Causes of disturbances in the formation of the gastrointestinal tract in the fetus, statistics
The content of the article
Anomalies in the structure of the gastrointestinal tract are associated with a violation of embryogenesis at the stage of 4-8 weeks of pregnancy, when the opening of the digestive tube is formed. Initially, it ends at both ends, but by the end of the 8th week, channels are formed, and the mucous epithelium closes the lumen of the intestinal tube. Among the most common pathologies are stenosis (narrowing or stretching of the walls) or atresia (fusion).
The duodenum suffers the most, which is due to the peculiarities of its embryogenesis. 1/2 of cases are accompanied by defects of other internal organs - heart, blood vessels, rectum, liver, stomach. Some cases are so severe that the baby will have to undergo many operations during his lifetime, and they will not guarantee his normal existence.
Abnormalities of the gastrointestinal tract are visible on ultrasound at 11 weeks. Ultrasound diagnostics is not a 100% guarantee that the baby will have serious abnormalities, so its results are the basis for a more detailed examination of the woman.
A pregnant woman undergoes karyotyping to detect chromosomal abnormalities. She also undergoes an amniotic fluid test, and based on the results of the examination (if they are bad and the diagnosis is confirmed), she is recommended to terminate the pregnancy
ultrasound shows enlarged fetal stomach
2009-12-11 19:37:16
Christina asks:
Hello! I was diagnosed as pregnant two weeks ago, at about 5 weeks. But upon admission, I had already been suffering from severe pain in the lower abdomen for two weeks. The diagnosis was as follows: Early pregnancy Cyst of the right ovary (This explained the pain) Ectopia of the cervix Tests were taken: Cytological examination of gynecological smears for atypia (cervix, cervical canal) Flora. An ultrasound was performed both by the doctor himself using a small conventional device, and by a specialist enlarged in a separate special ultrasound room. We found a cyst. A fertilized egg is detected in the uterine cavity. The average internal diameter of the ovum is 2.3 mm, which corresponds to no more than 5 weeks of pregnancy. The right ovary, 52.4 x 43.8 mm, contains an echogenic formation 45.1 x 38.2 mm with thin smooth walls (corpus luteum cyst?) The left ovary is 27.9 x 14.8 mm, of normal size and structure. A small amount of fluid behind the uterus. No volumetric formations were detected in the pelvis. visualization conditions: satisfactory Conclusion: Early uterine pregnancy. Therapy: Folio 1 t 1 time Utrozhestan 0.2 x 2 tablets intravaginally at night no-spa 1 t 3 times A week later, I was examined again by a doctor and his usual ultrasound. The doctor looked at the ultrasound and was upset, saying that the fetus was of irregular shape and deformed…. What she really didn’t like... The diagnosis at the conclusion: the same. Therapy is doubled (!!!) Folio 1t 1 time Utrozhestan 0.2 x 2 tablets Both in the morning and in the evening Injections with a solution of progesterone 1% -1.0 i.m. during the day for 10 days Papaverine suppositories in the anus in the morning and at night for 10 days Magne B6 1t x 3 times NO-Spa 1t x 3 times An enlarged ultrasound was prescribed after a week and examination. So many medications make my stomach cramp. With complaints that the chest has been hurting very much for the 4th week and it is simply impossible to touch it, they did not even examine it. The number of medications alarmed me... And the words that the fetus was deformed shocked me. But they didn’t even explain to me how dangerous it was and didn’t explain anything at all. Having made an appointment in a week... They gave out part of the finished tests, saying that they will explain everything as soon as the second part arrives in a week again... But on those that were issued, I can say that the conclusion says: Ecto- and endocervix: layers and cells of a multilayered squamous (more than 12 000) and, in small quantities, columnar endocervical epithelium, quite numerous leukocytes. There are no atypical cells. The cytological picture corresponds to ectopia of the columnar epithelium of the cervix. I ask you, please tell me whether such a strong treatment is possible and justified in my case? How dangerous is the situation with a deformed fetus and its consequences? And what does this even mean? Is it even possible to believe that the fetus is deformed? I don’t yet have the opportunity to go for an ultrasound to another clinic and check this conclusion..
December 21, 2009
Zheleznaya Anna Alexandrovna answers:
Good afternoon, the cyst that you were diagnosed with is most likely a corpus luteum cyst of pregnancy. folic acid, utrozhestan, magne - yes, but if there is no pain, then you don’t need a lot of antispasmodics, rectal suppositories are enough for pain or fatigue.
If there is a fetal heartbeat, then pregnancy develops. at 10 weeks you need to be examined at a medical genetics center and tested for developmental anomalies. Each doctor interprets the ultrasound picture and the human factor is important.
Maybe just do an ultrasound later and in a different place.
