Among the world's doctors, there is no unified classification of gastric and duodenal ulcers that would suit scientists to the same extent. Gastric ulcer is a polymorphic disease, often susceptible to chronicity and the development of complications. In different time periods, scientists proposed many classifications, which were based on various clinical, pathomorphological and pathogenetic criteria for disorders of the stomach and duodenum. The gradation of the ulcerative process is similar to the pathological conditions of a sigmoid ulcer.
Foreign Western literature often contains the term peptic ulcer. Western doctors and researchers clearly distinguish in practice the concepts of peptic ulcer of the stomach and peptic ulcer of the duodenum. The abundance of classifications of the disease once again emphasizes how incomplete and imperfect the described gradations are.
World Health Organization classification
According to this classification, the types of disease are divided:
- Stomach ulcer.
- Duodenal ulcer.
- Acute, having an unspecified location.
- Developed on the stomach after resection.
A patient has a stomach ulcer
For everyday clinical practice, such a classification of defects of the stomach and duodenum is insufficient. It is usually used for the purpose of recording and maintaining medical statistics. In order for the classification to be suitable for practical activities, it is necessary to refine and expand the lists; it is necessary to take into account the localization of the ulcer in the rectum or sigmoid colon.
...and after surgery
Despite the wide possibilities of modern pharmacotherapy, a number of patients with peptic ulcer disease require surgical treatment. The first day after surgery in a hospital setting, the patient should refrain from eating. It is allowed to feed the patient from a spoon in small portions.
The next step is to introduce a small amount of broth of the second or third boil. Over the course of a week, new foods are added to the diet day after day. The ulcer menu includes jelly, strained soups, semolina, cottage cheese, and whipped boiled meat.
A post-operative diet for stomach ulcers at home involves split meals in small portions. The ulcer diet is prescribed for at least six meals. The table becomes more generous every month, but you will have to forget about smoked, fatty, spicy and alcohol.
If a patient with a peptic ulcer does not have concomitant ailments of the liver, pancreas and gall bladder, therapeutic diet No. 2 can be prescribed for the period of postoperative recovery. Table No. 2 is regarded as a transitional stage from a gentle to a rational menu.
The peculiarity is that foods that are difficult to digest are excluded from the diet. And also dishes that irritate the mucous membranes. Pieces of food are already appearing, which is important for training the operated organ. But it must be chewed thoroughly. It is recommended to adhere to treatment table No. 2 for up to seven days.
Current classification
The most common classification used for practical purposes is the one described below.
General principles of classification
- General clinical and morphological characteristics of the disease, coinciding with the nomenclature proposed by the World Health Organization.
- A peptic ulcer that primarily affects the stomach.
- Lesions of the duodenum.
- A peptic ulcer with an unspecified location is ulcerative lesions that simultaneously affect both organs, or when it is not possible to establish a reliably precise localization of the ulcerative lesion. Often the cause is irradiation of pain due to damage to the sigmoid colon.
- Peptic, which develops in patients who have previously undergone gastric resection. The variety is also called gastrojejunal or ulcer of the anastomosis connecting the remaining part of the stomach with the small intestine.
Classification according to clinical signs
The clinical classification of gastric and duodenal ulcers provides for the division of ulcers into acute and chronic. Acute cases include those diagnosed for the first time, who have not reached the age of three months. Processes that are older than three months or develop repeatedly are usually classified as chronic.
Classification according to the course of the disease
- Latent course – when the patient does not subjectively feel the clinical symptoms of an ulcer. In such a case, the diagnosis of peptic ulcer becomes a diagnostic finding during examination for a pathological process in the area of the sigmoid colon.
- Mild course - in which the clinical manifestations are erased, relapses of the disease do not appear for several years.
- The disease is of moderate severity and is characterized by relapses about 1-2 times every year.
- In severe cases of the disease, relapses occur more than three times a year, and the incidence of complications is extremely high.
