The human body is an integral system that works only under the condition of coordinated functioning of organs under the strict control of nerves, hormonal substances and other regulatory mechanisms. If one of the parts of the whole breaks down, the operation of another component of the system is disrupted.
With pancreatitis, a direct or indirect effect on the functioning of the heart is possible. Sometimes cardialgia is difficult to distinguish from symptoms of inflammation of the pancreas tissue. Only a doctor can distinguish between symptoms and answer the question of whether the pancreas can radiate to the heart.
Cardialgia and pancreatitis
These conditions are rarely found together. But one disease often masks the manifestations of another.
It’s difficult to say which is more dangerous - pancreatitis or heart pain. Both situations require emergency care in a specialized department.
Heart pain, called cardialgia, according to the observations of modern doctors, extremely rarely has typical characteristics.
These include:
- localization: behind the sternum;
- irradiation: to the area of the left shoulder girdle, scapula, shoulder, hand, lower jaw;
- conditions of occurrence: during physical activity;
- response to therapy: positive dynamics while taking nitroglycerin and other nitro group donors.
Increasingly, the pain syndrome does not bother the chest, but has atypical localizations. You should not be sure, for example, that girdle pain is a typical manifestation of inflammation of the pancreas. Probably, the described clinical symptoms manifest an atypical form of angina or even myocardial infarction.
Cardialgia or pancreatitis: only a doctor can answer
The pancreas radiates to the heart quite often. Heart pain and pancreatitis must be differentiated at the prehospital stage. Without laboratory and instrumental research methods, it is difficult to distinguish between these pathological conditions. It is necessary to register an electrocardiogram, draw blood to determine amylase, creatine phosphokinase, troponin, myoglobin, aspartate aminotransferase, alanine aminotransferase, and a urine test for diastase.
Pancreatitis and heart pain are observed together in a patient when the patient has previously had angina pectoris. Inflammation of the pancreas is a powerful trigger and stress factor for a heart patient. The inflammatory process can provoke aggravation of angina pectoris and cause progression of the disease.
Pain in the heart during pancreatitis does not exclude the latter, even if the electrocardiogram reveals signs of angina pectoris or myocardial infarction. This situation is more difficult to treat. It is necessary to involve a surgeon and cardiologist in the treatment process. Complex etiopathogenetic therapy is carried out. Pancreatitis and angina pectoris are an interdisciplinary problem; they are solved individually.
Treatment methods
Treatment of conditions manifested by “pulsation in the stomach” depends on the presence of the disease and the severity of its course. During the treatment period, it is recommended to minimize physical and psycho-emotional stress; it is necessary to follow a strict diet - gas-forming foods are excluded from the diet: fried foods, legumes, dairy. It is recommended to eat frequently in fractional portions (up to 200 grams).
Pain in the heart area is one of the main companions of cardiac pathologies. However, in many cases where there are no cardiac problems, chest discomfort may be due to irritation of the intercostal nerves. This disease is called intercostal neuralgia, and pain in the heart area is called cardialgia.
Due to the similar location and intensity, an attack of thoracic neuralgia is often mistaken for a manifestation of heart disease. Typical symptoms for neuralgia are:
- severe sharp or dull, burning or aching paroxysmal pain in the left side of the chest;
- pain when inhaling, when changing position, sneezing, coughing, a feeling of squeezing of the ribs;
- sometimes - muscle twitching, redness or paleness of the skin, tingling in the chest, numbness of the skin between the ribs.
Despite the similarity with cardiac pathologies, neuralgia is easy to distinguish by the following characteristics:
- With neuralgia, the pain intensifies when inhaling, changing body position, palpating the ribs and the spaces between them. With angina pectoris, additional factors do not affect the nature of the pain.
- The pain with neuralgia is girdling in nature and can radiate to the shoulder blades, lower back, and subclavian region. In addition, it lasts several hours, or even days. Pain in cardiac diseases is localized in the center of the chest region and, as a rule, lasts 5–10 minutes. Sometimes it goes to the left hand.