2013-10-01 17:09:35
Rita asks:
Hello! Thank you very much for answering people’s questions in detail, clearly, wasting your time and attention!) May God grant you all the best! I had a cleansing on August 24 - a frozen pregnancy. The fetus had no audible heartbeat and development was not at 12, but they said about 10 weeks. then, 2 weeks after the cleaning, I did an ultrasound. Body of the uterus: width 52, thickness 36, length 55. endometrium: thickness 7.6 echostructure: zminena for rakhunok (in Ukrainian) exo(-) incl. cervix: length 36, thickness 19 Right ovary: length 27, thickness 19 structure corresponds to the cycle phase, follicle max.-6 Left ovary: length 37, thickness 20 structure corresponds to the cycle phase. They told me to wait for my period. Then, after another 2 weeks, on September 26, I visited an ultrasound specialist for gastroentorology, they looked at my stomach, kidneys, liver and at the same time went down to the lower abdomen and the ultrasound specialist asked when menstruation should be, I replied that it should already be , but maybe, maybe it will be delayed, since there was a cleaning after a frozen one. She replied that she could not understand whether it was the corpus luteum or a follicle, or that it could be the remains of the fertilized egg... and on the sheet she wrote: The uterus is not enlarged, M exo 1.0 cm , the cavity is free. In the left ovary a follicle of 2.0 cm is detected. My menstruation is already delayed... I’ll go to the doctor soon. On the days when, according to the date, it turns out to be September 24, it was supposed to come + - a few days... but on these days, for 3 days, I had a twist in the lower abdomen, which seems to be about to start, but that’s all .did not start. and the feeling that there should be menstruation disappeared. Before pregnancy, menstruation was always there all the years, every day, like clockwork. There were never any glitches, everything was always fine with hormones. The pregnancy was planned and went very well too. Please tell me what is this in my size 2.0 cm, maybe?? Is it possible that this is the remnant of the fertilized egg?? but why then, after 2 weeks of ultrasound with a vaginal sensor, I didn’t have it, they didn’t see it, if there was something left there?
and how many more days should I wait for menstruation before I need to induce menstruation if it doesn’t start?
October 02, 2013
Ivanna Ivanovna Korchinskaya answers:
Let's sort it out in order. The day of cleansing is considered the first day of the menstrual cycle, it turns out that on September 24th your period should have started. With an endometrial thickness of 10 mm, menstruation can theoretically begin.
Wait another week, if your period does not start on its own, contact your gynecologist to prescribe a drug that will induce menstruation. It’s difficult to talk about a 2 cm formation virtually, without seeing the ultrasound image. I don’t think that these are the remains of the fertilized egg, nor can it be a cyst.
Most likely it is a follicle or corpus luteum. After completing your period, I advise you to undergo a control ultrasound scan.
2011-06-27 18:30:14
Julianna asks:
Help me understand the ultrasound results please 20 weeks and 3 days 1 live fetus in cephalic presentation weight 390 g Fetometry VPD 47 FAD 157 FL 35 fists + feet + fetometry corresponds to 20+3 Fetal anatomy V/h 6/20 Cr 20 BC 6 ShSh 4 Heart dimensions 20*21 4 chambers of the heart, a section of three vessels is visualized Heart rate 149 Lungs Os. liver 40*20 upper lip normal spine normal stomach 8 kidneys 20 11 13 Placenta, umbilical cord, amniotic fluid The placenta is located on the posterior wall of the uterus the thickness of the placenta is increased to 26 mm the structure of the placenta with an expanded urinary tract Degree of maturity 0 which corresponds to the period of pregnancy the amount of amniotic fluid is normal Index amniotic fluid 53 The umbilical cord has 3 vessels 14 mm
Thank you in advance
2011-06-24 14:55:24
Julianna asks:
Help me understand the ultrasound results plz) 20 weeks 3 days 1 live fetus in cephalic presentation weight 390 g Fetometry VPD 47 FAD 157 FL 35 fists + feet + fetometry corresponds to 20+3 Fetal anatomy V/h 6/20 Cr 20 BC 6 ShSh 4 Heart dimensions 20*21 4 chambers of the heart, a section of three vessels is visualized Heart rate 149 Lungs Os. liver 40*20 upper lip normal spine normal stomach 8 kidneys 20 11 13 Placenta, umbilical cord, amniotic fluid The placenta is located on the posterior wall of the uterus the thickness of the placenta is increased to 26 mm the structure of the placenta with an expanded urinary tract Degree of maturity 0 which corresponds to the period of pregnancy the amount of amniotic fluid is normal Index amniotic fluid 53 The umbilical cord has 3 vessels 14 mm
thank you in advance)
June 29, 2011
Wild Nadezhda Ivanovna answers:
Good afternoon. According to ultrasound, there is the development of placental dysfunction, possibly due to some kind of infection in the body: either the presence of a chronic or acute form. There may be other reasons, but they need to be found and, if possible, treated. An examination and ultrasound control is required.
