Esophagitis in children is a fairly common pathology among diseases of the esophagus. Characterized by inflammation of the mucous membrane. In severe cases, the deeper layers of the esophagus undergo changes. Esophagitis can develop as an independent disease or occur against the background of other diseases. The cause of the disease is the release of stomach contents into the esophagus (reflux). If the condition recurs, serious consequences are likely to occur: the formation of ulcers, scarring of the esophagus, its narrowing or shortening. Over time, the disease can lead to cancer pathologies.
Reflux observed in infants, in most cases, is not considered a pathology, since it is caused by the fragile muscular system of the esophagus and sphincter, the sphericity and small size of the stomach, its rapid filling and slow emptying. Therefore, in the first 3 months of a baby’s life, regurgitation after eating and hiccups are considered common occurrences. The condition does not require treatment, you need to feed the baby at an angle of 60 degrees, after feeding you need to keep him in an upright position so that the air trapped in the stomach comes out. You need to place the baby on its side so that when regurgitating, the food mass does not get into the respiratory tract. If you are prone to frequent reflux, your baby should be put to sleep with the upper part of the body slightly higher. You can put it on your pillow.
Preventive measures help prevent the development of esophagitis.
Diagnosing reflux esophagitis in childhood is quite difficult, since the child cannot explain what is bothering him. Treatment of esophagitis in children is also complicated by the fact that many medications are not allowed to be used in childhood.
What it is
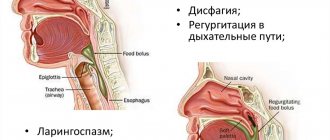
Esophagitis is an inflammatory process caused by the release of stomach contents into the esophagus. Under normal conditions, the contents of the stomach cannot enter the esophagus, since the muscular sphincter in the lower part of this organ is closed and prevents this. It opens in time to introduce food into the stomach and closes in time. When the function of the sphincter is impaired and the muscle ring does not close completely, gastric juices and acids enter the esophagus along with digested food. Contact of stomach contents with the mucous membrane causes the development of reflux esophagitis.
Reflux esophagitis also occurs in healthy children, and the condition is short-term in nature, so the child does not feel any changes or discomfort.
When the condition recurs in a periodic manner, causing the child to feel unwell, it is necessary to seek medical help.
Complications
The most common complication of congenital atresia, stenosis, esophageal-tracheal and bronchoesophageal fistulas is aspiration pneumonia. Esophageal atresia can lead a child to starvation within a few days. With stenosis, congestive esophagitis develops. Compression of the bronchi by the double esophagus causes repeated pneumonia and the development of bronchiectasis. When their cysts increase significantly, they can compress the esophagus and cause dysphagia. Suppuration of cysts and breakthrough of pus into the respiratory tract or pleural cavity are possible. The lining of cysts from the ectopic gastric mucosa may undergo ulceration with the development of bleeding and perforation. With a congenital short esophagus and insufficiency of the lower esophageal sphincter, reflux esophagitis, peptic ulcer, and then esophageal stricture occur; A common complication is aspiration pneumonia.
What does it look like
As a result of the development of reflux esophagitis, you can see changes in the contours of the esophagus, ulcerations, swelling of the walls and accumulation of mucus.
During normal functioning, the muscle ring opens the lumen for the passage of food into the stomach through the esophagus and closes it tightly in a timely manner, since the peristalsis of the sphincter is not impaired.
When the muscle ring is weakened and its functionality is impaired, a pathological condition is observed. Stomach acid travels back into the esophagus with food. Gastric juice in the mass coming back causes irritation and inflammation of the esophageal mucosa. As a result of an anatomical anomaly, the stomach protrudes through a weakened diaphragm.
Congenital bronchoesophageal and esophageal-tracheal fistulas
Duplication of the esophagus is a rare anomaly. The lumen of the second, abnormal esophagus may have a connection with the main canal of the esophagus, sometimes it is completely filled with secretion secreted by the mucous membrane. The abnormal tube can be completely closed, then it has the appearance of cysts that can communicate with the trachea or bronchus. As the cysts grow, symptoms of compression of the esophagus and airways develop. In this case, patients develop dysphagia, cough, and shortness of breath.
