Esophageal varicose veins: classification
The pathology of the varicose system of the esophagus is formed due to increased pressure in the structure of the portal or vena cava. When pressure increases, the outflow of blood is disrupted or stagnation occurs in the esophageal veins, which leads to the formation of varicose veins.
The effectiveness of the prescribed therapy depends on the correct diagnosis. In medical practice, esophageal varicose veins are classified according to severity. There are several types of systematization: NIEC (Italy), OMED, JRSPH (Japan), but they are all based on the same characteristics and the differences in classification are minor.
- Stage I. Pathology is detected only during endoscopic examination. Single dilations of the veins in the distal part of the esophagus are observed, no more than 5 mm.
- Stage II. It is characterized by tortuosity of the veins with their localization in the lower third of the food tube. The dimensions of the organ, as well as the thickness of its mucosa, are within normal limits.
- Stage III. Pathological changes in the veins are pronounced. The vessels swell and expand into the cavity of the organ, which leads to its narrowing. On endoscopic examination, red spots are observed.
- Stage IV. Many varicose nodes form in clusters. This leads to a strong narrowing of the lumen of the esophagus, up to its closure. Obstruction of the esophagus and the development of bleeding are observed. Treatment of pathology at this stage is carried out, among other things, by ligation of the esophageal veins.
Ligation of esophageal veins: description of the procedure, procedure, consequences, rehabilitation
Esophageal varicose veins are a disease of the esophageal veins, characterized by their tortuosity and expansion due to the development of phleboectasis.
In most cases, the pathology is asymptomatic and manifests itself only with complications in the form of bleeding. Esophageal vein ligation is a procedure designed to prevent bleeding.
The operation eliminates the complication of the pathology; an integrated approach is required to treat varicose veins.
Esophageal varicose veins: classification
The pathology of the varicose system of the esophagus is formed due to increased pressure in the structure of the portal or vena cava. When pressure increases, the outflow of blood is disrupted or stagnation occurs in the esophageal veins, which leads to the formation of varicose veins.
The effectiveness of the prescribed therapy depends on the correct diagnosis. In medical practice, esophageal varicose veins are classified according to severity. There are several types of systematization: NIEC (Italy), OMED, JRSPH (Japan), but they are all based on the same characteristics and the differences in classification are minor.
- Stage I. Pathology is detected only during endoscopic examination. Single dilations of the veins in the distal part of the esophagus are observed, no more than 5 mm.
- Stage II. It is characterized by tortuosity of the veins with their localization in the lower third of the food tube. The dimensions of the organ, as well as the thickness of its mucosa, are within normal limits.
- Stage III. Pathological changes in the veins are pronounced. The vessels swell and expand into the cavity of the organ, which leads to its narrowing. On endoscopic examination, red spots are observed.
- Stage IV. Many varicose nodes form in clusters. This leads to a strong narrowing of the lumen of the esophagus, up to its closure. Obstruction of the esophagus and the development of bleeding are observed. Treatment of pathology at this stage is carried out, among other things, by ligation of the esophageal veins.
Factors influencing the development of pathology
In rare cases, the disease is congenital. But in most cases it is acquired and is formed for a number of reasons. Impaired blood flow and increased pressure, which leads to esophageal varices, are associated with the following factors:
- Infectious lesions of the liver with changes in its parenchyma.
- Cirrhosis of the liver.
- Benign and malignant neoplasia in the liver.
- Pathological change (expansion) of the hepatic artery.
- Portal vein obstruction.
- A vascular disease characterized by the formation of blood clots inside blood vessels.
- Hypertonic disease.
- Damage to the thyroid gland.
According to statistics, the pathology most often occurs in men over 50 years of age.
Treatment methods
Depending on the stage of the disease, therapy is prescribed. The treatment is complex and under the mandatory supervision of doctors either in the gastroenterology department or in surgery. The main task is to prevent bleeding.
Drug treatment
Even if during the diagnosis it becomes clear that surgical intervention is not possible, the patient cannot do without medications.
- Hemostatic drugs: “Troxerutin”, “Curantil”, “Ascorutin”.
- Drugs that reduce acidity: “Rennie”, “Almagel”, “Relzer”.
- Vitamin K
- Calcium preparations.
- Fresh frozen plasma.
Surgical methods of therapy
The use of such methods is considered much more effective compared to conservative treatment. Surgeons use the following techniques:
- Sclerosis of the esophageal veins is an endoscopic technique in which a sclerosant solution is injected into the vein wall, which subsequently causes obliteration of the vessel.