Source: https://www.health-ua.org/tag/79225-uvelichen-zheludok-u-ploda-po-uzi.html
Intestinal pathologies
Anomalies of the duodenum include:
Atresia.
Occurs in 1 case out of 10,000. It consists of complete intestinal obstruction due to pathological fusion of the walls of the organ. In 37% of cases, it is accompanied by other anomalies - cauda equina, fusion of the cervical vertebrae, asymmetrical position of the ribs, etc.
In another 2% of cases, intestinal atresia is accompanied by esophageal atresia, anal hygroma, incomplete rotation of the stomach, etc. This is mainly typical for a fetus with chromosomal abnormalities, in particular with trisomy 21.
90% of pregnancies end in miscarriage or failure to thrive during the first 2 trimesters. The remaining 10% of pregnancies with pathology of the duodenum result in the birth of children suffering from various defects: 31% have airway obstruction (blockage by a foreign body such as a cyst, tumor), 24% have paresis of the facial nerve (impaired functionality of the facial muscles).
Only 1% of children lead a relatively normal life after undergoing a complex operation, provided there are no chromosomal abnormalities.
Intestinal membrane
. This is a film that blocks the intestinal lumen, resulting from a violation of the growth of the inner layer of the duodenum. Occurs in 1 case out of 40,000. On ultrasound it is visualized as a weakly echogenic formation. The intestinal lumen is narrowed by several millimeters, the contours of the mucous membrane are clear.
Pathology is not an indication for termination of pregnancy. Depending on the location of the membrane, it is removed after the birth of the baby using duodenotomy (opening the intestinal lumen and then removing the membrane). Malrotation.
It consists of a violation of the normal rotation and fixation of the duodenum. If the midgut has made a full rotation on the blood-feeding pedicle, this can lead to cessation of blood supply and death of the midgut.
Prenatal diagnosis can be made from 24 weeks, and polyhydramnios was observed in 61.5% of pregnancies. Ultrasound reveals an anechoic double-buble 3 consequence of dilatation of the intestine and stomach.
Although even a slight expansion at 16-22 weeks should cause alarm. Normally, the duodenum is visible on ultrasound only from 24 weeks. Additionally, in 62% of cases, malformations of the heart, genitourinary system, and other gastrointestinal organs are detected in the fetus. After karyotype testing, chromosomal abnormalities are detected in 67% of cases, of which Down syndrome ranks first. Stenosis.
It is detected in 30% of newborns, mainly in boys. This is a partial obstruction of the duodenum, localized in one place. It is mainly observed in the upper sections and is accompanied by anomalies of the pancreas. It is clearly visible on ultrasound from 24 weeks when using the Doppler method to study intestinal blood flow.
Stenosis is successfully eliminated and has more favorable prospects than atresia. Does not require termination of pregnancy. Megaduodenum
.
This is an increase in the size of the duodenum to a size that sometimes exceeds the size of the stomach. Occurs in 1 case out of 7500. It may be a consequence of an annular pancreas, when the head of the organ encircles the intestine in a ring, or atresia or stenosis of the duodenum. Diagnosed by ultrasound at 24 weeks. The upper part of the abdominal cavity is very swollen, while the lower part is sunken. Hyperechogenicity of the intestine.
The higher the density of the tissue being examined, the greater the echogenicity. On ultrasound, the echogenicity of the fetal intestine should be lower than that of bones, but higher than that of porous organs such as the liver, lungs or kidneys. When the echogenicity of the intestine is equal in density to the echogenicity of bone tissue, they speak of hyperechogenicity.
Pathology is detected no earlier than 16 weeks. It indicates a deviation in the development of the fetus. Increased echogenicity occurs with premature aging of the placenta, internal infections, discrepancy between the size of the fetus and the gestational age, endocrine disease cystic fibrosis, intestinal obstruction (stenosis).
An ultrasound scan should be performed in several different clinics to avoid specialist errors. Only when the diagnosis is finally confirmed, the woman is sent for a more detailed examination - biochemical screening, analysis for TORCH infections, cordocentesis and amniotic fluid analysis. The final diagnosis is made on the basis of a comprehensive analysis, and not just an ultrasound examination. Diverticula (cysts).
They have different names - duplication cysts, double colon, enterogenous diverticulum. It consists of budding from the intestinal walls of a formation during the embryonic period. They form not only in the intestines, but throughout the gastrointestinal tract from the larynx to the anus.
It is believed that the cause of bifurcation of the walls is a violation of the blood supply to the fetal digestive tube. Cysts on ultrasound are hypoechoic and can be either single-chamber or multi-chamber. The walls of the cysts are two-layered and have increased peristalsis, and are hyperechogenic if they contain blood.
