonal balance of the body, consultation with an endocrinologist and therapist are used.
Diagnostic methods
First of all, the specialist collects an anamnesis. It is determined when the greasy sheen of stool appeared, how much is released per day, what symptoms bother the patient. It is also important to find out whether the patient has any chronic or hereditary diseases, whether he has taken any medications for a long period, whether he has had contact with toxic substances, etc.
The doctor assesses the condition of the organs involved in fat processing. For this, the patient is examined and palpated on the left side of the abdomen. Using tapping, the sizes of the spleen, liver and pancreas are determined.
The method of macroscopic examination (visual assessment) of stool helps to determine the pronounced oily character. Often, the stool is liquid and light-colored—much lighter than normal. Laboratory analysis of stool can reveal excess fats, soaps and fatty acids.
If it turns out that 7 g or more fat is excreted in the stool per day, the doctor diagnoses steatorrhea.
If you find soap in your stool, you should not panic, since the presence of this substance is normal and indicates normal functioning of the gastrointestinal tract. The presence of fatty acids in feces in small quantities may be the norm for breastfed and bottle-fed children, while for older children and adults this is considered a pathology.
A more accurate method is radioisotope research. It allows you to find out the cause of disorders in the breakdown and absorption of fats. Its essence lies in the introduction of radioactive isotopes into the digestive tract.
To make a diagnosis, a specialist may prescribe a fat loading technique. Based on the results obtained, diseases of the pancreas or intestines can be excluded.
Additional methods may include ultrasound of the abdominal organs, colonoscopy, determination of hormone levels, and consultation with other specialists. The results of these studies will help clarify the diagnosis.
Elimination of steatorrhea
First of all, treatment is aimed at the disease that caused the appearance of neutral fat in the stool. Individual selection of diet is also carried out based on the underlying pathology. It is mandatory to exclude fried, pickled and smoked foods.
The patient must stop drinking alcoholic beverages and get rid of bad habits. It is recommended to add to the diet those foods that contain significant amounts of retinol, tocopherol, calciferol and vitamin K. These same fat-soluble vitamins are prescribed in the form of medications.
Complications and consequences
Complications develop only if treatment is not started in a timely manner. There is a disruption in the absorption of nutrients in the intestinal tract. Against this background, hypo- and avitaminosis, protein deficiency and exhaustion of the body develop. Pathology of water and electrolyte balance is manifested by a constant feeling of thirst, edema, dehydration, and convulsive attacks.
The specialist diagnoses the appearance of oxaluria (excessive pathological excretion of oxalic acid salts from the body along with urine) and the formation of urinary stones of oxalate origin. This pathological condition occurs because, under normal conditions, oxalates do not enter the blood from the intestinal tract, since their combination with calcium makes them insoluble. With the development of steatorrhea, calcium is excreted in large quantities from the body along with feces. This leads to a significant release of oxalates from the intestines into the blood.
The patient loses body weight quite sharply. The normal functioning of all internal organs and systems is disrupted. Such manifestations lead to psychological problems (insomnia, changes in communication, decreased performance).
How is a patient examined?
Among the most reliable studies, experts highlight laboratory tests (coprogram). Using tests, the level of content in the stool is examined:
Why does my stomach hurt after defecation?
- fatty acid;
- a lot or a little soap;
- triglycerides.
In cases where the analysis shows a level of total fat mass in stool exceeding 5 g, we can talk about the presence of steatorrhea. To make a correct diagnosis and prescribe treatment, it is enough to take tests to the laboratory. The specialist, in turn, examines the patient and assesses his general condition. During the conversation, the specialist takes an anamnesis of the disease.
During the examination of the patient, the abdomen is palpated. As a rule, palpation causes increased rumbling or a sensation of fluid transfusion in the left side of the abdomen. If it is necessary to complete the picture, the doctor will prescribe an x-ray examination. In the future, the functioning of the organs is studied and a referral for a biopsy is issued.
Before prescribing medications, it is necessary to undergo a macroscopic and microscopic assessment of the contents of stool. Having received the test results, the doctor calculates the amount of fatty acid, soap and neutral fat in the stool and prescribes appropriate therapy. Timely treatment of the disease will help avoid the development of a number of serious conditions, namely:
- leukopenia;
- hypolipemia;
- hypochromia, etc.
In advanced forms of the disease, fatty acids in feces may cause complications:
- disruption of the functioning of internal organs and systems;
- development of hypovitaminosis;
- violation of water-salt balance;
- lack of protein in the body;
- decreased performance;
- the appearance of mental disorders.
By treating the disease at the initial stage, you can completely get rid of the disease.
The coprogram will help you find out the level of fatty acid content
Preventive measures
Preventive measures can be divided into primary and secondary. Primary prevention is carried out to prevent the disease from appearing. It is based on preventing the development of pathologies in which steatorrhea becomes one of the symptoms. The important points are:
- cessation of smoking and excessive consumption of alcoholic beverages;
- correction of diet;
- increasing the amount of plant food consumed;
- fractional meals in small portions;
- use of multivitamin complexes;
- strengthening the body's defenses.
Secondary prevention (after the onset of the disease) is based on timely, rational treatment of the pathological condition.