Congenital chalazia (cardia insufficiency) is a consequence of underdevelopment of the neuromuscular apparatus of the lower esophageal sphincter or straightening of the angle of His. The clinical picture is similar to those of congenital short esophagus.
Congenital short esophagus is a developmental defect in which part of the stomach is located above the diaphragm. The clinical picture is due to cardia insufficiency, accompanied by gastroesophageal reflux. After feeding, children experience regurgitation and vomiting (sometimes mixed with blood as a result of the development of esophagitis).
Symptoms
In infants, the cause of reflux may be an overfilling of the stomach with food, or rarely, a food allergy or narrowing of the esophagus. Children may have congenital or acquired pathologies of the digestive system.
In older children, reflux develops as a result of gastroduodenal diseases, mainly with insufficiency of the cardiac sphincter, with acute or chronic gastritis, with stomach ulcers and 12 signet rings. In school-age children, reflux can develop as a result of irregular nutrition and excessive consumption of sweets, fatty foods, and sweets.
Parents should be attentive to the child’s complaints when they notice restlessness and refusal to eat for a long time. Symptoms of the disease may be nonspecific and can be confused with other diseases. The child may experience:
- Lack of appetite for a long time;
- Bad breath, especially alarming if the baby does not have dental problems;
- Hiccups, signs of suffocation;
- Changing the timbre of the voice;
- Cough not associated with colds;
- Difficulty swallowing;
- Inflammatory process in the ear;
- Previous destruction of baby teeth.
In newborn babies, reflux almost always occurs. Regurgitation is considered normal when it is rare and the baby does not lose weight. In a healthy child, reflux rarely appears after the 4th month, and completely disappears by the 10th month. During this period, the condition does not require treatment. If your child experiences reflux again after this, you should consult a doctor. In infants the disease occurs:
- Colic;
- Formation of gases in the intestines and difficulties in their passage;
- Repeated swallowing of food.
In some cases, reflux can be dangerous to your health. You should immediately consult a doctor if you observe the ineffectiveness of conventional medications against reflux and if your baby is rapidly losing weight. Alarming symptoms are:
- Difficulty swallowing food;
- Black color of vomit or traces of blood in it;
- Sudden fever;
- Hiccups that do not go away for a long time;
- The chair is black.
Main symptoms
With reflux esophagitis, the following symptoms may occur:
- regurgitation that occurs in an infant;
- Older children may indicate a bitter taste in the mouth, burning pain in the chest;
- anxiety of the baby, manifested in moodiness, crying;
- delay in the development of the child, which is typical for regular and profuse regurgitation.
At an early stage of the disease, pain begins to bother you immediately after eating. In an infant, reflux is characterized not only by regurgitation, but also by constant vomiting and insufficient weight gain. In addition, parents may notice that the baby has a poor appetite or no appetite at all, a specific smell from the mouth, a cough without signs of diseases of the respiratory system, as well as frequent hiccups, ear infections, voice changes and choking.
Signs
Signs of gastroesophageal reflux in children under 5 years of age can manifest themselves in different ways. The baby may complain of an unpleasant bitter-sour taste in the mouth, and may refuse to eat, since pain appears after each meal. The child's breathing becomes difficult, especially when the little patient suffers from asthma, weight begins to decrease, and vomiting appears.
In older children and adolescents, it is easier to determine the disease, as they can describe pain and discomfort. Specific signs are:
- An acidic taste in the mouth or esophagus;
- Nausea;
- Heartburn, burning and pain in the chest (middle of the chest);
- Pain during eating;
- Feeling of poor passage of food through the food pipe.
The pain may worsen during sleep.
Signs of the disease in one-year-old children are arching of the back or neck from pain, vomiting, refusal to feed, crying before and after feeding.