- The transjugular method of shunting is the application of a portacaval shunt in the middle of the hepatic and portal veins.
- Banding is the installation of small elastic bands over dilated veins.
- Devascularization is the removal of bleeding vessels.
- Endoscopic ligation of esophageal veins - applying clips to the affected bleeding vessels. Clipping avoids recurrent bleeding.
This operation is prescribed in the last stages of vascular pathology of the gastrointestinal tract. Ligation of the esophageal veins is an endoscopic surgical operation in which the dilated veins of the esophagus are ligated using special elastic ligature rings (hence the name). It can be performed as planned or in the event of an emergency bleeding.
As a result of the procedure, the lumen of the veins narrows, they are narcotized, and blood stops flowing to the affected areas. During the operation, mechanical damage to the walls of the esophagus sometimes occurs. But the injuries are minor, and this is a fairly rare occurrence.
Indications and contraindications for the procedure
The indication for ligation of esophageal varices is the prevention of primary and recurrent bleeding. Surgery may also be prescribed for the following conditions:
- Stages III and IV of esophageal varicose veins.
- Progressive cirrhosis of the liver.
- Severe stages of hypertension.
Contraindications to surgery are:
- Acute stages of cardiovascular diseases.
- Serious cerebrovascular accidents
- The period of exacerbation of any chronic diseases.
- Disruption of the hemostasis system.
Preparing for surgery
Preparatory activities include various general laboratory tests and instrumental diagnostics.
Laboratory research:
- Clinical blood test.
- Analysis of urine.
- Biochemistry of urine.
- Coagulogram.
- HIV, antibodies to hepatitis.
Instrumental diagnostics:
- Transabdominal ultrasound examination of the abdominal organs.
- MRI of the liver.
- X-ray of the esophagus.
- Esophagogastroduodenoscopy. Using this procedure, changes in the mucous membrane are visualized, the extent to which the lumen of the esophagus is narrowed, and damage of various origins is assessed.
If it is necessary to carry out ligation of the esophageal veins in case of liver cirrhosis, then the opinion of an infectious disease specialist and a hepatologist will be required. They, in turn, may order additional tests.
If the pathology arose as a result of the hemostasis system, it is necessary to obtain a phlebologist’s opinion.
Technology for ligation of esophageal varicose veins
The operation can be performed under either local or general anesthesia. 12 hours before the procedure you should completely avoid eating. Immediately before the intervention, the patient is given an enema and given psycholeptics.
The patient lies on his left side and inserts a mouthpiece into his mouth. The endoscopist inserts an endoscope through the pharyngeal ring. A special attachment on the esophagoscope allows you to visualize even the slightest changes in the mucosa.
The device is brought close to the affected vein and the vacuum aspirator is turned on. A section of the vein is sucked into the nozzle, where a ligature (nylon or latex ring) is placed over it. At one time, throw on from 3 to 10 rings. The ring thoroughly tightens the area of the vessel, which leads to its desolation and “gluing”. The operation lasts no more than an hour.
After operation
The patient is taken to the ward, even if local anesthesia was used. You can't get up for several hours. Within a week after ligation of the esophageal veins, certain areas die and become covered with fibrin. Necrotic vascular tissue falls off and is eliminated from the body naturally. Ulcers appear at the site of detachment, which scar after 3 weeks.
The patient is discharged no earlier than a week after the procedure. This is due to the fact that it is during this period that various complications may arise. Possible negative consequences:
- Severe pain in the abdominal area.
- Repeated bleeding.
- Development of the inflammatory process at the site of the latex ring.
- Allergic reaction to ligature material.
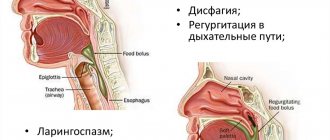
- Swallowing disorder. This is a fairly rare occurrence and is often associated with a psychological factor.
Rehabilitation period
After ligation of the dilated veins of the esophagus, upon arrival home, the patient must strictly follow all medical instructions. Otherwise, serious complications may develop.
The main condition for a speedy recovery is diet. Starting from the second day, the patient is transferred to table No. 1. Food should be boiled and ground through a blender. The duration of the diet is about a month. Subsequently, the patient is transferred to table No. 5.
