Who needs surgery?
Indications for stomach removal:
- Malignant tumor;
- Diffuse polyposis;
- Chronic ulcer with bleeding;
- Perforation of the organ wall;
- Extreme obesity.
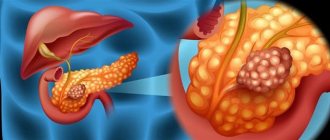
The main reason for resorting to stomach removal is malignant tumors. Stomach cancer is one of the most common types of neoplasms affecting humans, most common in Japan and Asia, but its incidence continues to rise in other regions. The presence of a tumor, especially in the middle third, cardiac or pyloric region, is considered a direct indication for gastrectomy, which is supplemented by removal of lymph nodes and other formations of the abdominal cavity.
Much less often, doctors perform surgery to remove the stomach for other reasons. For example, gastric ulcers are usually treated conservatively by gastroenterologists, but complications such as perforation or persistent massive bleeding may require radical surgery.
Diffuse polyposis, when polyps are multiple and scattered over the entire area of the gastric mucosa, is also an indication for gastrectomy, because it is not possible to remove every polyp, and their presence is fraught with malignant transformation. Perforation of the stomach wall, not only of ulcerative origin, but also due to trauma, requires emergency intervention, which may result in gastrectomy.
A special group of patients consists of overweight people, when the only way to limit the amount of food eaten is to remove the fundus and body of the stomach.
In very rare cases, gastrectomy can be prophylactic, in particular, if you are a carrier of the CDH1 gene, in which a mutation has occurred that predetermines the hereditary form of diffuse gastric cancer. For such individuals, the doctor may recommend preventive removal of the organ while cancer has not yet formed.
Considering the large volume of intervention, possible blood loss during surgery, and prolonged anesthesia, there are also contraindications to this type of surgical treatment:
- Cancer with metastases to internal organs and lymph nodes (inoperable tumor);
- Severe general condition of the patient;
- Decompensated pathology of the cardiovascular system, lungs and other organs;
- Bleeding disorders (hemophilia, severe thrombocytopenia).
Contraindications to gastric removal
Removing a vital organ is an operation that carries high risks.
Prolonged anesthesia and extensive surgical trauma can lead to death.
Therefore, the intervention has strict contraindications:
- inoperable oncology – metastases penetrating the lymphatic system or neighboring organs;
- ascites – accumulation of fluid in the abdominal cavity;
- unsatisfactory general condition of the patient - the body cannot cope with the load during surgery or during the rehabilitation period;
- pathologies in the stage of decompensation;
- cachexia in cancer;
- diseases of the hematopoietic apparatus - blood clotting disorders.
If no contraindications are identified, the operation is performed without taking into account the patient’s age.
Preparing for gastrectomy
Such a complex operation as gastric removal requires careful preoperative examination of the patient and treatment of concomitant diseases.
Before the planned operation you will need:
- General and biochemical blood tests;
- Analysis of urine;
- Examination of feces for occult blood;
- Fluorography or chest x-ray;
- Ultrasound examination of the abdominal organs;
- CT, MRI of the affected area;
- Fibrogastroscopy to examine the inner lining of the stomach, determine the nature of tumor growth, etc., which is usually supplemented by a biopsy.
Before the operation, if it is carried out as planned, you will have to undergo consultations with a number of specialists, starting with a therapist. In the presence of heart and vascular diseases (hypertension, coronary artery disease), diabetes mellitus, chronic bronchopulmonary pathology, their treatment must be adjusted so that the patient can safely undergo anesthesia and the operation itself.
Patients taking any medications should notify their doctor, and a week before gastrectomy they should stop taking blood thinners, antithrombotics (anticoagulants), non-steroidal anti-inflammatory drugs, and aspirin. If there is a high risk of infectious complications, antibiotics are prescribed in the preoperative period.
Diet and lifestyle should also be reviewed. Patients preparing for complete removal of the stomach need a gentle diet that excludes spicy, salty, fried foods, and alcohol. Smokers should think about how to quit the addiction, which increases the risk of dangerous postoperative complications.
When all the necessary examinations have been completed, the patient’s condition is stable and does not interfere with the operation, he is admitted to the hospital. The day before gastrectomy, the diet should be especially light, and from midnight it is forbidden to consume food and water, not only because of possible fullness of the stomach, but also due to possible vomiting during anesthesia.
Diet after gastrectomy
A balanced menu after gastric removal is an important component of treatment. If you follow the diet and the recommendations of your doctor, digestion is restored faster, eliminating discomfort when eating. A dietitian will help you organize your meals properly. He will help you create a diet and organize nutrition so that the body receives all the necessary substances for a speedy recovery.
What can patients without a stomach eat or those who have had part of their stomach cut off? 9-12 days after surgery, the patient is transferred to dietary table No. 1, but the pureed option is chosen. The patient should eat frequently, eating about 5 or 6 times a day. Portions should be small, about 250 g; if it is liquid, then no more than one glass.