GERD in children
Symptoms of gastroesophageal reflux disease in children are divided into two groups: those associated with the gastrointestinal tract (esophageal) and those not associated with the gastrointestinal tract (extraesophageal). In infants and preschool-age patients, the main clinical manifestations of GERD are vomiting (rarely streaked with blood), regurgitation, and insufficient weight gain. In some cases, disturbances in the functioning of the respiratory system occur, leading to respiratory arrest or sudden death. In adolescents and children of the older age group, the picture of gastrointestinal disorders is more clearly visible, heartburn and dysphagia are observed. Regardless of age, GERD may cause weather dependence, insomnia, headaches and emotional instability.
Esophageal manifestations are a direct consequence of the impact of refluxed contents on the wall of the esophagus. The primary and most common (but not obligatory) symptom is heartburn. Subsequently, regurgitation and belching of sour or bitter foods occur. Many patients have a “wet spot” symptom, in which a whitish mark remains on the pillow after sleep. The cause of its development is hypersalivation, which is characteristic of impaired motility of the cardiac esophagus. Odynophagia (pain behind the sternum while eating) and dysphagia, manifested by a sensation of a lump in the chest, may be observed. Sometimes there are no clinical manifestations of gastroesophageal reflux; changes are revealed only during instrumental examination. The opposite option is also possible when, with severe clinical GERD, endoscopic signs of the disease cannot be detected.
All extraesophageal symptoms of gastroesophageal disease in children are divided into groups. Most often, GERD is accompanied by bronchopulmonary manifestations (up to 80% of cases). Bronchial asthma and broncho-obstructive syndrome are usually observed, accompanied by paroxysmal cough or shortness of breath after eating and at night. Often these symptoms are combined with belching and heartburn. With adequate treatment of GERD, bronchial obstruction decreases or completely disappears. Typical otolaryngological symptoms include sensations of tickling and food stuck in the throat, hoarseness of the voice, a feeling of pressure in the neck and upper chest, ear pain and coughing that is not dependent on food. Cardiac manifestations of GERD are caused by the esophagocardial reflex, which can cause sinus arrhythmias, extrasystoles and the phenomenon of slowing intraatrial conduction - an increase in the PQ interval. Odontogenic symptoms of GERD include the formation of erosions on tooth enamel.
Classification and degrees
Pathological reflux occurs in acute and chronic forms.
The acute form of the disease develops against the background of existing gastrointestinal diseases. The main symptoms of this form are disruption of the gastrointestinal tract, the presence of a source of infection in the body, and vitamin deficiency. The baby looks unhealthy, has difficulty swallowing, and chest pain.
The chronic course of the disease manifests itself as a complication of another disease of the digestive system. Infrequently, esophagitis occurs primarily, which is due to the specific nutrition. The chronic form of reflux occurs with severe symptoms.
Depending on the nature of the disease in a child, the following types of reflux are classified:
- Catarrhal. There is a superficial lesion of the mucous membrane without an erosive process. Manifests itself as a result of exposure to a mechanical or thermal stimulus. Conservative therapy is used for treatment.
- Hydropic. This type is characterized by thickening of the walls of the esophagus, swelling of the mucous membrane, and the esophagus narrows.
- Exfoliative. It is a severe form of the disease. There is separation of fibrin from the mucous membrane, which provokes severe coughing, soreness, bleeding and perforation of the esophagus.
- Pseudomembranous. It occurs with the formation of a gray-yellow film of fibrin on the mucous membrane, which over time gives way to ulcers and erosive formations. The child experiences nausea and vomiting; film fragments are found in the vomit.
- Erosive. A serious form of reflux is esophagitis. It occurs with redness of the mucous membrane, the development of microabscesses, and swelling of the esophageal glands. The solution to the problem is surgery.
There are four degrees of development of the disease. The symptoms and treatment regimen depend on the degree.
- In the first degree of pathological reflux, irritation of the esophagus by stomach contents is observed. Under the influence of the aggressive substance contained in the mass, the mucous membrane of the esophagus swells, becomes red, and isolated erosive lesions are recorded. Symptoms at this stage are absent or mild.