It is not recommended to engage in sports or serious physical activity for 3 years. If your previous job does not allow you to do this, you will have to change it.
Surgery does not involve the removal of an important organ, so it does not result in disability.
Doctors advise visiting special sanatoriums with mineral waters. In addition, they have developed a special daily routine with procedures that promote rapid recovery.
You need to know that esophageal varicose veins are incurable. After surgery, all measures must be taken to prevent re-bleeding.
Prevention
In order to avoid ligation of the esophageal veins in cirrhosis, it is necessary to take all measures to prevent and timely treat this disease. You should be regularly examined and see a hepatologist. Internal hemorrhages are very dangerous and often lead to death. To avoid disastrous consequences, you should be examined by a gastroenterologist.
People prone to varicose veins should adhere to a special diet. Fried, spicy foods should be excluded, food should be chewed properly. Dishes should not be too cold or hot.
You should completely stop drinking alcohol. You should not lift weights, but it is also extremely undesirable to lead a passive lifestyle.
Surgery is an extreme, albeit effective, method of therapy. In order not to resort to its use, at the slightest abnormal manifestations, you must visit a doctor.
Source: https://FB.ru/article/438672/ligirovanie-ven-pischevoda-opisanie-protseduryi-poryadok-provedeniya-posledstviya-reabilitatsiya
Factors influencing the development of pathology
In rare cases, the disease is congenital. But in most cases it is acquired and is formed for a number of reasons. Impaired blood flow and increased pressure, which leads to esophageal varices, are associated with the following factors:
- Infectious lesions of the liver with changes in its parenchyma.
- Cirrhosis of the liver.
- Benign and malignant neoplasia in the liver.
- Pathological change (expansion) of the hepatic artery.
- Portal vein obstruction.
- A vascular disease characterized by the formation of blood clots inside blood vessels.
- Hypertonic disease.
- Damage to the thyroid gland.
According to statistics, the pathology most often occurs in men over 50 years of age.
Causes of pathology
Varicose veins of the esophagus are formed as a result of disruption of blood flow to the liver through the portal vein, usually as a result of scar changes in the tissue of the organ. When the outflow of blood through the portal vein is disrupted and the pressure in it increases, the blood begins to “look” for workarounds. One of them - portacaval anastomosis (communication between the cava and portal vein) - is located in the veins of the esophagus. The pressure also increases in them and they expand. Under certain conditions they may begin to bleed.
The most common causes of increased pressure in the portal vein, which lead to esophageal varices:
- Cirrhosis is a condition in which normal liver tissue is replaced by fibrous connective tissue. It develops as a result of viral hepatitis, alcoholic liver disease, fatty hepatosis, impaired bile outflow (primary biliary cirrhosis) and other pathological processes.
- Chronic hepatitis.
- Thrombosis is a blood clot in the portal vein or splenic vein.
- Parasitic infections such as schistosomiasis.
- Compression of the portal vein by pathological formations from the outside.
- Liver cancer is hepatocellular carcinoma.
- Pathologies of the tricuspid heart valve.
According to prospective studies, 90% of patients with liver cirrhosis sooner or later develop dilatation of the esophageal veins, and 30% develop bleeding. Once a patient is diagnosed with cirrhosis, the risk of developing esophageal varices is 5% annually. The risk of bleeding is 10–15% per year. At the time of diagnosis of cirrhosis, dilatation of the venous vessels of the esophagus is detected in approximately 30% of patients.
The risk of bleeding depends on several factors:
- Portal vein pressure. The higher it is, the more likely bleeding will develop.
- The degree of dilation of the veins of the esophagus.
- Presence of “Red Markers”: If red streaks or spots are found in the area of esophageal varices during endoscopic examination, the risk of bleeding is higher.
- Degree of liver dysfunction. It is assessed using a special Child-Pugh scale. The more severe the liver failure, the higher the likelihood of bleeding.
- Alcohol consumption. If a person already has esophageal varices but continues to drink alcohol, they are more likely to develop bleeding.
- If the patient has already had bleeding, then there is a risk of it happening again in the future.
Bleeding from varicose veins of the esophagus threatens serious blood loss, the development of shock and death of the patient. Ligation helps prevent this dangerous complication.
The degree of esophageal varices is assessed during an endoscopic examination. Classification of the World Gastroenterological Organization:
- Grade 1 (small varicose size): less than 0.5 cm, small dilated veins that are visible above the surface of the mucous membrane.