The diet should contain a lot of proteins, so patients need to eat chopped meat or boiled fish, prepare omelettes from proteins, and do not give up fresh cottage cheese. Fats are also necessary, but in moderation.
A balanced menu after gastric removal is an important component of treatment
If the patient feels bad from such food, the amount of fat is reduced. The patient should eat little carbohydrates, especially if they are easily digestible, it is better to reduce their content. During this period, the patient should not eat strong broths, as well as fatty poultry, meat, all kinds of sausages, ham, smoked products and canned food. All fried foods, bread, flour products, and pickles are also prohibited. All vegetables and fruits must be ground before consumption.
An example of a diet after gastrectomy, which can be regulated by the attending physician:
- from 1 to 3 days:
the patient does not eat anything, drinks plenty of water; - from 3 to 7 days:
the patient can be given liquid dishes (soups and broths) prepared with lean products. After a week after the operation, the pain begins to gradually subside, but the diet does not change yet; - starting from day 14:
the patient can independently eat chopped foods (vegetables, chicken fillet, etc.); - after another week has passed:
namely, on day 20, you can eat boiled porridge, well-cooked chicken fillet, or steamed fish and vegetables (this way they become as soft as possible);
Next comes the gradual formation of a daily diet, which is prescribed and monitored by the attending gastroenterologist together with a nutritionist.
Sources:
- https://medportal.ru/clinics/services/1120/
- https://spb.krasotaimedicina.ru/treatment/gastroduodenal-resection/total-gastrectomy
- https://www.dobrobut.com/library/c-osnovnye-pokazania-dla-prodolnoj-rezekcii-zeludka-i-gastrektomii
- https://www.mskcc.org/ru/cancer-care/patient-education/eating-after-your-gastrectomy
- https://prioritetmed.ru/bolezni-zhkt/dieta-pri-udalenii-zheludka.html
Types of gastric removal operations
Gastrectomy usually involves the complete removal of the stomach, but it is also possible to leave small parts of the organ. Removal of the stomach includes several types of operations:
- Distal subtotal gastrectomy, when most of the stomach is removed, passing into the intestines.
- Proximal subtotal gastrectomy, used for tumors of the upper third of the organ, when the proximal fragment of the stomach with the lesser curvature, both omentums, and the lymphatic system must be removed.
- Total gastrectomy - the entire stomach is removed and the esophagus is connected to the small intestine.
- Sleeve gastrectomy.
Procedure for removing the stomach
During the operation, the patient is under general anesthesia. After the patient is given endotracheal anesthesia and muscle relaxants, the doctor treats the surgical field at the sites of future incisions with antiseptic agents.
Main stages of the operation
- The formation of the incision is transabdominal, transthoracic or thoracoabdominal.
- Examination of the abdominal organs with determination of the localization of pathology and tissue condition.
- Mobilization of the body of the stomach - dissection of ligaments, omentums, cutting and suturing of the small intestine, dissection of the gastro-pancreatic ligament with intersection and ligation of damaged vessels.
- Restoration by connecting the esophagus and small intestine by combining the two ends or the end of the esophagus with the lateral surface of the kink.
Progress of oncology surgery
Stomach surgery in the presence of a cancerous tumor involves removing the stomach completely.
If a malignant neoplasm has metastasized, some adjacent structures must also be removed.
The patient is given a catheter to remove urine and a probe.
At the first stage, the surgeon makes an incision in the anterior wall of the abdominal cavity. He then expands the approach depending on the location of the tumor.
If the formation affects the middle or upper lobe of an organ with or without the esophagus, the incision is moved to the left side and at the same time the diaphragm is cut.
During the operation, the surgeon removes the stomach, omentum, fatty tissue, gastric ligaments and lymph nodes in a single block. The volume of structures removed depends on the degree of damage by cancer cells.
If necessary, the pancreas, part of the esophagus, liver and spleen can be removed.
Surgery for ulcers and non-cancer lesions
In case of chronic ulcers and other pathologies of the stomach, for example diffuse polyposis, etc., removal of the omentum, lymphatic system and organs connected to the stomach is not carried out.
The doctor tries to choose a less traumatic method of gastrectomy, limiting himself to resection or subtotal surgery.
Sleeve gastrectomy
Sleeve gastric ablation
To control the amount of food consumed, obese patients are prescribed a sleeve gastrectomy.
The doctor removes only part of the stomach, which includes the body and fundus. The canal, limited in area along the line of the lesser curvature of the organ, remains intact.
Main stages of gastrectomy
Introducing the patient into anesthesia (endotracheal plus muscle relaxants).
- Opening the abdominal cavity transabdominally (through the anterior abdominal wall), transthoracically (through the pleural cavity), thoracoabdominally (a combination of both approaches).
- Examination of the abdominal cavity.
- Mobilization of the stomach.
- The connection between the esophagus and intestines.