- In the second degree, esophagitis occurs with certain symptoms, which is associated with erosive damage to the esophageal mucosa. Spots measuring 3–6 mm in size are observed on the mucosa, which sometimes merge, gradually covering the entire surface of the esophagus.
- The third degree of pathology in a baby is characterized by severe symptoms. Difficulty in the swallowing process, severe pain, the formation of defects in the esophageal mucosa, and a feeling of discomfort in the stomach area are recorded. At this degree, damage to the esophagus occupies more than 70%. Ulcerative lesions merge. The child complains of a burning sensation and heaviness in the chest, especially after eating.
- The fourth degree is expressed by large-scale ulcerative lesions of the esophagus (more than 75%). The symptoms are more pronounced and constantly bother the child. The patient complains of pain in the stomach area, an unpleasant taste in the mouth, swallowing becomes impossible due to severe discomfort and burning. This stage is the most dangerous and difficult for the baby, since this is the point after which there is a risk of developing gastrointestinal cancer.
Pathological reflux is detected in most cases from the second degree, when the symptoms become severe. In the third and fourth degrees, surgical intervention is often resorted to.
Among the extraesophageal manifestations there are:
- Bronchopulmonary;
- Otolaryngological;
- Cardiological;
- Dental.
Forms and degrees
A disease such as reflux esophagitis, which occurs in children and adults, has degrees of severity. The first of which is due to the presence of separate erosive formations that do not come into contact with each other. Degree No. 2 is characterized by merging erosions that do not spread along the top of the mucous layer of the membrane. The next degree is the third, it is characterized by the formation of confluent ulcers in the lower part of the esophagus. Ulcerative lesions cover the entire surface of the organ mucosa. The last degree is the fourth, which is caused by the appearance of stenosis of the esophagus and the formation of a chronic ulcer.
In medical practice, the following forms of GER are distinguished:
- Spicy. The acute form of the disease has the following symptoms: increased body temperature, pain in the chest, difficulty swallowing food and liquids, belching, a burning sensation in the esophagus and increased salivation.
- Chronic. With a chronic inflammatory process in the esophagus, difficulty breathing, vomiting, hiccups, painful sensation in the chest and heartburn are observed.
In addition to two main forms, the disease also has morphological ones. This:
- Catarrhal. The inflammatory process forms on the surface of the mucous membrane of the organ and does not have a destructive effect on the tissue.
- Erosive. This form of GER is characterized by deep erosive lesions that occur on the mucous layer of the esophagus. In the erosive form of the disease, the following symptoms are present: burning behind the sternum, severe belching, nausea, periodic vomiting and the sensation of a foreign object in the throat. This symptomatology in the erosive form of reflux esophagitis is more pronounced and causes more discomfort to the patient.
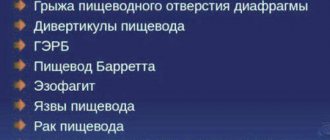
ICD 10 code
According to ICD-10 (international classification of diseases), esophagitis refers to diseases of the esophagus, stomach and 12 rings. Reflux - esophagitis according to ICD - 10 has a classification K 21.0 - reflux with esophagitis, K 21.9 - without esophagitis.
The Savary Miller classification is also used:
- Grade A. The affected area of the esophagus reaches up to 4 mm, ulcers are observed that do not merge with each other;
- Grade B. The affected area is enlarged to 5 mm. Erosion areas may merge in places;
- Grade C. The area affected by ulcers reaches up to the 5th part of the esophagus;
- Grade D. The esophagus is 75% affected.
Treatment options
Treatment tactics for GERD depend on the age of the child and the degree of structural changes in the esophagus. To get rid of the disease, you need an integrated approach.
Eliminating reflux without drugs
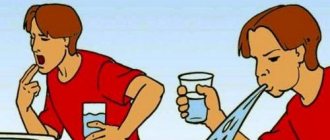
For infants and preschoolers, the treatment regimen mainly includes non-drug correction. This includes changes in body position and diet. Feeding babies is carried out at an angle of 50-60°. If the child is bottle-fed, pediatricians recommend choosing formulas with an anti-reflux effect. This food is released with the mark “AR”. During sleep, the position of the head and upper torso should be elevated to avoid reflux.