- Grade 2 (medium-sized node): tortuous dilated veins occupy less than a third of the lumen of the esophagus.
- Grade 3 (large varicose nodes): more than 0.5 cm, covering more than a third of the lumen of the organ.
Our doctors will help you
Leave your phone number
Surgical methods of therapy
The use of such methods is considered much more effective compared to conservative treatment. Surgeons use the following techniques:
- Sclerosis of the esophageal veins is an endoscopic technique in which a sclerosant solution is injected into the vein wall, which subsequently causes obliteration of the vessel.
- The transjugular method of shunting is the application of a portacaval shunt in the middle of the hepatic and portal veins.
- Banding is the installation of small elastic bands over dilated veins.
- Devascularization is the removal of bleeding vessels.
- Endoscopic ligation of esophageal veins - applying clips to the affected bleeding vessels. Clipping avoids recurrent bleeding.
Etiology and pathogenesis of the disease
The classification for varicose veins of the esophagus is as follows:
- Grade 1 esophageal pathology is characterized by an increase in the diameter of the veins (three mm);
- in the second degree, the size of the arteries is 3–5 mm in diameter;
- Grade 3 esophageal pathology is determined by the size of the veins (diameter more than 5 mm);
The arterial expansion of the esophagus is due to its anatomical connection with the portal vein system, as well as the spleen and other organs of the gastrointestinal tract. Phlebectasia develops against the background of diseases leading to blockage of venous networks and the formation of collaterals and aneurysms.
There are congenital and acquired varicose veins of the digestive tube. The first disease is less common than the second disease. With acquired varicose veins in the esophageal tube, the saccular arterial dilatations are significantly increased.
What is esophageal vein ligation?
This operation is prescribed in the last stages of vascular pathology of the gastrointestinal tract. Ligation of the esophageal veins is an endoscopic surgical operation in which the dilated veins of the esophagus are ligated using special elastic ligature rings (hence the name). It can be performed as planned or in the event of an emergency bleeding.
As a result of the procedure, the lumen of the veins narrows, they are narcotized, and blood stops flowing to the affected areas. During the operation, mechanical damage to the walls of the esophagus sometimes occurs. But the injuries are minor, and this is a fairly rare occurrence.
The main advantages of the vein embolization method used in the center of Professor Kapranov
Endovascular embolization in our center is a low-traumatic procedure. It is fundamentally different from standard surgical interventions in the absence of large incisions in the vein and tissue. In addition, embolization does not require the patient to be put under general anesthesia. This reduces numerous risks and makes intervention possible in the presence of general contraindications to standard surgery.
The advantages of carrying out the intervention at the center of Professor Kapranov also include:
- Experience of professionals. All doctors performed a lot of interventions to restore the functionality of the esophagus. They are ready to help you too.
- Comfortable conditions of stay in any clinic. Embolization of the esophageal vessels will not cause pain or severe discomfort.
- Reducing the likelihood of relapse. The technique used to block the vessel allows you to quickly and reliably stop the blood flow of the vein (vessel) of the esophagus.
- No discomfort when restoring the functionality of the esophagus. During vein embolization, the patient does not experience pain. All unpleasant sensations are eliminated with the help of special medications.
- Short recovery period after intervention for varicose veins of the esophagus. For minor vascular interventions, the patient may be discharged on the day of the procedure. In this case, special care, complex treatment, and regular dressings are not required.
- Minimal number of contraindications and complications. The success of an operation for embolization of esophageal vessels largely depends on the professionalism of the doctor. That is why it is important to choose a surgeon wisely.
- Opportunities for organ preservation. Esophageal embolization, for example, avoids a number of serious problems.
Indications and contraindications for the procedure
The indication for ligation of esophageal varices is the prevention of primary and recurrent bleeding. Surgery may also be prescribed for the following conditions:
- Stages III and IV of esophageal varicose veins.
- Progressive cirrhosis of the liver.
- Severe stages of hypertension.
Contraindications to surgery are:
- Acute stages of cardiovascular diseases.
- Serious cerebrovascular accidents
- The period of exacerbation of any chronic diseases.
- Disruption of the hemostasis system.
Symptoms of the disease
At the initial stage of pathological changes, pronounced symptoms of varicose veins of the esophagus may not be observed. Heartburn may appear, but such a symptom is not always given due importance. In addition, heartburn can signal completely different diseases.