Mobilization of the stomach is a very important part of the operation, in which the surgeon provides access to the organ by cutting the ligaments, omentum, cutting and suturing the small intestine. Crossing the gastropancreatic ligament simultaneously with the vessels located there is the most significant stage, requiring extreme caution and attentiveness. As the ligament is dissected, the surgeon also ligates the vessels.
Gastrectomy is completed by making a connection between the esophagus and the small intestine, most often in an end-to-side manner. End-to-end anastomosis is rarely performed when the esophagus or portion of the small intestine to be connected is long.
How is the operation performed?
The second name for gastrectomy is extirpation. It takes place in stages under general anesthesia. The progress of the operation is determined by the degree of development of the cancer process. A surgical incision is made and the blood vessels are ligated. Then the organ is cut off from the esophagus and intestines in the area of attachment. In addition to the stomach, regional lymph nodes and omentums are removed. Then an anastomosis is formed by combining the esophagus and small intestine.
After the operation, a cytological examination of the swabs is performed. The absence of malignant cells is an indicator of a successful operation. Surgery is useless for metastases if the course of the cancer is complicated by ascites and endocrine disorders. Tuberculosis is also considered a contraindication.
In the preoperative period, the patient must adhere to a diet and daily routine in order to lose excess weight. You should stop taking acetylsalicylic acid and drugs based on it. The day before the operation you need to spend without food and cleanse the intestines with an enema.
Disability is given after complete removal of the stomach. Radical surgery is performed when conservative treatment does not help. As a result, an important link in digestion is lost, so following a diet is vital for the patient.
Progress of cancer surgery
Since the main indication for gastrectomy is a malignant tumor, most often doctors are forced to remove the entire organ and some surrounding structures at once. Surgery to remove the stomach for cancer has its own characteristics associated with the prevalence of the tumor process and damage to neighboring tissues.
A gastrectomy is performed under general anesthesia and can take up to five hours. The patient is given a urinary catheter and a nasogastric tube. In oncology, open types of operations are most appropriate; abdominal access is preferable, implying a fairly large incision in the abdominal cavity. Of course, this is more traumatic, but it gives the surgeon the opportunity to thoroughly examine the affected area and remove all affected tissue.
After opening the abdominal cavity, the doctor inspects the organs, and then proceeds with a gastrectomy, removing in a single block the stomach, both omentums, gastric ligaments, fatty tissue, and lymph nodes, according to the stage of the disease. If the tumor has spread significantly, resection of the pancreas, part of the esophagus, liver, and spleen may also be required.
The final stage of total gastrectomy for cancer is the reunification of the small intestine with the esophagus. All stages of the operation are carried out with strict adherence to the principles of ablastics to prevent the spread of cancer cells (early ligation of blood vessels, change of linen and gloves, etc.). The oncologist surgeon must be very careful, because even the most modern diagnostic methods do not always provide accurate information about the spread of the tumor, and upon direct examination, the doctor may detect additional foci of cancer that require expansion of the operation.
In some cases of oncological pathology, laparoscopic access is possible, when the stomach is removed through a small incision on the abdominal wall. Laparoscopy is much less traumatic than open surgery; modern equipment allows it to be performed safely and effectively, but difficulties may arise with the removal of lymph nodes, so the possibility of such an operation is decided individually with each patient.
Gastrectomy
Gastrectomy is a surgical procedure in the gastrointestinal tract aimed at removing the stomach. Despite the fact that this operation is quite traumatic, in some cases it is the only chance to save the patient’s life.
Removal of the stomach (gastrectomy) is a technique that involves complete excision of the stomach and restoration of the continuity of the digestive tract by forming an anastomosis between the small intestine and the esophagus. Indications include gastric malignancies and Zollinger-Ellison syndrome.
In case of local processes, the organ is completely removed while other structures are preserved. For common cancer tumors, the scope of the operation is expanded to a combined gastrectomy, which may include removal of the spleen, resection of the liver, pancreas, lower third of the esophagus, colon or diaphragm.
Gastrectomy is a surgical intervention in the gastrointestinal tract aimed at removing the stomach
The intervention is performed using laparoscopic, open or combined access.
Types of gastrectomy:
- partial gastrectomy: removal of part of an organ. The procedure is indicated for people with a tumor located in the lower part of the stomach;
- total gastrectomy: complete removal of an organ. Doctors perform the procedure if the malignant process is localized in the upper part of the stomach or has spread throughout the organ .
The operation to remove the stomach is performed under general anesthesia. The average duration is from two to five hours. During the procedure, a urinary catheter is inserted into the patient. This operation is considered particularly traumatic with a high risk of complications. Pain after removal of the stomach usually goes away within a month.
After gastrectomy
On the first day, eating and drinking is strictly prohibited. After two days, the patient is offered a small amount of water and liquid food. If everything went well and the intestines began to function, the diet is gradually expanded. Liquid soups, porridge and pureed dishes are recommended. You can eat small portions 6-8 times a day. To regulate intestinal function, prunes, boiled beets and fermented milk products are recommended. Rehabilitation after gastric removal should be given special attention.