Mild forms of GERD in school-age children are treated with diet and changes in sleep position. The head end of the bed is raised by 15-20 cm. This measure reduces reflux. In some cases, eliminating the factors that provoke the reverse movement of the food bolus helps: giving up medications that cause pathology, reducing physical activity associated with increased intra-abdominal pressure.
If the disease is associated with obesity, weight loss measures are taken. In this case, the child needs to consult an endocrinologist, because Excess weight is usually associated with hormonal imbalances.
Medicines
The doctor makes the decision to prescribe drug therapy taking into account the general condition of the child and the complaints of the parents. The treatment regimen includes drugs:
- proton pump inhibitors (PPIs) – Rabeprazole, Pariet;
- Histamine H2 blockers – Ranitidine;
- prokinetics - Motilium, Motilak;
- agents regulating gastrointestinal motility - Trimebutin, Trimedat;
- non-absorbable antacids - Maalox, Lactamil, Gaviscon;
- enzymes – Creon, Pancreatin.
The combination of medications is selected based on the age of the child and the complexity of the disease.
Antacids help when used in combination with other medications. When taken alone, they help relieve heartburn and reflux, but symptoms return after 4-5 hours.
The duration of the course of therapy for the superficial form of esophagitis is 10-14 days. The treatment regimen includes prokinetics and non-absorbing antacids. Healing of erosions and ulcers will take more time, since the inflammatory process involves deep layers of the mucosa. Single erosions that do not merge with each other are treated with H2-blockers of histamine receptors and prokinetics for 2-4 weeks. At the discretion of the doctor, the treatment regimen can be supplemented with enzymes and agents that normalize peristalsis. Complicated degrees of esophagitis with confluent ulcers, erosions, and persistent vomiting are treated with proton pump inhibitors and prokinetics. The course of therapy is 1-1.5 months.
The effectiveness of treatment depends on nutrition and lifestyle. If you irritate the esophagus with prohibited foods, recovery may be delayed.
Diet
Nutrition correction is carried out for any form and degree of esophagitis. Gastroesophageal reflux in a child should be treated with a special diet.
Basic principles:
- you need to eat in small portions 5-6 times a day;
- avoid hunger and large meals;
- meals are taken without haste and at certain hours;
- reduce (during the course of therapy eliminate) the consumption of foods that cause reflux - coffee, chocolate, carbonated drinks, fats;
- limit vegetables with coarse fiber - garlic, fresh onions, radishes, white cabbage;
- during the diet, avoid foods that increase acidity - tomatoes, millet, pearl barley, pickles, smoked meats, fast food, kvass;
- do not eat 2-3 hours before bedtime;
- The food should be consumed warm.
Surgical intervention
The operation is performed if conservative therapy does not produce results or complications arise. Surgery is indicated when GERD is combined with a diaphragmatic hernia or severe airway obstruction.
With timely treatment of GERD, the prognosis is favorable. Superficial esophagitis is completely curable. Complicated forms of the disease require systematic monitoring by a specialist.
We recommend: What does a diet for GERD include and why should it be followed?
Clinical guidelines
Clinical recommendations of pediatricians are based on the study of anamnesis, clinical and laboratory data and the results of instrumental studies. With the help of anamnesis, the pediatrician is able to determine the presence of dysphagia, wet spot symptom and other typical manifestations. The CBC may reveal a decrease in the level of red blood cells and hemoglobin (with posthemorrhagic anemia) or neutrophilic leukocytosis and a shift in the leukocyte formula to the left (with bronchial asthma).
The doctor prescribes endoscopic diagnostics - fibrogastroduodenoscopy, which allows you to detect pathology on the mucous membrane, take biomaterial for research, see anatomical anomalies of the esophagus, and assess the condition of the stomach.