- Heart pain, if it is not caused by myocardial infarction, is relieved with Nitroglycerin. Neuralgic pain does not go away with heart medications, but relief may occur with sedatives.
- Intercostal neuralgia does not affect pulse and blood pressure, unlike cardiac disorders.
At the same time, we should not forget about the individual characteristics of each patient. In some cases, pain sensations can be difficult to characterize, so self-diagnosis if neuralgia is suspected is impossible. In addition, a condition as dangerous and requiring immediate assistance as myocardial infarction is often manifested by sharp, severe pain that intensifies with movement, and it is sometimes impossible to distinguish it from neuralgia. A heart attack requires urgent medical attention.
If the pain radiates to the lower back or hypochondrium, you may need to check for diseases of the urinary and digestive systems. In combination with digestive pathologies, neuralgia intensifies in the supine position and is localized in the lower region of the sternum. At the first stage of diagnosis, blood and urine tests will help to distinguish neuralgia from diseases of the kidneys, liver, and pancreas. With intercostal neuralgia, they do not show deviations from the norm.
When diagnosing neuralgia, the doctor is guided not only by a physical examination, but also by the results of additional studies:
- electrocardiograms (ECG);
- chest x-ray;
- general blood test, urine test;
- myelography - an x-ray study with contrast that allows you to assess the condition of the nerve roots.
The diagnosis of neuralgia assumes normal results of the first three studies and a difference from normal results with myelography.
The main reason for the occurrence of chest pain is irritation and compression of the roots of the intercostal nerves, occurring due to muscle spasm. This is preceded by both pathological and physiological factors:
- diseases of the musculoskeletal system: osteochondrosis, spondylitis, ankylosing spondylitis, intervertebral hernias, kyphosis, perichondritis, osteophytes of intervertebral joints, myositis, myalgia, pectoralis major syndrome;
- benign and malignant tumors of the sternum, spine, spinal cord;
- neurological diseases: demyelination of nerve fibers, radiculitis, multiple sclerosis, neuritis;
- infectious diseases: influenza, herpes, herpes zoster, tuberculosis;
- metabolic disorders: diabetes mellitus, salt deposition in the spine;
- diseases of the digestive system: cholecystitis, pancreatitis, gastric ulcer, hiatal hernia, cholangitis;
- chest injuries, bruises;
- uncomfortable position during sleep, work;
- strenuous physical work;
- hypothermia, being in a draft;
- chronic intoxication;
- deficiency of B vitamins;
- psycho-emotional disorders: stress, chronic fatigue.
Due to the large number of causes of cardialgia, pain can be difficult to get rid of. However, there is no universal technique for all patients. For some, drug treatment is a more effective method, for others - physical therapy. For some, pain in the heart area is so mild that it is easier for people to endure.
Medicines for the treatment of pain in the heart:
- non-steroidal anti-inflammatory drugs: Ketorolac, Nimesulide, Ibuprofen, Indomethacin;
- antispasmodic: Drotaverine, Papaverine;
- painkillers: Baralgin, Analgin;
- B vitamins.
In case of severe pain, the patient is prescribed bed rest (the mattress should be thin and hard) and intramuscular injection of Novocaine.
Warming ointments and gels, which contain turpentine, bee venom, pepper extract, capsaicin, and camphor, help relax muscles and increase blood flow to the affected area. To enhance the effect, after applying the product, you need to wrap your chest in a blanket or put on a sweater.
Physiotherapy methods are widely used that warm up tissues, relieve spasms and dull pain:
- acupuncture;
- vacuum therapy;
- magnetic therapy;
- infrared and ultraviolet irradiation;
- electrophoresis with Novocaine;
- ultra-high frequency therapy (UHF);
- massage;
- dosed physical education.
For mild cardialgia and for prevention, it is possible to use herbal remedies that have a general strengthening, mild analgesic and sedative effect:
- compresses from steamed flax seeds;
- immortelle infusion;
- alcohol tincture or ointment with bodyaga;
- decoctions of barberry, lemon balm, chamomile, rose hips;
- infusion of valerian with the addition of orange zest;
- baths with the addition of sage decoction.