Indirect signs of bleeding from esophageal varices are black or bloody stools, which indicates internal bleeding. For the same reason, the patient may feel weak and causelessly tired.
Symptoms of varicose veins of the esophagus may not be permanent, lulling vigilance. However, the disease can have serious consequences; at the slightest suspicion of esophageal varicose veins, you should consult a doctor.
Important: a very serious sign of the disease is the clear appearance of veins on the chest, which occurs due to strong pressure in the veins.
Preparing for surgery
Preparatory activities include various general laboratory tests and instrumental diagnostics.
Laboratory research:
- Clinical blood test.
- Analysis of urine.
- Biochemistry of urine.
- Coagulogram.
- HIV, antibodies to hepatitis.
Instrumental diagnostics:
- Transabdominal ultrasound examination of the abdominal organs.
- MRI of the liver.
- X-ray of the esophagus.
- Esophagogastroduodenoscopy. Using this procedure, changes in the mucous membrane are visualized, the extent to which the lumen of the esophagus is narrowed, and damage of various origins is assessed.
If it is necessary to carry out ligation of the esophageal veins in case of liver cirrhosis, then the opinion of an infectious disease specialist and a hepatologist will be required. They, in turn, may order additional tests.
If the pathology arose as a result of the hemostasis system, it is necessary to obtain a phlebologist’s opinion.
Consequences of the disease
It is almost impossible to completely get rid of such a disease. Varicose veins of the esophagus are a very dangerous disease and the mortality rate is high. If the patient experiences an exacerbation, symptoms may return with increased severity in a short time. After eliminating foci of inflammation, you must carefully follow the recommendations. There is a high probability of death of the patient in the period from 1 to 3 years after making such a diagnosis due to the development of cirrhosis of the liver. To prolong your life, you need to carefully monitor the condition of your body and consult a doctor at the slightest deviation.
Technology for ligation of esophageal varicose veins
The operation can be performed under either local or general anesthesia. 12 hours before the procedure you should completely avoid eating. Immediately before the intervention, the patient is given an enema and given psycholeptics.
The patient lies on his left side and inserts a mouthpiece into his mouth. The endoscopist inserts an endoscope through the pharyngeal ring. A special attachment on the esophagoscope allows you to visualize even the slightest changes in the mucosa.
The device is brought close to the affected vein and the vacuum aspirator is turned on. A section of the vein is sucked into the nozzle, where a ligature (nylon or latex ring) is placed over it. At one time, throw on from 3 to 10 rings. The ring thoroughly tightens the area of the vessel, which leads to its desolation and “gluing”. The operation lasts no more than an hour.
Preparation and performance of the operation
Before prescribing alloying, the specialist must necessarily indicate the need to carry out certain procedures. In particular, we are talking about an initial examination, a blood test and correct checking of the patient for the presence of any contraindications. It is also important to consider that before a procedure in the area of the esophageal veins, it is unacceptable to eat food for 12 hours; in some cases, the presented period of time is even longer.
In addition, it is very important to stop using anti-inflammatory drugs and blood thinners. Before the operation itself, the patient is given a dose of local anesthesia, and sedative and sedative components may also be administered. Speaking about the operation itself in the area of the esophageal veins, it should be noted that it always goes through the following sequential stages:
- the patient must be placed on his left side and in order for the oral cavity to be open, a dilator is placed in it;
- heart rate and breathing indicators should be under constant monitoring by assistants;
- To drain saliva, a special tube is inserted into the mouth. In addition, if there is such a need, oxygen is administered through the nose.
Intervention in the area of the esophageal veins also involves inserting an endoscope into the problem organ through the oral area.
It is equipped with a microscopic camera and a lamp to simultaneously film and illuminate internal organs.
Speaking about the expansion of the organ, it should be noted that it occurs due to the supply of air. It is also important to consider that the loops are always placed around the problem area. As a result of such manipulations, the pathological area of tissue will be sucked into the tube.
What is balloon dilatation and how is it performed?
The presented procedure, performed in the area of the esophageal veins, can last no more than 60 minutes. This intervention is one of the least traumatic in its field, and therefore is the most in demand today. About how rehabilitation is carried out and what other, additional information about alloying is, below.
After operation
The patient is taken to the ward, even if local anesthesia was used. You can't get up for several hours. Within a week after ligation of the esophageal veins, certain areas die and become covered with fibrin. Necrotic vascular tissue falls off and is eliminated from the body naturally. Ulcers appear at the site of detachment, which scar after 3 weeks.