Intestinal cysts are visualized in the 2nd trimester and are often combined with other pathologies. The accuracy of visualization of intestinal cysts in the fetus is 66.6%. This pathology is not an indication for termination of pregnancy, because in uncomplicated cases it is operated on and eliminated. Abnormalities in the shape, size, position and mobility of the intestine. By the 2nd trimester of pregnancy, it should turn around the mesenteric artery counterclockwise by 2700. If embryogenesis is disrupted, the following pathologies can be distinguished: lack of rotation, failed rotation and incomplete rotation.
On ultrasound, with anomalies of intestinal rotation in the fetus, polyhydramnios and dilation of intestinal loops without peristalsis are noted. In case of intestinal perforation, myconium peritonitis occurs - infection due to the release of intestinal contents. The pathology is detected late, only in the 3rd trimester, which requires immediate preparation of the woman for delivery.
Microgastria in the fetus? Don't give up - your child can and will be happy!
Every parent wants their child not to know what diseases are. But it happens that already in the womb the baby is given the first diagnoses of diseases. Microgastria in the fetus - not many mothers hear such a verdict while expecting a miracle, but what if this fate did not pass you by?
The most important thing is not to get upset, because most often this diagnosis is questionable and requires monitoring the dynamics of the development of internal organs. And even when the verdict is confirmed by ultrasound, absolutely healthy babies are often born, because the prevalence of this defect is only 1%. Let's figure out what microgastria is in the fetus.
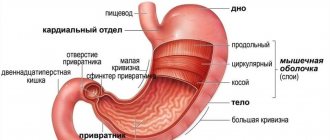
The baby's stomach lining is normal
With normal development of the baby in the womb, already at 4 weeks of embryonic development, the formation of the baby’s stomach begins. From the endodermal plate of the embryo, the future digestive tract is formed, which at this stage is represented by an ordinary intestine. Before the beginning of the fifth week, both the oral and anal openings should be formed.
In the fifth week, the fetus already has not only an expanded part of the intestine - the stomach, but also the large and small intestines.
In the sixth week, all these formations are overgrown with muscle tissue, a venous network is formed, and a serous membrane is formed, in which endocrine cells develop.
Subsequently, they mature and accumulate regulatory peptides - gastrin, motilin, secretin, neurotensin, etc. In a 14-week fetus, it is already possible not only to examine the stomach on ultrasound, but also its characteristic anatomy (fundus and body, pylorus, greater and lesser curvature).
Causes of microgastria
Microgastria, like all other malformations of a baby, most often occurs due to exposure to unfavorable factors of various origins. These include:
- stress and strong emotional experiences of the mother;
- the influence of various medications taken by a pregnant woman (teratogenic effects);
- alcohol, nicotine and tar inhaled when smoking. are also teratogens;
- bacterial infections suffered by the mother at the time of the formation and development of the organ and system;
- exposure to salts of heavy metals and other toxic substances at work, etc.
The situation with defects in the development of the unborn baby is complicated by the fact that very often at the moment the fetus’s stomach begins to form, a young woman may not even be aware of her pregnancy, and therefore may not be wary of the effects of these factors
Gastrointestinal tract with microgastria
Microgastria of the fetal stomach most often occurs in combination with other malformations of the child, this can be: absence of the gallbladder, tracheal anomalies, intestinal malrotation, vaginal atresia, imperforate anus and others.
The stomach of such children does not have differentiated parts; the shape of the organ is tubular. When x-rayed, it is most often found in the chest. At the same time, an enlarged esophagus and a shortened duodenum can be detected. Anomalies in the location of other parts of the intestine are also possible (the cecum cannot be detected, the sigmoid colon is located on the right side of the abdominal cavity).
In addition, the immature cells of the stomach glands are not able to produce hydrochloric acid, so the pH of its contents remains alkaline, even despite stimulation by histamine. Children with this pathology often have developmental delays, partly due to a lack of nutrients and vitamins (they eat little, prefer only liquid foods), and also due to combined pathologies.
Criteria for making a preliminary diagnosis
Since most often this diagnosis is first voiced by an ultrasound diagnostic specialist, there is a criterion for the normal size of the stomach in this study: its cross-section should be equal to or less than 1/16 of the cross-section of the fetal abdominal cavity. But even if a single ultrasound gives such results, dynamic observation is necessary, since often the reason for such small values of this value can be due to banal emptying of the baby’s digestive tract.
Polyhydramnios can be an indirect confirmation of the diagnosis of fetal microgastria, since very often these disorders exist in parallel. Parents who have heard such a diagnosis can be advised not only to do a repeat study, but also to contact another specialist to confirm or refute the preliminary verdict.