In some cases, for example, with herniated vertebral discs, it is impossible to cope with neuralgia using conservative methods. In this case, the problem is solved surgically.
Intercostal neuralgia is a disease characterized by cyclicity: under the influence of a number of factors, pain can return. To prevent this from happening, patients are advised to:
- avoid hypothermia, drafts, sudden movements;
- do swimming, stretching, yoga, dancing;
- get plenty of rest and avoid stress;
- don't carry heavy things.
The symptoms and treatment of atherosclerosis are complex. The disease can affect the arteries of various organs - the brain, heart, kidneys, lower, upper extremities, etc. Therefore, the signs of atherosclerosis can vary greatly.
But often patients complain of pain in the sternum, increased blood pressure, general weakness, and goosebumps.
Therapy for the pathology includes taking medications (statins, fibrates, nicotinic acid, FA severstants) and following a special diet. In more severe cases, surgery is performed.
The greatest role in the deposition of atherosclerotic plaques is played by reasons such as impaired lipid metabolism, hereditary predisposition and the state of the vascular structure.
Cholesterol is an important lipid (fat) in the human body. Being a building material, it is an integral part of vitamins and hormones. It is mainly produced by the liver (70%), and the remaining 30% enters the body with food.
In the human body, lipid is part of lipoproteins. They transport it from the liver to the cells, and if there is an excess amount, from the cells back to the liver. When this process is disrupted, atherosclerosis occurs, characterized by the accumulation of cholesterol plaques and growths on the walls of the arteries.
Depending on which arteries are affected, atherosclerosis is distinguished between cardiac and renal vessels, brain, aorta, upper and lower extremities. Forms of the disease can manifest themselves either individually or systemically.
Modifiable factors are:
- inactive lifestyle;
- excessive alcohol consumption;
- long history of smoking;
- unbalanced diet;
- arterial hypertension;
- abdominal obesity;
- elevated cholesterol levels;
- diabetes mellitus of any type.
Non-modifiable items include:
- age (male {amp}gt;45 years, female {amp}gt;55 years);
- gender (men are much more likely to suffer from atherosclerosis);
- genetic predisposition.
Most of these factors are corrected independently, so a person can prevent the development of such a serious disease and its complications: the formation of blood clots and rupture of atherosclerotic plaques.
Many patients ask the question, sclerosis and atherosclerosis - what is the difference? Atherosclerosis is a pathology in which there is a violation of lipid and protein metabolism, as a result of which growths and plaques are deposited on the walls of blood vessels.
The initial signs of atherosclerosis are hidden. The disease is characterized by a preclinical and clinical period. Moreover, symptoms do not appear until the lumen of the vessels is blocked by more than 50%.
How to distinguish between heart pain with angina and referred pain with pancreatitis
It is extremely important to correctly collect anamnestic data. It is important for the doctor whether there were such pains before, how long they lasted and under what conditions they were relieved. Half of the correct diagnosis lies in adequately posed questions and honest answers from the patient.
Coronary heart disease is supported by pain that occurs during exercise. But sometimes they can bother you even at rest, especially in severe forms of angina. Here it is necessary to find out what helps in this case. A Nitroglycerin tablet or a dose of nitrospray, which improves well-being, indicates myocardial ischemia.
When pain in the chest was provoked by a heavy meal, it is necessary to assume pancreatitis, despite the anginal localization.
Many diseases can spread to the heart area, including inflammation of the pancreas. Previous episodes of similar pain associated with alcohol consumption or arising from an error in diet will speak in favor of pancreatitis.
It is difficult to objectively identify signs of cardiac muscle ischemia. But you can suspect manifestations of pancreatitis. To do this, palpate the area of the costosternal joints. If there is pain in the area of the left second or third joint, inflammation of the pancreas is likely.
Next, Kutch and Mayo-Robson syndrome are examined. Examination of the area of the transverse processes of the 8th, 9th, 10th and 11th thoracic vertebrae gives pain in acute pancreatitis. This is Kach's symptom. In Mayo-Robson syndrome, pain is detected by palpation of the left costovertebral angle. These signs are quite specific for pancreatitis. Especially, together with peritoneal symptoms, negative in the presence of angina.