Gradation of the disease by phase
- The exacerbation phase of gastric and duodenal ulcers is characterized by deterioration of the condition, increased clinical symptoms, and the appearance of severe pain. Often an exacerbation occurs in the autumn or spring months and is triggered by poor diet, stress, or taking medications that irritate the stomach.
- During treatment, a subacute or attenuated phase begins.
- Remission is a period of disappearance of acute symptoms of the patient’s clinical well-being.
Return of ulcerative pathology
Diagnostics
Diagnosis of pathology can be carried out by a therapist, gastroenterologist or surgeon.
Data collection and inspection
In the first stages, it is important to interview the patient, during which the doctor finds out the complaints, their nature, duration and frequency.
It is mandatory to establish the onset of the disease, find out the hereditary history, and the plan for previous treatment. A detailed examination will help the doctor detect inflammatory lesions of the eyes, skin or tongue, and joint contractures as a result of long-term arthritis. Palpation of the abdomen is carried out to determine the area of pain, pathological changes in the shape and size of the intestine, and bloating.
Instrumental studies
Invasive techniques allow a more detailed and “personal” examination of the intestinal mucosa, detect the nature and number of defects on it, perform a biopsy and even minor operations if necessary.
Be sure to read:
H2-histamine blocking drugs and their use in gastroenterology
To establish a diagnosis, the following types of instrumental diagnostics are prescribed:
- Fibrogastroduodenoscopy (with/without urease test). This is an examination of the upper segment of the gastrointestinal tract using an endoscope (from the esophagus to the duodenum). It is the “gold” standard for diagnosing peptic ulcer disease.
- Fibercolonoscopy. The rectum and colon are examined; It is possible to perform a biopsy and minor surgical interventions (stop bleeding, remove polyps).
- Contrast irrigography. X-ray examination of the intestine using a contrast agent and taking a series of images.
In addition to a visual assessment of the condition of the intestinal mucosa, a biopsy is required, followed by a histological examination of the collected material. This helps not only confirm the diagnosis, but also exclude oncology.
Laboratory research
Laboratory tests include clinical and biochemical blood tests (decrease in hemoglobin and albumin levels, appearance of C-reactive protein and fibrinogen).
In some cases, they resort to immunological analysis, which detects the presence and amount of plasma antibodies. A coprocytogram and bacteriological examination of stool can show the presence of undigested particles, leukocytes and a high concentration of pathogenic microbes. Equally important is a stool test for occult blood.
Classification by stages
- An active ulcer causes acute clinical symptoms, bleeds heavily, and leads to a number of complications.
- The scarring ulcer is gradually covered with connective tissue, bleeding stops, and the epithelium is restored.
- The red scar stage is characterized by the formation of active, well-supplied granulations that are easily damaged. Hence, the development of relapse or bleeding from granulations is possible.
- The white scar phase is characterized by the formation of rough scar connective tissue containing few blood vessels and nerves.
- They also consider the category of defects that do not heal for a long time.
What is remission of a stomach ulcer - Let's say no to diseases with iMes.website
Pathologies of the digestive system are dangerous for many reasons. First of all, they trigger problems in other body systems. One of the most dangerous diseases is gastric ulcer. Its presence means that a person will always have to adjust his lifestyle and be treated for exacerbations. But less attention should be paid to the disease in remission.
Remission of a stomach ulcer poses a great danger to health.
Features of the course of gastric ulcer in remission
Peptic ulcer is a pathology of the mucous membrane of the stomach wall. It manifests itself in the form of local defects in the surface of the organ and has a chronic recurrent nature. Without proper treatment, it progresses and, affecting other organs, leads to complications that are life-threatening. This disease is caused by a number of reasons:
- heredity;
- nutritional errors (eating spicy, coarse, fatty, smoked, too salty or hot foods);
- Helicobacter pylori infection;
- drinking alcohol and smoking;
- mental and physical stress.
These factors reduce the protection of the mucous membrane, which causes an exacerbation.
As a result, less gastric mucus is released, bicarbonates (components of gastric and pancreatic juice) are not produced, local blood flow worsens, and epithelial regeneration is weakened.