Gastrectomy for ulcers and other non-neoplastic lesions
In case of chronic peptic ulcer disease that cannot be treated with conservative methods, or in case of its complications, gastrectomy is also performed, trying to limit oneself to subtotal versions of the operation or removal of part of the stomach (resection). In addition, in case of non-oncological processes (diffuse polyposis, Zollinger-Ellison syndrome), there is no need to remove omentums, lymph nodes and areas of other organs, so the intervention is generally more gentle and less traumatic for the patient.
If the operation is performed as an emergency due to massive bleeding, then there is simply no time for examination, so the surgeon has to determine the required volume of intervention directly during the operation.
Resection methods
The surgical technique largely depends on the reason for the intervention and the location of the pathological focus. The course of surgery for peptic ulcer disease is especially unpredictable - the erosive process can affect various parts of the internal walls, so the surgeon is forced to literally “cut out” a new organ from the stomach tissue.
Types of surgery can be divided according to the position and volume of tissue removed. There are:
- proximal resection - with removal of the upper inlet part of the stomach;
- distal - with a reduction in the output part of the organ;
- median – the main part of the body of the stomach is cut out, preserving the inlet and outlet zones;
- partial - the operation affects a small area with the affected area.
Depending on the volume of intervention, resection can be:
- economical - with removal of 1/3 or 1/2 of the stomach;
- extensive - with cutting out 2/3 of all organ tissues;
- subtotal – almost complete removal with preservation of 1/5 of the part.
On a note! Total resection with the removal of more than 90% of the organ body is called gastrectomy. In this case, the digestive tube is restored by a direct anastomosis of the duodenum with the esophagus.
Operation techniques:
- Billroth-1 is a simple option when the connection after cutting out the fabrics occurs “joint to joint.” This preserves the sequence of arrangement of organs in the gastrointestinal tract, but the technique is difficult to perform. Rarely used.
- Billroth-2 is a more radical solution, when the segments are connected not directly, but in the most comfortable position for the body according to the “side to side” principle, without excessive tension on the seams.
The second option is more preferable for stomach cancer with a high risk of metastasis. This is what surgeons choose most often.
Sleeve gastrectomy
A special type of surgery to remove the stomach is the so-called sleeve gastrectomy, which is indicated for patients with severe obesity.
To reduce the amount of food that the patient can eat, the surgeon removes the body and fundus of the stomach, leaving only a narrow canal at the lesser curvature of the organ. When eating even a small amount of food, the remaining fragment of the stomach quickly fills, and a feeling of fullness sets in, and the patient stops eating. Sleeve gastrectomy is widely practiced all over the world and shows good results. Persistent weight loss is observed in most patients, but further dietary restrictions cannot be avoided.
Complications of gastrectomy and possible consequences
Removal of an entire organ, in this case the stomach, cannot go unnoticed by the patient. The risk of complications is quite high, and the consequences are not limited to impaired digestion of food. Most likely:
- Reflux esophagitis;
- Anemia;
- Loss of body weight;
- Dumping syndrome;
- Tumor recurrence in the gastric stump;
- Bleeding and peritonitis.
Bleeding and peritonitis are acute surgical pathologies that require urgent treatment. Typically, such complications are caused by failure of the sutures placed on the vessels and intestinal walls when removing the stomach.
If the operation itself and the early postoperative period are favorable, after discharge home the patient may encounter a number of other consequences of treatment. Thus, reflux esophagitis consists of inflammation of the esophagus when intestinal contents with bile acids and enzymes are thrown into it, which is manifested by pain, heartburn, and nausea.
Dumping syndrome is caused by an inadequate amount of food consumed and is manifested by tachycardia, sweating, dizziness, and vomiting immediately after eating.
The vast majority of patients who have undergone gastrectomy, regardless of the reason for the operation, suffer from a lack of vitamins, microelements, and nutrients, which is manifested by weight loss, weakness, drowsiness, etc. Anemia is associated with a lack of factors produced by the gastric mucosa and enhancing the formation of red blood cells.