Mayo-Robson point for pancreatitis
Can the pancreas give to the heart?
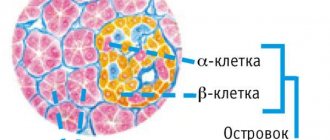
The pancreas is an organ that plays an important role in the digestion process. It is responsible for the production of digestive enzymes. Pancreatic hormones regulate blood sugar levels and are involved in many important processes.
With pathologies of this organ, a person often experiences painful sensations. Sometimes they are very intense, patients complain of pain on the left, characteristic of heart pain.
In this case, it is necessary to answer the question, are we talking about heart pathology or are these pains the result of inflammation in a neighboring organ? Can the pancreas give to the heart?
Angina and heart attack under the guise of pancreatitis
Often, symptoms of pancreatic inflammation may hide problems with other organs, such as the heart. The heart is in close proximity to the pancreas, and in pathological conditions such as heart attack or angina, it can be difficult to determine the source. With these diseases, pain appears, radiating to the back and left shoulder.
Myocardial infarction
This is a dangerous, life-threatening condition. The danger also lies in the fact that for a long time it can be asymptomatic, and manifest itself only as pain in the abdomen or left arm. These referred pains are taken, in particular, for pancreatitis, as well as other diseases.
Pain in the area of the stomach and pancreas is manifested by the so-called abdominal infarction, which is a rather rare form of heart pathology.
In such cases, taking stomach medications (antacids and antispasmodics) does not bring significant relief. This means that the reason must be sought in something else.
During myocardial infarction, pain develops progressively and reaches a peak within an hour. Taking nitroglycerin brings some relief.
The appearance of pain is usually associated with great physical and psycho-emotional stress. Sometimes they occur after a heavy meal and may be accompanied by vomiting.
Angina pectoris
A very common disease, which is based on insufficient blood supply to the heart muscle. With angina, painful sensations vary in nature and intensity. They are usually localized behind the sternum.
In some cases, referred pain appears in the epigastric region. They can be mistaken for a manifestation of acute pancreatitis or peptic ulcer of the stomach and duodenum. In this case, nausea often appears, turning into vomiting.
Various pathologies of the gastrointestinal tract may be accompanied by increased secretion. Excessive production of hydrochloric acid causes:
- nausea;
- heartburn;
- belching sour;
- epigastric pain.
These unpleasant symptoms are explained by insufficient production of digestive enzymes, which is typical for many gastrointestinal diseases, in particular pancreatitis. Such symptoms will allow the specialist to most likely exclude heart pathology.
With biliary dyskinesia and cholelithiasis, sharp, cramping or dull, aching pain appears in the right side. Problems with the gallbladder are a very common cause of chronic pancreatitis.
With angina pectoris and heart attack, pain occurs in the heart, radiating to the left side of the body. However, these symptoms are not always associated specifically with heart disease. Chest pain causes diseases of the musculoskeletal system, disorders of the digestive and respiratory systems. In any case, only a specialist can make an accurate diagnosis after conducting the necessary research.
Does the pancreas affect the heart?
The most important organs of the digestive system - the liver, stomach and pancreas - are located in the abdominal cavity in close proximity to the heart.
Consequently, any pathology of these organs can negatively affect the heart.
In medical practice, there are quite frequent cases of patient requests regarding complaints of pain in the heart, the cause of which is diseases of the digestive organs, in particular the pancreas.
Acute pancreatitis (inflammation of the pancreas), like myocardial infarction, is a serious pathology. If not treated promptly, the patient's condition becomes critical and can result in death. In the acute form of pancreatitis, the pain is sharp and cramping.
The pancreas is located behind the stomach and slightly to the left. This can explain the nature of the pain radiating to the heart and left hypochondrium in acute pancreatitis. Often the pain that occurs with this pathology spreads upward, to the region of the heart, and radiates to the left shoulder blade.
Diseases of the pancreas are not the only cause of pain in the heart area. Gallstone disease may not manifest itself for a long time.