Possible complications
In the absence, or untimely and incorrect treatment, complications will not keep you waiting. The most common problems that may occur are:
- obstruction of the gastrointestinal tract;
- development of a hernia;
- vomiting and nausea after eating;
- persistent diarrhea and other digestive disorders.
Timely medical and, if necessary, surgical treatment can lead to a 100% recovery. The child will not only be able to fully develop and live to a ripe old age, but it is also likely to have healthy offspring.
Treatment
Depending on the severity of the pathology after the birth of the baby, doctors in the maternity hospital choose further treatment tactics. There are two main directions of treatment for microgastria in a child:
- Therapeutic treatment. Prescribed for mild gastric malformations. In this case, instead of surgical intervention, children are given tube feeding, the purpose of which is to cause widening of the gastric gap. In addition, the child is prescribed histamine-containing drugs and, if necessary, enzymes.
- Surgery. If the lumen of the stomach is negligible and there is no chance to cure the baby using conservative methods, then the issue of urgent surgery is decided. During this intervention, doctors form an analogue of the stomach from the tissues of the small intestine. Unfortunately, the process of food digestion cannot fully take place in it, but the chyme, being there for a certain amount of time, will give the body the necessary substances, minerals, and vitamins.
With the right treatment regimen, the prognosis for children with gastric microgastria is very optimistic
The diagnosis of microgastria of the fetal stomach is heard by only 1 pair of parents out of five hundred. But it is extremely important that, even after hearing such a verdict, mom and dad do not give up and continue to fight for the health and happiness of their child. After all, mother's love and father's strong shoulder under the guidance of experienced doctors will help to cope with even such a serious problem. Health to you and your baby!
Organ structure
On an ultrasound scan at 20 weeks, the fetal stomach has a round or oval shape of an anechoic formation with liquid contents. Located in the upper quadrant of the abdomen. The size depends on the amount of amniotic fluid swallowed.
Normally, the organ should peristalt.
In the absence of visualization of the stomach during a 30-minute observation, they speak of poor filling of the organ, its absence, dystopia due to a congenital hernia, or lack of connection with the esophagus.
Stomach dimensions
The table of measurements by week allows us to judge the normality of development by measuring the diameter of the fetal abdomen:
| Duration, weeks | Circumference, mm |
| 16 | 88—116 |
| 17 | 93—131 |
| 18 | 104—144 |
| 19 | 114—154 |
| 20 | 124—164 |
Diseases and abnormalities
One possible type of pathology may be esophageal atresia.
It is from the 16th to 20th week that pathology can be observed that affects the gastrointestinal tract. As soon as there is a suspicion of any anomaly during screening, a dynamic ultrasound is prescribed at 22 weeks of pregnancy. Among the vices there are:
- Artresia or absence of natural passages. Often this is non-visualization of the pyloric or antral zone. Often combined with polyhydramnios, anomalies of the larynx and esophagus, and pulmonary dysplasia.
- Artesia of the esophagus. Due to the absence of a passage opening, the digestive organ is not filled with amniotic fluid, and therefore is not visualized. The cause may also be central nervous system defects, cleft lip, or neuromuscular pathologies.
- Microgastria, when the stomach is reduced, has an irregular shape (cylindrical) and does not correspond to the period of fetal development.
- Macrogastria, when the organ is too large. Develops against the background of intestinal obstruction and obstruction. Additional differential signs when the stomach is enlarged are: thickening of the walls, absence of the lesser curvature, narrowing of the funnel-shaped vestibule.
- Gastromegaly, when the organ is too dilated. It can also be a variation of macrogastria (when the organ is large).
- Slit-like stomach, as a consequence of underdevelopment during onotogenesis. There are fewer norms.
- Location anomalies. When displacement or doubling of an organ occurs.
Reasons for deviations from the norm
The pathology may be due to a hereditary factor.
Incorrect size of the stomach in the fetus, its absence is provoked by the following factors:
- maternal infectious diseases;
- deficiency of nutrients;
- use of contraindicated drugs during pregnancy;
- bad ecology;
- heredity;
- pathologies of the placenta.
Diagnostics
It is possible to determine abnormalities in the development of the stomach in the fetus only by ultrasound. The image on the device allows you to determine the volume and size of the organ in dynamics and in real time from the 20th week.
It is also possible to determine the presence of “pseudo-content,” which is characterized by the ingestion by the fetus of blood that appears in the amniotic fluid after amniocentesis or during placental abruption.
Ultrasound allows you to differentiate this condition from tumors in the stomach.
Treatment of abnormalities
Microgastria of the fetal stomach, like macrogastria, a slit-shaped organ, requires careful monitoring during pregnancy and after birth. Often, a small stomach is treated conservatively: with diet and medications.
But if the pathology is accompanied by GER (reflux esophagitis) in a newborn child, antireflux surgery is needed. Pyloric atresia is treated surgically. In this case, the success of the operation reaches 90%.