Stomach operations
Gastrostomy (gastric fistula)
- Upper-median laparotomy
(see page 125). During the inspection, the surgeon evaluates the detected changes and selects a place to place a gastrostomy. - Fistula application
. With four napkins inserted into the corners of the surgical wound, the surgeon isolates the free abdominal cavity. By this time, the sister should prepare a gastrostomy tube 30-40 cm long from soft rubber, which can be made from a thick gastric tube that has been repeatedly boiled. The surgeon places the tube along the longitudinal axis of the stomach. Above the tube, 7-8 interrupted sutures made of silk No. 4 are placed on the wall of the stomach so that a tunnel 4 cm long is formed from this wall; two or three sutures at the end of the tube are not tied. After this, a rigid clamp is applied to the second end of the tube, and the nurse delivers a scalpel to open the lumen of the stomach. First, the tip of an electric suction is inserted into the resulting hole and the contents are evacuated, and then the proximal end of the tube is inserted and fixed to the gastric wall with an interrupted catgut suture No. 6 or No. 8, stitching the rubber and the stomach. Previously placed sutures are tied. At this stage, several additional stitches may be necessary: the nurse should have needle holders loaded with silk on hand. To check the patency of the rubber tube, remove the clamp from its outer end and insert a funnel through which a small amount of isotonic sodium chloride solution is injected into the stomach, after which the clamp is applied to the tube again. - Bringing the tube out.
The gastrostomy tube is usually brought out in the area of the left rectus abdominis muscle. To do this, use the same techniques as when removing drainage through a counter-aperture (see p. 126), only the skin is not pierced with a scalpel, but pulled out in the form of a cone with a Kocher clamp and excised with a scalpel in the form of a circle.
After this, the barrier napkins are removed, and the tube is passed through the thickness of the abdominal wall using a forceps. From the inside, the anterior wall of the stomach is sutured to the peritoneum with interrupted silk sutures. After making sure that the sutures are tight, the surgeon sutures the wound of the anterior abdominal wall in layers. On the operating table, the gastrostomy tube should be closed to prevent leakage of gastric contents.
Gastrotomy (opening the lumen of the stomach)
- Upper-median laparotomy.
- Opening the lumen of the stomach. The surgeon grabs the anterior wall of the stomach with a damp gauze pad and guides it into the wound. Isolates the stomach with napkins. Two holders made of silk No. 4 are placed on the front wall of the stomach. The threads for the holders need to be 35-40 cm long. A clamp is applied to both threads of each holder. The nurse hands the surgeon a scalpel and prepares No. 2 catgut threads on an intestinal needle for puncturing and ligating the vessels of the submucosal layer. The surgeon incises the wall of the stomach in the longitudinal direction, punctures the vessels of the submucosal layer and ligates them; The ends of the catgut threads are cut off with scissors. Using the same scalpel, the surgeon opens the mucous membrane for 1.5-2 cm and throws the scalpel into the pelvis. By this time, the nurse should prepare the tip of the electric suction, which is inserted into the resulting hole. After suctioning out the stomach contents, the mucous membrane is cut along the required length with scissors. Narrow abdominal speculum may be needed to examine the stomach. The further course of the operation depends on the nature of the detected pathology. The operation is completed by applying sutures to the stomach: first, the nurse applies a long catgut thread No. 4 on a round needle to apply a continuous suture, then, after cutting off the ends of the catgut thread, short (20-25 cm) silk No. 4 threads, also on a round needle for application second row of interrupted sutures.
- Layer-by-layer suturing of the anterior abdominal wall.
Suturing of a perforated ulcer of the stomach and duodenum
- Upper-median laparotomy.
- Abdominal toilet.
Immediately after opening the abdominal cavity, the contents are evacuated with tampons, or better yet, with the help of an electric suction. After this, the nurse gives the surgeon four large tampons, which he inserts deep into the abdominal cavity around the stomach and duodenum. - Suturing the perforation hole.
The sister feeds silk No. 4 threads 25-30 cm long on a round needle; the surgeon applies 4-5 interrupted sutures in the transverse direction, sometimes placing a strand of the greater omentum under the suture line. - Repeated toilet of the abdominal cavity
. Tampons placed before suturing are removed. The surgeon carefully drains the abdominal cavity with tuffers. - Layer-by-layer suturing of the anterior abdominal wall.
Gastroenteroanastomosis
- Upper-median laparotomy.
- Preparation of a loop of small intestine for anastomosis.