This stage of the disease is accompanied by severe cutting pain, nausea, vomiting and other negative symptoms.
There are three main phases of the disease:
- exacerbation;
- fading exacerbation;
- remission.
Fading exacerbation
In a state of exacerbation approaching the end, no symptoms of the disease are observed, and the ulcer is actively healing. In this case, there is still inflammation of the mucous membrane.
Sometimes there are “hunger” pains that go away after eating. Depending on the time that has passed since the start of treatment, the defect scar becomes white or red.
Before complete scarring, the ulcer heals unevenly and has red and white spots.
At this time, the patient finally feels good, he has an appetite and the pain, nausea, and heartburn go away. The main thing is not to interrupt the prescribed course of treatment and eliminate the Helicobacter pylori infection. Otherwise, chronic Helicobacter gastroduodenitis is activated and the ulcerative defect is renewed.
Complete remission
At this stage, the ulcer is completely scarred, and the symptoms of gastroduodenitis disappear. The stage is characterized by complete cessation of pain and absence of inflammation. However, an exacerbation can occur at any time, the catalyst of which is a violation of the diet, physical and psychological stress, alcohol, smoking, and a disrupted daily routine.
Prevention
To prevent ulcers, you must do the following:
- adhere to the day and night routine;
- follow a diet;
- prevent and promptly treat infectious diseases;
- undergo regular examinations with a doctor;
- carry out anti-relapse measures;
- go to sanatorium-resort treatment.
Sanatorium treatment
Preventive and therapeutic measures at sanatoriums include health-improving gymnastics, climatic procedures, drinking mineral water and electric warming techniques. Long-term normalization of the patient’s condition allows one to move from local resorts to remote climatic sanatoriums.
If the patient has had bleeding, then this type of prophylaxis should be postponed for more than 6 months. For patients with mild exacerbation, rest and drug treatment are recommended. During long-term recovery, the permissible doses of ultraviolet radiation and bicarbonate water are significantly increased.
Physiotherapy
An ulcer requires a change in a person's physical activity. Gymnastics reduces acid production, stabilizes gastric motility and has a beneficial effect on the nervous system. Therapeutic exercise is combined with the intake of mineral waters, combining alkalization and proper motor exercises. The course is selected by the attending physician.
Climatotherapy
Another stage of active treatment is walking and taking air baths. Along with them, heliotherapy is used, which often takes place in special aerosolariums. When sunbathing, you must follow the doctor’s instructions, do not exceed permissible radiation levels, and maintain intervals between procedures (at least 2 hours).
Treatment with mineral waters
The internal and external use of mineral waters has a beneficial effect on the health of a patient with peptic ulcer. This takes into account the peculiarities of the course of the disease, the characteristics of the condition of the stomach and other concomitant diseases.
Patients are prescribed to take sodium bicarbonate-sulfate and sodium bicarbonate waters. Usually they are drunk an hour and a half before meals, 8 times a day. People with acidosis are advised to drink mineral water after meals because otherwise drinking causes acid dyspepsia (an ulcer-like condition).
Source: https://imes.website/chto-takoe-remissiya-yazvy-zheludka/
Classification by location
Based on localization, processes are divided into gastric and duodenal. Each species is divided into several subspecies.
Ulcers in the stomach
- Damage to the cardiac part of the stomach.
- Process in the subcardial part of the stomach.
- An ulcer affecting the body of the stomach.
- Damage to the antrum.
- Damage to the minor or major curvature.
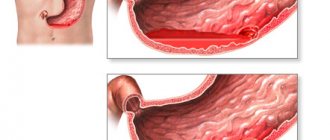
Damage inside the stomach and intestines
Duodenal ulcers
In the duodenum, the ulcerative process can develop in the bulb or in the postbulbar region. The ulcer affects the anterior or posterior wall of the duodenum. Localization is divided according to the lesser and greater curvature.
What is remission for stomach ulcers?
Exacerbation of duodenal ulcer is observed mainly in patients who do not adhere to the therapeutic and protective regimen, violate the prescribed diet, abuse alcoholic beverages, or are exposed to frequent and severe stress. These factors can lead to exacerbation of chronic peptic ulcer disease.