But sooner or later, especially after intense physical activity or due to stress, gallstones begin to make themselves known.
Biliary colic appears, accompanied by arrhythmia and shortness of breath, which are characteristic of cardiovascular pathology.
When pain in the chest was provoked by a heavy meal, it is necessary to assume pancreatitis, despite the anginal localization.
When diagnosing, the doctor pays attention to atypical manifestations of gastrointestinal diseases.
For example, gastroesophageal reflux (heartburn) is often accompanied by heart rhythm disturbances and chest pain.
According to some reports, this pathology is one of the most common causes of chest pain, along with coronary heart disease.
Tachycardia
Another complication of inflammatory processes in the pancreas can be tachycardia, or rapid heartbeat. In acute pancreatitis, tachycardia can be caused by a fever or pain syndrome, which is accompanied by a high level of stress.
Also, tachycardia is often a consequence of low blood pressure, characteristic of acute pancreatitis. In general, tachycardia is a serious condition that requires immediate attention.
It may be accompanied by acute lack of air, dizziness, even loss of consciousness.
First aid and treatment for heart pain
In all pathological conditions, it is necessary, first of all, to relieve pain with the help of antispasmodic intramuscular drugs, such as Papaverine or Platiphylline.
Then, once the diagnosis is made, medications are prescribed to treat the pancreas. The most important condition for inflammation of the pancreas is to temporarily provide a state of rest for this organ using enzyme replacement therapy.
For patients with pancreatitis, it is important to follow a strict diet that excludes fried foods and high-fat foods.
Heart rhythm disturbances
Chronic inflammation of the pancreas tissue usually does not affect the condition of the heart in any way. But with an exacerbation of the disease or during acute pancreatitis, rhythm and conduction disturbances are possible. How can one explain their appearance?
The most common type of arrhythmia is tachycardia. This is a rapid heartbeat that the patient feels. The pulse is higher than normal - more than 90 beats per minute. Tachycardia occurs from a reflex effect. There are close relationships between the conduction system of the heart and the abdominal organs. They are realized when they are pathological. In the case of pancreatitis, there may be pancreatic-cardiac syndrome, similar to gastrocardial or cholecystocardial syndrome.
Arrhythmia often accompanies inflammation of the pancreas
Another possible mechanism is typical for severe forms (when complications of pancreatitis occur). The pain in the stomach radiates to the heart. Tachycardia with pancreatitis is explained by the body's inflammatory reaction. This is especially clearly noticeable when the temperature rises to subfebrile or febrile levels. There are 10 beats per minute per degree. But the pulse with pancreatitis can reach 120-130 beats per minute. Blood pressure changes in a friendly manner. There is a tendency to hypotension, although initially blood pressure rises. Perhaps the cause of the disorder is nicotine addiction.
Effect of the pancreas on the heart
The main organ in the cardiovascular system is the heart. This cone-shaped muscular organ can work automatically and at the same time performs an important function - it pumps blood throughout the body. The close location of the heart to the pancreas and stomach contributes to the fact that various inflammatory processes of these organs contribute to changes in cardiac activity.
The main cardiac disorders in pancreatic pain:
- Tachycardia - rapid heartbeat
- Extrasystole is an extraordinary contraction of the myocardium.
The features of the structure and equipment of the pancreas were indicated above. All this confirms the complexity of the organization of the organ and the importance of the influence it has on the entire body as a whole and on the heart in particular. Since with pancreatitis the first thing that worries the patient is pain, it is its presence and severity that significantly affects the functioning of the heart.
Pain causes an increase in blood pressure and heart rate by two main mechanisms that can act simultaneously.
- The sympathetic (autonomic) nervous system is stimulated through electrical pain signals that reach the central nervous system. This often occurs with acute pain, exacerbation, but can also occur with chronic pain. Aberrant neuroanatomical changes in the brain that can occur with severe persistent pain are capable of producing continuous sympathicotonia. As a result, excitation of the sympathetic department leads to changes in heart rate and pressure.