a) If the small intestine is located behind the colon, this stage of the operation begins with opening the gastrocolic ligament, which requires 6-8 hemostatic clamps, scissors, and No. 4 catgut ligatures. Assistants stretch the transverse colon, and the surgeon dissects its mesentery in an avascular area with scissors. He then selects a site for anastomosis on the small intestine and marks it with silk and catgut sutures (No. 4), passing them into the mesentery of the small intestine using a pointed clamp. Both threads with clamps placed on them and a loop of the small intestine are passed through an opening in the mesentery of the transverse colon and the latter is immersed in the abdominal cavity. The surgeon positions the intestinal loop so that the silk thread (beginning) is above the anastomosis site, and the catgut thread (end) is below the anastomosis site. b) When the small intestine is located in front of the colon, the place on the small intestine is marked in the same way and the loop is brought over the colon and omentum to the anterior wall of the stomach (or to the posterior wall - after opening the gastrocolic ligament). - Anastomosis
. The first point of this stage of the operation is the application of stay sutures that limit the size of the future anastomosis. For the holders, the sister places two silk No. 4 threads 40 cm long on an intestinal needle. Then interrupted silk (No. 2) sutures are placed on the posterior lip of the anastomosis without opening the lumen of the stomach and intestines; silk threads 25-30 cm long are fed on an intestinal needle. After applying this series of sutures, the nurse gives the surgeon scissors to cut off all threads except the outermost ones, and napkins to isolate the surgical field before opening the lumen of the gastrointestinal tract. At the moment of opening the lumen, the nurse should immediately turn on the electric suction or prepare several lush tuffers. Usually, to prevent the entry of contents, the wall of the stomach at the site of the anastomosis is pressed with a soft curved gastric sponge. The intestinal lumen is also closed with one or two soft intestinal clamps. Parallel to the line of sutures, the surgeon uses a scalpel to incise the seromuscular membrane of the stomach and intestines. After this, he can either immediately open the lumen of both organs with scissors and perform hemostasis, capturing the bleeding vessels with clamps supplied by the nurse, or ligate the vessels first, before opening the lumen. In this case, the surgeon pricks the vessels visible in the submucosal layer with a round thin needle loaded with catgut or silk (at the surgeon’s discretion) thin (No. 0, No. 1) threads. Threads are pricked and tied on both sides of the intended dissection of the mucous membrane of both organs; after opening the lumen, there is no bleeding, and the surgeon proceeds in a calm atmosphere to the next stage of the operation. This stage consists of applying an internal row of sutures - a continuous catgut suture (No. 2) first on the posterior and then on the anterior wall of the anastomosis. After cutting off the ends of the hemostatic sutures with scissors, the operating nurse provides the surgeon with a catgut thread 40-50 cm long on a round intestinal needle, and the assistant with anatomical tweezers and several gauze balls for periodic drying of the suture line. At the same time, the nurse must ensure that the small balls, as they are used up, are dropped one by one into the pelvis and do not remain in the area of the surgical field. After tying a continuous thread and cutting off its ends with scissors, gloves are processed, napkins and tools are changed. The surgeon begins to apply a second row of sutures on the anterior wall of the anastomosis, for which the nurse applies silk threads No. 2, 16-20 cm long, on a round intestinal needle. After this, the clamps are removed from the stomach and intestines. - Application of enteroenteroanastomosis.
Typically, gastroenteroanastomosis is supplemented by the imposition of an anastomosis between the afferent and efferent loops of the intestine in a side-to-side manner (see “Enteroenteroanastomosis”). - Abdominal toilet
. Isolating napkins are removed from the abdominal cavity, the cavity is dried, and the nurse counts the presence of instruments and material. - Layer-by-layer suturing of the wound of the anterior abdominal wall.
Gastric resection according to Billroth II (Hofmeister-Finsterer modification)
- Upper-median laparotomy.
- Revision of the abdominal organs
. The nurse gives the surgeon a napkin to fix the stomach, and the assistant a liver speculum. Large tampons are inserted through mirrors inserted into the abdominal cavity, the mirrors are moved from under the tampons on top of them and the surrounding tissues are removed with mirrors. - Mobilization of the stomach
. The purpose of this stage of the operation is to achieve mobility of the stomach by intersecting the tissues that fix it. To separate the stomach along the greater curvature, the nurse gives the surgeon a pointed clamp, which makes two holes in the gastrocolic ligament. Then she gives the surgeon and the assistant one hemostatic clamp each to apply a ligament to the resulting strand (Fig. 89, a). In this sequence, everyone works until the nurse has 2-4 clamps left, about which she must promptly warn the surgeon. After this, ligation begins. To ligate the part of the gastrocolic ligament remaining in the body, the nurse applies strong catgut (No. 6) threads. As a rule, the ligament contains fatty tissue and the threads slide when tied, so they must be of sufficient length (25-30 cm). Silk ligatures No. 6 are applied to the part that leaves with the stomach. After releasing all the clamps, mobilization continues in the same order as before. When manipulating near the duodenum and pancreas, the surgeon may need 2-4 thin Mosquito-type clamps and strong, thin No. 2 silk ligatures 20-25 cm long. After releasing the entire greater curvature, the nurse gives a long curved clamp, with which the surgeon makes a hole in the lesser omentum and passes a gauze strip or rubber tube, prepared in advance by the sister, around the stomach. A clamp is placed on the ends of this tube or ribbon, which is passed to a second assistant to hold the stomach in an elevated position. The surgeon completes mobilization in the duodenum area. The instruments are supplied in the same sequence: a clamp for separating tissue, two clamps for clamping the resulting portion, scissors for crossing it and two ligatures of the appropriate caliber and material - in each specific case, the surgeon usually names the item he needs. - Crossing the duodenum and processing its stump