In addition to these reasons, seasonality plays an important role in the pathogenesis of exacerbation of peptic ulcer disease. Often, exacerbation attacks occur in patients during the off-season - spring, autumn. Doctors explain this circumstance by a decrease in the body’s overall resistance during the cold season. In the spring, the state of hypovitaminosis is involved in the pathogenesis of exacerbations.
Chronic peptic ulcer disease has a characteristic wave-like course: the exacerbation stage is replaced by a remission stage - a decrease in pain and other symptoms.
Possible forms of exacerbations
Clinical symptoms of exacerbation of duodenal ulcer are varied, showing differences.
- According to the frequency of occurrence, it is customary to distinguish between ulcers that rarely recur. The often exacerbating form is characterized by the occurrence of relapses more than 4 times per year.
- Based on the number of ulcerative formations, a single ulcer and multiple lesions of the mucous membranes are distinguished.
- Based on the location and depth of penetration into the tissue of the duodenum, the ulcer is divided into lesions in the area of the bulb or in the horseshoe of the duodenum.
- Damage to the mucous membrane can be superficial or deep.
What is the difference between relapse and remission?
The stage of stable remission in peptic ulcer disease has clinical distinctive features from the phase of exacerbation of the ulcerative process.
If an exacerbation of duodenal ulcer occurs, the clinical symptoms will be severe and accompanied by signs of dysfunction of the gastrointestinal tract.
When the disease enters the stage of remission, no acute severe symptoms are noted, the patient’s condition remains relatively satisfactory.
During the remission stage, the patient may not have clinical signs indicating the presence of an ulcerative process.
Abdominal pain due to ulcer
Pain in the epigastric region on the right side is a characteristic hallmark of duodenal ulceration.
Periodically, during an exacerbation, the patient feels pain in the interscapular area or in the heart area. What happens is due to the movement of pain sensations along the nerve trunks to other parts of the human body, creating false sensations, which are commonly called irradiation.
According to the observation of gastroenterologists, a characteristic feature of duodenal pain with any irradiation is pain in the central part of the abdomen in the navel area.
If the irradiation is characterized by a variable nature and can appear and disappear, then the pain around the navel persists constantly.
Hunger pains
Most often, pain in the epigastrium is observed in a person who has not eaten for a long time or is hungry. Similar pain may occur a couple of hours after eating. As soon as the patient takes a small amount of food, the pain disappears. If the patient has consumed foods that are not recommended for peptic ulcers, or has eaten too much, the painful sensations become more intense.
Patients often complain to their doctor that they cannot sleep at night due to intense epigastric pain. Attacks of pain are extremely severe and prolonged. What happens is due to the effect of hydrochloric acid on the mucous membrane of the empty stomach or intestines, corroding the surface of the ulcer.
During the period of remission, the patient can provoke a worsening of the condition if he violates the diet, takes alcohol, or contraindicated drugs. A person experiences an exacerbation of a duodenal ulcer.
Digestive dysfunction
Disturbances in the normal functioning of the digestive organs are characterized by the following symptoms:
- The appearance of flatulence, bloating.
- The appearance of sour belching.
- Nausea and profuse vomiting, after which the patient feels better. In some cases, patients, trying to get rid of painful sensations, induce vomiting on their own.
- Chronic constipation, lasting several weeks.
- The appearance of blood or occult blood in the stool.
General deterioration
Since exacerbation of peptic ulcer disease is severe and affects the general condition, patients become irritable and tired, complaining of insomnia and depression. Having said that, patients' appetite rarely suffers. Reducing the amount of food taken is due to the fear of pain after eating. The signs of increasing asthenic syndrome are described.
Principles of treatment
Treatment of duodenal ulcer is carried out using conservative or surgical methods.
Conservative treatment includes following a strict diet, taking medications, and, if desired, alternative medicine. In case of exacerbation, when the listed symptoms appear, treatment is carried out in a hospital setting.