- When pain occurs, signals are sent to the hypothalamus and pituitary gland, which promotes the release of the hormone adrenocorticotropin (ACTH), which stimulates the adrenal glands, which release adrenaline with a subsequent increase in heart rate and blood pressure.
The stronger the pain, the more pronounced the changes in the cardiovascular system may be. People who have previously been diagnosed with heart or vascular disease are especially susceptible to such disorders.
In such cases, the risk of myocardial infarction especially increases, since with severe pain the blood supply to the heart muscle is disrupted, which can lead to ischemia and necrosis.
If the pain does not go away for a long time, it is necessary to use suitable medications that may have been previously prescribed by a doctor. If this has not been done, then you should immediately contact a gastroenterologist, who will prescribe medications to eliminate pain due to pancreatitis, which will make it possible to normalize cardiac activity.
Symptoms of pancreatitis and tachycardia
A rapid pulse indicates a high degree of intoxication. At the same time, vomiting, nausea occur, and patients feel a rapid heartbeat.
It is worth remembering about emotional disturbances with inflammation of the pancreas. This is a rather serious stress factor for the human body. It makes an additional contribution to the development of cardiac rhythm and conduction disorders.
Pancreas and tachycardia may also be associated with developing dehydration. Diarrheal syndrome that develops with pancreatitis leads to loss of fluid and electrolytes. This will inevitably affect the heart rate. Extrasystole, sinus or nodal tachycardia may appear. These conditions are manifested by such symptoms as rapid heartbeat during pancreatitis, sensations of “fading” of the heart, and flickering of spots before the eyes.
The influence of the pancreas on the heart is realized with severe pain syndrome. Girdle pain can be very intense, because with pancreatitis necrosis (death) of part of the organ occurs. Painful sensations activate the sympathetic-adrenal system. At the same time, heart rate increases and blood pressure increases[/anchor]. Because of this, interruptions in the functioning of the heart occur.
Tachycardia with pancreatitis
The pancreas and the heartbeat are closely related structures, since with the development of acute pancreatic inflammation in the cavity of the parenchymal gland, the level of heartbeat begins to increase, exceeding the limits of 100 beats per minute. An increase in the rhythm of the heartbeat may affect the patient’s general well-being, or it may go unnoticed. In such situations, tachycardia is determined only by listening to the pulse and heartbeat.
The main reason for the development of tachycardia in pancreatic disease may be either an increase in temperature and the development of intoxication processes extending beyond the abdominal cavity, or a peculiar reaction of the body to developing pancreatic pain and disturbed psycho-emotional balance in the patient.
It is also worth noting that the development of tachycardia can occur with low blood pressure, which is a characteristic symptom in the acute form of pancreatic pathology, accompanied by the formation of painful shock.
Symptomatic signs of tachycardia appear:
- high heart rate;
- the appearance of a feeling of weakness throughout the body;
- lack of air;
- attacks of dizziness;
- sensations of possible loss of consciousness.
Extrasystole
Sometimes patients note the appearance of so-called extraordinary heart contractions. That is, the normal rhythm of the heart is interrupted by beats, which patients describe as special, early or late, untimely. We are talking about extrasystoles.
Frequent single ventricular extrasystoles
In diseases of the abdominal organs and retroperitoneal space, this type of cardiac arrhythmia is quite typical. The pancreas and heartbeat are usually connected.
The following mechanisms for the development of extraordinary cardiac contraction (extrasystoles) are distinguished:
- Changes in electrolyte composition with the development of hyperkalemia (increased serum potassium levels).
- Reflex influence from the pancreas (this is explained from the standpoint of common innervation).
- Intoxication syndrome.
- Emotional disorders (tendency to depression, anxiety).
The danger of extrasystoles in pancreatitis is due to the fact that they can cause more serious rhythm disturbances, especially with existing organic diseases of the heart muscle. Extrasystole acts as a trigger (triggering factor) for ventricular tachycardia, atrial fibrillation or flutter, which can be fatal.
We recommend reading:
- Symptoms of stones in the pancreas;
- Danger of parenchymal pancreatitis.
- Stones in the gall and pancreas.