Pressure measurements inside the gastrointestinal tract, ultrasound, and contrast radiographic examination are also carried out, with the help of which hernias, narrowings, and evacuation dysfunction of the upper gastrointestinal tract are detected. An important indicator is the procedure for daily measurement of pH inside the esophagus.
Treatment regimen
If gastroesophageal reflux disease is not complicated (first or second degree), infants are treated with a simple change in diet:
- Reduce food portions; overeating should not be allowed;
- Avoid contact of the baby with tobacco smoke;
- Whole milk is removed from the diet.
If a child experiences excessive and frequent regurgitation, this can lead to dehydration and disruption of water and electrolyte balance. In such cases, the baby’s treatment is organized in a hospital setting using infusion solutions.
For children beyond infancy, treatment is selected by specialists based on research, taking into account the individual specifics of the child’s body.
The following groups of medications are used:
- PPIs are proton pump inhibitors. Block the formation of hydrochloric acid. Omeprazole and Pantaprazole are used. Omeprazole is recommended for the treatment of children from 2 years of age.
- H2 blockers - histamine receptors. Reduces the acidity of gastric juice. These include Ranitidine, Famotidine. Not allowed to be used to treat children under 1 year of age.
- Antacids. Neutralizes hydrochloric acid and restores damaged areas of the mucous membrane. Phosphalugel, Maalox, Gaviscon are prescribed.
- Prokinetics. They activate the contraction of the stomach muscles, increase the tone of the esophageal sphincter, normalize the process of gastric emptying, and reduce reflux.
- Enzyme medications that help digest food.
- Medicines to combat flatulence. It is recommended to use the drug Melikon.
The above drugs are used in symptomatic therapy, but do not eliminate the cause of the disease.
In most cases, the third and fourth stages of reflux esophagitis require surgical intervention.
Indications for surgery are:
- Ineffectiveness of long-term drug treatment;
- Severe pain (pain does not subside after taking painkillers);
- Deep damage to the mucosa, when multiple erosions and ulcers are recorded, occupying a large extent of the organ;
- Aspiration syndrome;
- Severe airway obstruction (complication of esophagitis).
The operation is performed by laparoscopic fundoplication, during which the sphincter muscle in the lower part of the esophagus is strengthened.
Drug treatment
Drug therapy is prescribed by specialized specialists in the initial stages (first and second) with mild symptoms that can still be corrected by taking medications. Appointments are made after research and taking into account the patient’s characteristics. The following groups of drugs are used:
- PPI proton pump inhibitors (omeprazole, pantaprazole) - they block the formation of hydrochloric acid. Omeprazole is the “gold standard” in the treatment of reflux in children from the age of two.
- H2 blockers - histamine receptors (ranitidine, famotidine) - reduce the acidity of gastric juice, their mechanism of action differs from PPIs, and are not used in children under one year of age.
- Antacids: the purpose of their use is to neutralize hydrochloric acid, restore damaged mucous membranes (Phosphalugel, Maalox, Gaviscon).
- Prokinetics (Domperidone, Coordinax, Motilium, Cisapride) - increase contractions of the stomach muscles, increase the tone of the esophageal sphincter, promoting faster gastric emptying, reducing reflux.
- Enzyme preparations promote better digestion of food.
- Anti-flatulence drugs (Melicon).
Taking these drugs is symptomatic therapy; they do not eliminate the cause of the disease.
With frequent and profuse regurgitation, the child becomes dehydrated and has an imbalance in water and electrolyte balance. In such cases, treatment is carried out in a hospital setting using infusion solutions.
Without exception, all medications have side effects and contraindications. Therefore, treatment of a child should be carried out only by a specialist and be fully justified.
Folk remedies
Herbal teas and decoctions of medicinal herbs are effective for the treatment of esophagitis in children. Before using traditional medicine recipes, be sure to check the baby’s body’s reaction to the formulations used and consult a doctor.
Collection of thyme and marshmallow
Thyme and marshmallow rhizomes are taken in equal quantities. 40 g of the collection is poured into 250 ml of boiling water and left for 2 hours.