If drug therapy turns out to be ineffective over a long period of time, or the patient develops serious complications, doctors decide to perform surgery on the small intestine. Often operations are performed for severe cicatricial deformities of the duodenal bulb.
If the patient is in a state of stable remission, he leads his usual lifestyle. At the same time, it is advisable to protect yourself from stress and overload, avoid alcohol and smoking. Under the current conditions, if a duodenal ulcer worsens, treatment proceeds much faster and healing occurs more intensively.
Diet for peptic ulcers
If a person is diagnosed with a duodenal ulcer in the acute stage, it is important to know the list of foods that will have to be abandoned. Such products have an irritating effect on the mucous membrane of the stomach and intestines and worsen the condition.
- Alcoholic, highly carbonated, sweet drinks.
- Hot spices, seasonings, savory sauces.
- Any fried foods, including vegetables and fish dishes.
- Coffee and caffeinated drinks.
- Rich mushroom or meat broths.
- Coarse black bread, fresh baked goods.
The above list is subject to exclusion from the daily diet during an exacerbation, in a state of stable remission.
Below is a list of dishes and foods that are preferable for ulcers.
- Vegetable and milk soups.
- Boiled lean meat, boiled or baked fish.
- You should eat yesterday's bread.
- Cereal dishes.
It is not recommended to consume raw vegetables containing coarse fiber - radishes, cabbage, beans, corn.
Principles of therapeutic nutrition
The nutrition of patients suffering from peptic ulcers is based on the rules.
- The number of meals during the day is at least five.
- The amount of food per serving should not exceed the volume of the saucer.
- Food temperature 30-35 degrees. You should not eat cold or too hot food.
- The amount of salt in the diet is reduced to a minimum or it is abandoned.
- A prerequisite for nutrition in the acute stage is a mechanically gentle consistency of food - dishes must be ground.
- Fruits and berries, completely ripe, with soft skin or peeled, are allowed in small quantities.
- Concentrated sweet juices are diluted with water.
Source: https://1001salad.com/chto-takoe-remissija-pri-jazve-zheludka/
Classification of disorders of the physiological functions of the gastroduodenal system
When compiling the classification, functional disorders affecting the motility and secretory activity of organs are taken into account.
- Perforation - perforation - a through breach of the wall in the area of damage to the stomach or duodenum. Gastric juice and food debris drain from the stomach into the free abdominal cavity or retroperitoneal space. A dangerous exacerbation occurs, during the development of which the clock counts. If assistance is not provided in time, peritonitis and an abdominal abscess develop.
- Penetration is the process of gradual germination of a defect into neighboring organs or tissues, into the liver, pancreas, into the wall of the colon or sigmoid colon.
- Stenosis of the pyloric stomach or one of the sections of the duodenum. It becomes a consequence of healed extensive erosion. According to clinical forms, stenosis is divided into compensated, subcompensated, and decompensated forms. In the compensated form, the motor and evacuation functions of the intestine are not affected. In the subcompensated clinical stage, there is a partial disruption of the evacuation of digested food into the small intestine. The decompensated form prevents the removal of food from the stomach, leading to the development of putrefactive processes inside. Surgery is required.
Degeneration into a malignant tumor - Malignancy is the degeneration of an ulcerated area into a malignant neoplasm.
- Gastric bleeding – develops when the vessels of the stomach wall are damaged by an ulcerative process. Bleeding can be acute or chronic. Based on severity, bleeding is divided into 4 stages, depending on the volume of blood lost and the state of hemodynamic parameters.
Common types of gastric ulcers are described in detail in the International Clinical Classification of Diseases, 10th revision. This classification reflects the pathogenetic, morphological and clinical types of gastric ulcer.
Treatment
The treatment is complex. Therapy should include dietary advice, medications and, if necessary, surgery.