The patient is discharged no earlier than a week after the procedure. This is due to the fact that it is during this period that various complications may arise. Possible negative consequences:
- Severe pain in the abdominal area.
- Repeated bleeding.
- Development of the inflammatory process at the site of the latex ring.
- Allergic reaction to ligature material.
- Swallowing disorder. This is a fairly rare occurrence and is often associated with a psychological factor.
Complications
With the development of varicose veins, the likelihood of internal hemorrhage is high. It can be provoked by overeating, or increased physical activity, sudden lifting of weights, which will not lead to anything good if you ignore the first symptoms of the disease. Severe bleeding from esophageal varices can be fatal. Minor bleeding from the veins of the esophagus provokes the development of anemia or frequent vomiting. Bleeding from varicose veins of the esophagus is always dangerous to human health.
Against the background of vascular disorders, inflammatory processes in the esophageal mucosa are often noted. Gastric juice flows into the esophagus at different intervals. This creates a burning sensation and makes it difficult to swallow food.
Rehabilitation period
After ligation of the dilated veins of the esophagus, upon arrival home, the patient must strictly follow all medical instructions. Otherwise, serious complications may develop.
The main condition for a speedy recovery is diet. Starting from the second day, the patient is transferred to table No. 1. Food should be boiled and ground through a blender. The duration of the diet is about a month. Subsequently, the patient is transferred to table No. 5. For 3 years, it is not recommended to engage in sports and serious physical activity. If your previous job does not allow you to do this, you will have to change it. Surgery does not involve the removal of an important organ, so it does not result in disability.
Doctors advise visiting special sanatoriums with mineral waters. In addition, they have developed a special daily routine with procedures that promote rapid recovery.
You need to know that esophageal varicose veins are incurable. After surgery, all measures must be taken to prevent re-bleeding.
Recovery period
The patient is allowed to get out of bed and walk around the ward several hours after the operation; at this time the patient can only drink and does not eat any food.
Nutrition after ligation of esophageal varices
From the second day the patient is transferred to table No. 1 according to Pevzner. Food should be soft, pureed, cool. If pain bothers you, the patient is given Almagel A; if the pain does not subside, painkillers are prescribed. The pain usually goes away on its own after three days.
On days 4–5, rejection of the ligated varixes begins, and superficial ulcers form in their place. Diet at this time, as during exacerbation of erosive esophagitis, is one of the main methods of treatment during this period.
Patients should accustom themselves to eat regularly, in small portions, avoiding hyperphagia. Food must be boiled or steamed.
An approximate menu during this period could be like this:
| Eating | Dishes and products |
| 1 | Mashed buckwheat |
| 2 | Unsweetened kefir |
| 3 | Purated pearl barley soup, steamed fish cutlets |
| 4 | Dried fruits compote |
| 5 | Vegetable puree, weak tea |
After three weeks, the ulcers heal, leaving star-shaped scars.
If the patient does not have complications or new varixes, then the further course of the disease and the patient’s ability to work determines the course of the cirrhotic process.
Prevention
In order to avoid ligation of the esophageal veins in cirrhosis, it is necessary to take all measures to prevent and timely treat this disease. You should be regularly examined and see a hepatologist. Internal hemorrhages are very dangerous and often lead to death. To avoid disastrous consequences, you should be examined by a gastroenterologist.
People prone to varicose veins should adhere to a special diet. Fried, spicy foods should be excluded, food should be chewed properly. Dishes should not be too cold or hot.
You should completely stop drinking alcohol. You should not lift weights, but it is also extremely undesirable to lead a passive lifestyle.
Surgery is an extreme, albeit effective, method of therapy. In order not to resort to its use, at the slightest abnormal manifestations, you must visit a doctor.
Development of the disease
A change in the structure of the veins in the esophagus becomes an extreme stage of liver disease. Connective tissue replaces healthy liver parenchyma. The vascular network located inside the liver is compressed. The pressure in the portal vein increases. This condition changes blood circulation. Redistribution of blood increases the load on the veins and vessels in the digestive tract. The vein takes on a tortuous shape. The walls of the blood vessels change their structure: some become elastic and collapse, others become fragile and are susceptible to injury. Veins begin to protrude into the esophagus.
The likelihood of death if internal bleeding occurs is high. Portal hypertension syndrome is one of the manifestations of problems with veins in the digestive system
.