Sometimes a decision is made to create an artificial cavity from parts of the small intestine, which will allow food to be retained and absorbed to a greater extent.
If pyloric stenosis has been diagnosed (improper structure of the pyloric area and an enlarged stomach in the fetus), to ensure normal passage of food into the duodenum, surgery will also be required immediately after the birth of the child. In case of severe defects in the development of several organs and systems, the woman may be offered the option of terminating the pregnancy. Otherwise, the baby is unlikely to survive after birth.
March 29, 2021 At 19-20 weeks, a second screening ultrasound of the fetus is performed. By this time, the child is fully formed, all his organs are distinguishable and it is possible to identify their anomalies. One of the organs that undergoes a thorough examination is the stomach. What size of the fetal stomach on ultrasound is normal, and should you panic if it deviates from these values?
Sonography allows you to examine and evaluate the condition of internal organs. Organs such as the heart, spleen, lungs, kidneys, bladder, and, of course, the stomach are subject to close study. Read more about the second screening.
Why is it important to assess the condition of the baby’s internal organs? The fact is that some deviations in their development are markers of chromosomal abnormalities. Such pregnant women are then recommended to undergo genetic counseling.
The timing of the screening study (16-22 weeks) was chosen so that if severe intrauterine developmental anomalies incompatible with life are detected, the pregnancy can be terminated.
Norms for the size of the fetal stomach on ultrasound and possible deviations
The fetal stomach at 16-20 weeks can have variable sizes. They are defined in millimeters. The normal sizes of the fetal stomach by week are presented in the table.
| Gestational age | Abdominal circumference |
| 16 weeks | 88-116 |
| 17 weeks | 93-131 |
| 18 weeks | 104-144 |
| 19 weeks | 114-154 |
| 20 weeks | 124-164 |
The study may reveal the following deviations:
- large or small stomach in the fetus on ultrasound;
- absence of an organ;
- presence of pseudo-content;
- slit-like stomach;
- gastric atresia in the fetus.
Causes of abnormalities in the fetal stomach
The stomach on ultrasound is defined as a round or oval anechoic formation located in the upper left parts of the abdominal cavity. Changes on its part may be signs of gastrointestinal pathology or indirect signs of other unfavorable conditions.
If the fetus's stomach is not visible on ultrasound
, then suggest esophageal atresia. In this case, the organ is there, but it is not filled with amniotic fluid.
The absence of echoshadow may indicate oligohydramnios, and this indirectly indicates kidney pathology, chronic infections of the mother, pathology of the placenta, and gestosis.
Sometimes the fetal stomach is not visualized if it is displaced from its usual place. This condition occurs with a diaphragmatic hernia.
Fluid in the stomach
sometimes absent due to defects of the central nervous system, cleft lip, neuromuscular diseases.
"Pseudo-contents" of the stomach
– these are various hyperechoic inclusions. They are formed when clumps of cells are ingested.
Sometimes an intrauterine tumor manifests itself this way, but it is rarely diagnosed in isolation; it is accompanied by other anomalies. Swallowed blood also gives the picture of a full stomach.
In this case, you need to look for the cause of the bleeding and carefully examine the placenta for abruption. Blood may appear after amniocentesis is performed.
If no pathology of the placenta or other defects is detected, then the isolated presence of “pseudo-content” is taken as a variant of the norm.
The cause of an enlarged stomach in the fetus
There may be intestinal obstruction and obstruction. But it should be remembered that the stomach can expand to significant sizes and this is the norm. Therefore, if the size of an organ deviates from the norm, you need to look for additional symptoms:
- polyhydramnios;
- thickening of the walls of the organ;
- the vestibule is narrowed and funnel-shaped;
- no slight curvature.
Microgastria of the fetal stomach
does not occur as a separate congenital disease. It is usually part of the pathology of the entire gastrointestinal tract. It can be combined with:
- violation of rotation of abdominal organs;
- absence of a gallbladder;
- abnormal position of the liver.
With microgastria, the stomach looks small, significantly smaller in size than normal, and may be cylindrical in shape.
Slit-like stomach in the fetus
means its underdevelopment during onotogenesis.
Microgastria and slit-like stomach are subject to observation after detection. After the baby is born, plastic surgery is performed to create a stomach from part of the small intestine. It will not be able to perform its main functions, but will keep food from directly entering the intestines. This will increase the digestion time, and the child will be able to absorb more nutrients.
Gastric atresia
- a rare anomaly. This is the presence of a membrane in the pyloric or antrum. Sometimes the fusion is incomplete, there is a small hole.
Like most developmental defects, there is a combination of atresia with anomalies of the larynx, esophagus, pulmonary dysplasia, ascites, and hydrothorax. Sometimes it is a sign of autosomal recessive hereditary diseases, combined with epidermolysis bullosa.