Diet
It is important to maintain a balanced diet both during and outside of exacerbations. You should avoid overeating, eating dry or on the go, excessive consumption of carbonated drinks, and fast food. Food should be prepared using gentle methods (baking, boiling) and served at the optimal temperature (20-40 °C).
| Recommended Products | Not Recommended Products |
|
|
The presence of frequent diarrhea implies an increase in daily calorie intake and the amount of fluid consumed. This will avoid dehydration and sudden weight loss.
Drugs
Medications that can be used include:
- Antibiotics. Designed to fight infection (penicillins, cephalosporins, fluoroquinolones).
- Antisecretory, antacid drugs. Reduce acidity, protect the walls of the gastrointestinal tract (omeprazole, rabeprazole, Maalox, Almagel).
- Corticosteroids. They have anti-inflammatory activity and inhibit autoimmune processes (Prednisolone, Budesonide).
- Aminosalicylates/cytostatics. Prevents the progression of autoimmune inflammation in the intestines (Sulfasalazine/Methotrexate).
Be sure to read:
Helic test for the detection of Helicobacter pylori: preparation, implementation and interpretation
In addition, symptomatic therapy is prescribed: painkillers, vitamins.
Surgery
Surgical interventions are indicated in case of steady progression of the disease, development of complications, and ineffectiveness of drug therapy. Statistics indicate a high relapse rate (up to 45%) 3-5-7 years after the intervention. Surgeries for duodenal ulcers are most effective.
Types of operations
- Necrectomy. Excision of ulcerative defects.
- Vessel ligation. Used to stop bleeding.
- Bowel resection with/without anastomosis. Removal of the most altered segment of the intestine with or without the formation of an anastomosis with another part of the gastrointestinal tract.
Recovery period
In most cases, the recovery period takes from 2-4 weeks to several months, which depends on the degree of intestinal damage and the timeliness of therapy. In some cases, remission is achieved for years or the disease leads to disability.
Atypical and symptomatic ulcers
In addition to the main groups, the classification of peptic ulcer disease includes acute defects caused by exposure to chemical factors (for example, steroid hormones, non-steroidal anti-inflammatory drugs, thyroid hormones).
Atypical forms occur with a non-standard pain syndrome or without it at all, but show other clinical symptoms.
Processes caused by the influence of stress factors are not classified as peptic ulcers, but are considered symptoms of other acute or chronic diseases. The manifestations scar when the unfavorable factor is eliminated, and are not prone to recurrence unless the impact of the aggressive factor is repeated.
- With widespread thermal burns of the skin, a pathology called Curling's ulcer is observed.
- The consequence of severe open or closed craniocerebral injuries, neurosurgical operations, and strokes is Cushing's ulcer.
- Ulcerative processes in the stomach are sometimes caused by the development of acute myocardial infarction, a septic condition, or the consequences of severe injuries.
- Drug-induced lesions can develop under the influence of a number of medications.
- Endocrine lesions occur when the body's hormonal functions are disrupted.
It is possible to develop acute or chronic ulcerative processes that accompany the long course of a number of chronic pathological conditions affecting other organs.
- Nonspecific diseases affecting the respiratory system and lung tissue.
- Vascular diseases - atherosclerosis of organ vessels, hypertension, rheumatic lesions.
- Defects of the stomach and small intestine are hepatogenic in nature and are observed with liver damage.
- The same clinical picture accompanies the development of pancreatic pathology.
- Acute bleeding ulcers often accompany chronic renal failure, a serious disease.
Defects in the gastric mucosa are complicated by rheumatoid arthritis, a systemic disease of the joints and connective tissue.
Causes of the disease
If we talk about the reasons for the development of peptic ulcers, modern medicine classifies poor diet and stress as contributing factors. “Yes, there is a peptic ulcer induced by stress or long-term use of anti-inflammatory drugs. In particular, aspirin. But the main etiological factor is infection with the bacterium Helicobacter pylori,” says Andrey Naletov.
This infection is diagnosed in 90-95% of patients with peptic ulcer disease. In general, up to 80% of the population of the CIS countries are carriers of Helicobacter. Interestingly, in European and North American countries only about 10-15% of the population is infected. This is probably due to a higher standard of living, mentality and hygiene habits.