. Before crossing the duodenum, the nurse gives the surgeon 2 strong clamps, which he places on the intestine. A crush clamp (or small Payra clamp) is applied closer to the pylorus. To isolate adjacent tissues, the nurse provides two medium napkins, which the surgeon and assistant place around the circumference of the duodenum; prepares a scalpel, a stick with iodine and, at the request of the surgeon, gives him a scalpel, and the assistant - a stick with iodine. The surgeon crosses the duodenum between the clamps (Fig. 89, b), the assistant turns the stomach upward and closes the crossed surface first with the middle one, then wraps a large napkin around the clamp and, finally, fixes it all with a long silk No. 8 ligature. Without any reminders, the operating nurse must quickly provide the materials needed to cover the dirty surface. The contaminated scalpel is put aside on a special napkin: 6N will be needed to cut the stomach. After this, the surgeon begins to process the duodenal stump. In a typical case, it is necessary to apply a long thread of catgut No. 4 on a round intestinal needle. The surgeon places a continuous wrapping suture around the clamp. After applying the suture, the clamp is removed, the thread is tightened, tied and, without cutting off its ends, a second row of interrupted silk sutures No. 4 is applied on the same needle. Before applying the last sutures of the second row, the ends of the catgut thread are cut off. Sometimes the surgeon finds it necessary to apply a third row of sutures - also interrupted with silk No. 2. After suturing the duodenal lumen, wash your hands, change napkins and instruments. In technically difficult cases, the duodenal stump is sutured atypically and the nurse follows the surgeon’s instructions. In any case, she must remember that processing the duodenal stump is one of the critical moments of the operation, and carefully check the strength of the suture material and the serviceability of the instruments before submitting them to the surgeon. - Ligation of the left gastric artery.
An equally important step is the ligation of a large vessel approaching the lesser curvature of the stomach from above and the posterior left gastric artery. If the ligature slips or the hemostat malfunctions, severe arterial bleeding occurs, which is extremely difficult to stop. The nurse should be extremely attentive at this stage, have long hemostatic clamps and an electric suction ready.Rice. 89. Stages of gastric resection according to Finsterer. a-mobilization of the stomach; b — intersection of the duodenum;
Having mobilized the stomach along the lesser curvature, the surgeon incises the anterior layer of the lesser omentum with a scalpel, passes a clamp under the control of a finger through the entire thickness of the omentum and prepares to clamp the artery. At his direction, the sister applies two strong, sharply curved clamps (many people successfully use Fedorov clamps for the renal pedicle for this purpose; see page 21). The left gastric artery, together with the surrounding tissue, is crossed between the clamps. The sister immediately gives another clamp, which is applied to the visible central end of the crossed vessel. To bandage it, use a long (30-40 cm) ligature made of silk No. 6. After tying, its ends are cut off with scissors and the artery is ligated a second time under a clamp applied to the vessel. Silk No. 4 is used here. The part remaining on the stomach is ligated with silk No. 6.
- Preparing a loop of the small intestine for anastomosis with the stomach - see section “Gastroenteroanastomosis”
(section 2a). - Cutting off the stomach, treating the lesser curvature.
The surgeon applies stay sutures using two long silk No. 2 threads on a round needle. Clamps are applied to the holders. After this, a Payr's press and two strong Kocher clamps are applied to the resection line. The abdominal cavity is isolated with napkins, the stomach is cut off with a scalpel along the upper edge of Payra's pulp (Fig. 89, c) and thrown away along with the instruments and scalpel placed on it. The stump is treated with iodine and sutured from the lesser curvature under Payr's sphincter, not reaching the greater curvature at a distance equal to the width of the future anastomosis. The suture is applied with a continuous catgut thread No. 4 on a round needle. Some surgeons prefer to sew not with a curved needle on a needle holder, but with a straight needle, holding it with their fingers.Rice. 89. c - cutting off the stomach; d — application of gastroenteroanastomosis
After applying a continuous catgut suture, the ends of the tied thread are cut off, Payra's sphincter is removed and a second row of interrupted silk sutures No. 2 is applied. The threads of three to four sutures closest to the site of the future anastomosis can be used to fix the afferent loop of the intestine, so they are not cut off, but put a clamp on them.
- Gastroenteroanastomosis.
The sequence of this stage of the operation is described in paragraph 3 of the section “Gastroenteroanastomosis”. The first moment of this stage is the application of interrupted sutures made of silk No. 2 on the posterior lip of the anastomosis, without even opening the lumen of the stomach and intestines (Fig. 89, d). After applying this series of sutures, fixing the posterior wall of the gastric stump to the site of the small intestine selected for anastomosis, the nurse gives the surgeon scissors to cut off all threads except the outer ones, and a scalpel to cut off the gastric stump between the suture line and the clamp remaining on the stump from the side of the greater curvature . In parallel, the lines of applied sutures open the lumen of the small intestine. Using a round intestinal needle, a long (40-50 cm) thread of catgut No. 2 is fed to apply a continuous suture first to the posterior and then to the anterior wall of the anastomosis. To dry the suture line, the assistant is given anatomical tweezers and small balls. After tying and cutting off the ends of the catgut thread, the hands are treated, napkins and tools are changed. The surgeon begins to apply a second row of sutures on the anterior wall of the anastomosis (no. 2 silk threads 16-20 cm long). The anastomosis is completed by fixing the afferent loop of the small intestine above the anastomosis to 3-4 sutures previously placed on the stomach for the purpose of suturing the lesser curvature. The nurse hands the surgeon a needle holder with an uncharged needle; the threads, taken on a clamp, are sequentially threaded into a needle and they are used to suture the intestine to the stump of the stomach. - The final stage of the operation.