Isolated pyloric atresia can be treated surgically, with a survival rate reaching 90%.
The fetus may not have a stomach
. This condition is called agastria or agenesis. In the first case, the pathology is the absence of the upper part of the abdominal wall and the organs of half of the abdominal cavity. Agenesis is the absence of an organ. An extremely rare pathology, combined with multiple defects of other organs. These developmental anomalies are incompatible with life.
What to do if a fetal stomach pathology is detected by ultrasound?
Any pathologies identified during screening require repeated ultrasound diagnostics over time. It is carried out at 22 weeks. If the anomalies detected in the previous study were transient in nature, then they will disappear with repeated diagnostics. Persistent changes speak in favor of serious congenital diseases.
In case of severe concomitant malformations, the woman is offered termination of pregnancy for medical reasons. The birth of such a child is impossible; it will end in death in the first few days.
Yulia Shevchenko, obstetrician-gynecologist, especially for Mirmam.pro
Important!
Liver pathologies in the fetus
The liver is visualized by ultrasound examination already at the 1st screening. At 11-14 weeks, a hypoechoic formation in the form of a month can be seen in the upper part of the abdominal cavity. By week 25, echogenicity increases and becomes the same as that of the intestine, and before birth it exceeds the density of the intestine.
Assessing the state of liver blood flow is very important. The fetal umbilical cord vein enters the liver, and in the 2nd trimester the portal vein is visualized. Its diameter is normally 2-3 mm, and by childbirth it increases to 10-11 mm. Bile ducts should not normally be visualized in the fetus. One of the most common pathologies of the fetus is hepatomegaly of the liver - an increase in the size of the organ. To detect anomalies, a 3D sensor is used that can visualize the slice in longitudinal, transverse and vertical sections. You can also see an increase in the size of the liver on a regular ultrasound machine through a protruding tummy, the coverage of which significantly exceeds the norm.
At the same time, various hyperechoic inclusions are visible on the screen. As a rule, the anomaly is complemented by an enlarged spleen.
Among the reasons leading to an increase in the size of the digestive organs are hidden infections (toxoplasmosis, syphilis, chickenpox), as well as chromosomal mutations (Down, Zellweger, Beckwet-Wiedemann syndromes).
- With Zellweger syndrome, abnormalities of the limbs, distortion of the chest, and kidney cysts are visible. Analysis of amniotic fluid reveals a deficiency of dihydroxy-acetone-phosphate acyl-transferase.
- Chickenpox, herpes, and cytomegalovirus cause calcification of hepatic vein thrombi, which is reflected on the ultrasound monitor screen as hyperechoic round calcifications. They are also formed during meconium peritonitis - poisoning with the contents of the fetal intestines, which enters as a result of damage to the walls.
In 87.5% of cases, the cause of liver enlargement and the formation of calcifications is intrauterine infections. Also, most pregnant women are diagnosed with hyperechoic intestines, changes in the structure of the placenta, and a large spleen. Pathology in the 3rd trimester occurs in case of Rh conflict between mother and child. Metabolic disorders are also possible. Liver enlargement occurs with galactosemia (a genetic disorder of carbohydrate metabolism, due to which galactose is not converted into glucose), trypsinemia (lack of production of the digestive hormone trypsin), methylmalonic acidemia (lack of conversion of D-methylmalonic acid into succinic acid), and disorders of urea excretion. Single large hyperechoic inclusions are much better than multiple scattered formations in combination with other pathologies. In almost 100% of cases, large hyperechoic inclusions are eliminated before the baby is born or in the first year of life. In some cases, abdominal organ defects are diagnosed incorrectly. This happens if the baby’s abdominal cavity is compressed by the walls of the uterus, myometrial pathologies or other factors.
The monitor screen shows a pseudoomphalocele - an erroneous visualization of the exit of the abdominal organs beyond the abdominal wall. Sometimes ultrasound “does not see” significant defects. Thus, a hernia in shape and echostructure resembles intestinal loops; in this regard, Doppler ultrasound is of great help, allowing one to see the blood flow.
Our clinic has an excellent 4D device, equipped with all modern capabilities that eliminate diagnostic errors.
Microgastria of the fetal stomach - causes, pathology
Microgastria of the fetal stomach is a very rare pathology of the intrauterine development of a child, which is characterized by a decrease in the size of the stomach and a change in its shape. This disease is diagnosed in one newborn out of a hundred, it is dangerous for serious complications in the future, requires long-term and complex treatment, which in most cases has a positive prognosis.
Microgastria is a rather rare pathology of child development; the factors that cause it are still unknown. It is believed that with this pathology the rotation of the stomach stops and it remains in an upright position.