Tincture of mint, valerian and celandine
A herbal mixture is prepared from mint, valerian, celandine (2:2:1). 20 g of the collection is poured into 250 ml of boiling water and heated in a water bath for 20 minutes.
Dill tincture
2 tsp. Ground dill seeds, pour 200 ml of boiling water, leave for 3 hours. The infusion is consumed after straining, 3 times a day, 1 tbsp. l. before eating.
Sweet water or water with flower honey (1 tbsp. Product per 1/3 warm water), which is prepared overnight and given to the child in the morning, is useful.
Prevention
To prevent the development of esophagitis in children, you need to monitor their lifestyle and routine. You cannot smoke in front of a child; teenagers need to be explained the harm of smoking and alcoholic beverages to the body. The baby's diet should include only healthy foods; more fresh vegetables and fruits are needed.
It is necessary to feed the child after checking the temperature of porridge and drinks. Eating very hot or cold food is not allowed. To avoid chemical burns, household chemicals should be stored out of the reach of children. During the treatment period, a gentle diet is recommended. Regular examinations by specialized specialists are recommended, which will allow timely detection and treatment of pathology, preventing possible complications.
All parents should remember that self-medication is dangerous to the child’s health.
Symptoms of esophagitis in children
The clinical picture of the acute form depends on the degree of the inflammatory process. The catarrhal type of esophagitis is not accompanied by any symptoms. When deeper layers are affected, the most common manifestations of the disease are painful swallowing and discomfort when eating hot or cold food. In the severe stage, the symptoms of reflux esophagitis in children are:
- burning pain behind the sternum;
- mild or sharp pain when swallowing;
- dysphagia;
- constant heartburn;
- excessive salivation.
After a few days, the symptoms of esophagitis in children may become less intense. However, after a couple of weeks, the sick child develops rough scars on the walls of the esophagus, leading to the development of stenosis. This condition is fraught with progression of dysphagia and food regurgitation. Therefore, at the first symptoms of the disease, you should contact a specialized clinic for a complete diagnosis of the stomach and intestines.
The chronic form of reflux esophagitis in children manifests itself:
- frequent heartburn, which becomes more intense when taking fatty and spicy foods, carbonated drinks;
- the appearance of belching;
- heavy breathing during sleep.
A child suffering from chronic esophagitis is predisposed to frequent pneumonia and the appearance of bronchial asthma. Babies under 1 year of age suffer from frequent regurgitation immediately after feeding. One of the symptoms of reflux esophagitis in children is malnutrition (lack of body weight in relation to its length).
Diet
For infants, breastfeeding is the best option. Food thickeners (corn, potato, rice starch) are added to the menu. This will help prevent food from flowing from the stomach into the esophagus. According to American scientists, a maximum of 1 tablespoon of thickener per 30 ml of liquid can be added to the food of a child from 0 to 3 months.
A gentle diet is used for preschool children and adolescents. The diet is prepared taking into account that food intake is regular and divided. You need to eat 6 times a day, in small portions at precisely set times.
The child should eat only freshly prepared meals from foods that are easy to digest. It is necessary to exclude legumes, fibrous foods, and fruits with skins.
All drinks and dishes should be used warm (not hot), since the inflamed mucous membrane is sensitive to the temperature of the food used.
It is recommended to include cereal soups, vegetable broths, boiled and chopped meat and fish, pureed porridges, and jelly in the diet. You should not give your child rich soups, hot, spicy, or sour dishes. The use of sweets with dyes, chocolate, fast food, sausage, fresh bread, sweet products, and carbonated drinks is prohibited. Water should be given little by little, but regularly.
Treatment of esophagitis in children is complicated by the fact that young patients find it difficult to explain what is bothering them. Parents should be attentive to their child’s behavior and consult a specialist at the first sign of digestive problems. Timely treatment of the child prevents the disease from progressing to a more complex stage of development, making it possible to quickly and effectively cure the child using medications.