To establish an accurate and correct diagnosis, varicose veins in the digestive system are divided into four degrees:
- Dilatation of blood vessels. Differs in isolated cases. Detected during endoscopic examination.
- Localization of competing veins in the lower third. To diagnose the disease, a method using air is used. At the same time, the organ does not increase in size, and the pathology in the thickness of the walls is easy to visualize.
- Protrusion of veins not only in the lower part, but also in the middle. During the examination, it is possible to see problem areas not only in large vessels, but also point dilations in small ones.
- Vessels with varicose nodes. They do not deform when air is supplied. Erosion occurs against the background of thin mucous membranes.
The veins in the esophagus dilate for several reasons:
- liver diseases of various etymologies, including cirrhosis due to prolonged alcohol consumption, viral hepatitis, tuberculosis;
- formation of thrombotic formations;
- high blood pressure;
- constriction of the portal vein.
Prevention of complications
After ligation, preventive measures should be taken. This is necessary to prevent the development of complications.
You cannot immediately return to your old lifestyle and put stress on the area injured by the operation.
Alcohol should be completely avoided after ligation. It is one of the risks of developing complications after surgery. You should absolutely not drink alcohol for 30 days after surgery.
.
During this time, the affected area will have time to recover. It is advisable to eliminate alcohol completely for 6-12 months.
.
The following circumstances pose a risk of complications:
- Poor blood clotting. This needs to be clarified before surgery (coagulability tests).
- Having bad habits.
- Severe prolonged bleeding.
- Diseases of the gastrointestinal tract, heart, kidneys, lungs.
- Chronic infections.
- Old age of the patient.
- Some types of medications that cannot be stopped.
Ligation for varicose veins is an effective surgical treatment method. The advantages of this procedure are obvious.
The ease of the operation and the short recovery period make ligation one of the leading methods of treating varicose veins.
A procedure such as ligation of the esophageal veins is considered one of the more effective methods of eliminating bleeding that occurs due to vasodilation in liver cirrhosis. The operation is performed plannedly or in emergency cases and does not require special preparation of the patient. It refers to minimally invasive surgical interventions that are characterized by minimal trauma to soft tissues.
How is ligation performed?
The intervention is carried out in a specially equipped sterile room. Local anesthesia is generally used, and sedatives and painkillers are administered if necessary. The patient is placed on the left side, so that a tube is inserted into the oral cavity to pump out fluid. Next, an endoscope with a special attachment is inserted into the esophagus and brought to the varicose node. Using a vacuum, the changed area is absorbed. Finally, the ligator of varicose veins of the esophagus fixes latex rings, which tightly tighten the vessel and stop bleeding.
After ligation, some complications may occur that require immediate medical intervention. These include:
After surgery, the patient's condition may be complicated by a rise in temperature.
- increased body temperature;
- recurrent bleeding;
- blood poisoning;
- pathological breathing;
- violation of swallowing functions;
- pain in the peritoneum;
- general weakness;
- dizziness.
After ligation of the esophageal veins, additional drug therapy is possible.
The most unfavorable consequence of liver cirrhosis is an increase in pressure in the portal system. And the most dangerous complication is bleeding from pathologically dilated (enlarged) esophageal veins. Scientists are constantly working to improve methods for preventing bleeding. One of the new methods used today is endoscopic ligation of esophageal varices.
Ligation procedure for esophageal varices
By replacing normal hepatic parenchyma with connective tissue, which, in turn, compresses the intrahepatic vessels, compression in the portal venous system increases. Which causes a redistribution of blood flow in the veins of the esophagus, spleen, and rectum, contributing to their dilatation (expansion) and the development of massive bleeding. In the first 2 years of the disease, the risk of bleeding occurs in 25–40% of patients. Mortality after the onset of bleeding from varicose veins of the organ is recorded in 50–70% of cases. A second episode of recurrent bleeding occurs two years later in all patients and leads to death in 30–50%.
The above-described pathological process of restructuring of the vascular bed occurs not only with cirrhosis of the liver against the background of alcoholism or viral hepatitis. A thrombus in the portal vein, compression by a tumor, congenital vascular pathologies, taking medications (cytostatics, anti-tuberculosis drugs), congenital cirrhosis of the liver in newborns cause the opening of portacaval and cava-caval anastomoses. Rare causes of the syndrome we are considering include chronic heart failure initiating cirrhosis of the liver, Randrew-Osler disease and others.