This pathology very rarely comes alone; it is usually combined with anomalies in the development of the trachea, esophagus, intestines, absence of the gallbladder and abnormal location of the liver, and pathologies of the rectum.
Microgastria is usually accompanied by several anomalies from this list.
Clinical picture
What symptoms are accompanied by gastric microgastria? This pathology leads to a decrease in the size of the organ, which does not correspond to the development of the child, as well as to a change in the shape of the stomach.
With microgastria, the sections of the stomach are usually not differentiated, the esophagus is dilated, and a violation of the internal environment of the organ is often observed (it remains alkaline).
The duodenum may be shorter than it should be and may not have its characteristic curves.
Changes in the size of the stomach rarely occur separately; usually this disease is accompanied by impaired intestinal rotation, abnormal location of the liver, and absence of the gallbladder. There may be other disorders, but these are the most common.
https://www.youtube.com/watch?v=ZvKls_-wl48u0026list=PL-Hg0RRDgfBpiYXOpFia7_twYH6mYTGIL
This disease can be diagnosed during fetal development, and treatment begins after birth.
The main symptoms that accompany microgastria are:
- nausea and vomiting;
- frequent diarrhea, development of obstruction;
- hernias;
- hypochromic normocytic anemia;
- aspiration pneumonia;
- developmental disorder (delay).
Causes
The causes of the disease are still poorly understood. No specialist can give an exact answer as to why this disease occurred in a child. But probably the main reason for the development of microgastria is the lifestyle of the expectant mother.
Doctors believe that microgastria is often the result of mechanical damage: even minor blows that go unnoticed by the expectant mother can lead to the development of such pathologies. It is believed that microgastria develops when it is impossible (for any reason) to swallow amniotic fluid.
Stomach
At 16-20 weeks, the fetal stomach is visualized as an anechoic formation of a round or oval shape in the upper abdominal cavity. If the stomach is not filled with amniotic fluid, then we can talk about esophageal atresia (complete absence of lumen).
With a diaphragmatic hernia, the stomach is displaced and also cannot be detected on an ultrasound. Also, amniotic fluid is absent when the central nervous system is damaged in the fetus. If the fetus swallows blood along with liquid, hyperechoic inclusions are visualized in the stomach. They are also seen in stomach tumors, but they are usually accompanied by other malformations. The size of the organ increases with intestinal obstruction, polyhydramnios, thickening of the walls, and absence of the lesser curvature. A decrease in the size of the stomach is typical of microgastria, which occurs due to the absence of a bladder or abnormal position of the liver. In 52% of cases, the fetus dies before the 24th week of pregnancy, and the child is born non-viable. A slit-like stomach is characteristic of underdevelopment in the early stages of pregnancy. This pathology is corrected after the baby is born: a stomach is constructed for the child from part of the small intestine. The operation is extremely complicated, but the anomaly is not an indication for an abortion. Gastric atresia is characterized by the absence of echoshadow and involves the formation of a film with or without an opening located across the walls of the stomach. If this is an isolated pathology, then in 90% of cases it is eliminated surgically. But usually gastric atresia is combined with fusion of the esophagus, ascites (excessive accumulation of fluid), and underdevelopment of the lungs. Gastric agenesis involves the complete absence of the organ. This is typical for severe chromosomal abnormalities that cause fetal death during the prenatal period. Ultrasound at week 22 is of great importance in diagnosis. some abnormalities disappear on their own, while others require immediate intervention.
If you find an error, please select a piece of text and press Ctrl+Enter
Norms for the size of the fetal stomach on ultrasound and possible deviations
The fetal stomach at 16-20 weeks can have variable sizes. They are defined in millimeters. The normal sizes of the fetal stomach by week are presented in the table.
| Gestational age | Abdominal circumference |
| 16 weeks | 88-116 |
| 17 weeks | 93-131 |
| 18 weeks | 104-144 |
| 19 weeks | 114-154 |
| 20 weeks | 124-164 |
The study may reveal the following deviations:
- large or small stomach in the fetus on ultrasound;
- absence of an organ;
- presence of pseudo-content;
- slit-like stomach;
- gastric atresia in the fetus.
Main settings
On an ultrasound scan at 20 weeks, the fetal stomach has a round or oval shape of an anechoic formation with liquid contents. Located in the upper quadrant of the abdomen. The size depends on the amount of amniotic fluid swallowed. Normally, the organ should peristalt. In the absence of visualization of the stomach during a 30-minute observation, they speak of poor filling of the organ, its absence, dystopia due to a congenital hernia, or lack of connection with the esophagus.
The table of measurements by week allows us to judge the normality of development by measuring the diameter of the fetal abdomen:
| Duration, weeks | Circumference, mm |
| 16 | 88—116 |
| 17 | 93—131 |
| 18 | 104—144 |
| 19 | 114—154 |
| 20 | 124—164 |
Return to contents