After performing the anastomosis, the surgeon fixes the stomach stump to the edges of the window in the mesentery of the transverse colon with 3-4 interrupted sutures made of silk No. 2. The nurse carefully counts the instruments and material used. All holders are cut off, the condition of the duodenal stump is checked again (abdominal speculum may be needed), the tampons are removed from the abdominal cavity, hemostasis is checked and the abdominal cavity is drained. - Suturing a wound of the anterior abdominal wall.
Gastric resection according to Billroth I
Stages 1, 2, 3 are the same.
4. Transection of the duodenum
performed in the same sequence as during resection according to Billroth II. After wrapping the crossed surface of the stomach with napkins and retracting it to the upper corner of the wound, the surgeon does not suture the duodenal stump, but leaving a clamp on it, also closes it with a napkin in order to return to this area after removing the resected part of the stomach and prepare the stump for anastomosis with the remaining part of it.
5. Ligation of the left gastric artery
- see paragraph 5 of the section “Resection of the stomach according to Billroth II”.
6. Cutting off the stomach for treatment of the lesser curvature
- see paragraph 7 of the section “Resection of the stomach according to Billroth II”.
7. Gastroduodenoanastomosis
. Under a clamp applied to the duodenum, the surgeon uses a scalpel to incise the seromuscular membrane, stitches the vessels present here with thin catgut threads on an intestinal needle, ties the threads and cuts them off with scissors. The stomach stump is prepared in a similar way. After this, the surgeon sews together the posterior walls of the stomach and duodenum with interrupted sutures using silk No. 2; the ends of the threads are cut off.
The edges of the duodenum and stomach stumps are cut off with scissors under clamps. At this stage of the operation, an electric suction may be needed. The nurse applies a long catgut thread (No. 4) on an intestinal needle to apply a continuous suture first to the posterior and then to the anterior wall of the anastomosis. The assistant uses anatomical tweezers to dry the suture line with small balls. After tying, the ends of the thread are cut off with scissors.
Change napkins, tools, wash hands.
Interrupted silk sutures are placed on the anterior wall of the anastomosis. Silk threads No. 2 should be 25-30 cm long.
8. The final stage of the operation.
Wipes and instruments are removed from the abdominal cavity, carefully counting them. Toilet the abdominal cavity.
9. Layer-by-layer suturing of the wound of the anterior abdominal wall
.
Gastric resection using staplers
Stages 1, 2, 3 are the same.
4. Transection of the duodenum
. The surgeon places the UKL-40 device on the intended line of intersection of the duodenum, fixes it by tightening the screw until the marks align, and stitches the duodenum with staples (for more details on the procedure for working with the devices, see page 173). A crushing clamp is applied above the apparatus. After isolating the surgical field with napkins, the operating nurse gives the surgeon a scalpel, with which he crosses the duodenum between the UKL-40 and the clamp. Next, the pyloric part of the stomach is treated with iodine and wrapped in napkins. The UKL-40 fixing screw is loosened and the device is removed; the duodenal lumen is sutured with one row of tantalum staples.
For Billroth II resection, one or two rows of silk sutures are placed over the staples.
During Billroth I resection, the seromuscular layer is incised below the line of staples, the vessels are ligated, and before applying the anastomosis, the stitched edge of the duodenum is cut off along with the staples.
5. Ligation of the left gastric artery.
6. Preparation of a loop of the small intestine for anastomosis with the stomach
- see paragraph 6 of the section “Resection of the stomach according to Billroth II”.
7. Cutting off the stomach, treating the lesser curvature.
To treat small curvatures, UKL-60 and UKZH-8 devices can be used.
UKL-60 device
applied from the lesser curvature side together with a crushing clamp and fixed in this position. The surgeon stitches the stomach wall with staples and cuts off the resected part below the applied device. The latch is loosened, the device is removed; the slight curvature is stitched with one row of tantalum brackets. Next, seromuscular interrupted silk sutures are applied, immersing a series of metal staples inside. Anastomosis of the gastric stump with a loop of the small intestine or duodenum is usually performed.
Apparatus UKZH-8
allows you to apply a double-row immersion suture using U-shaped tantalum staples. After mobilization of the stomach, a device with separated halves is applied to its wall from the side of the greater curvature. After checking the correct installation of the device, bring its halves together by rotating the steering wheel. After this, fixing needles are inserted into the holes of the ribs. Raising and lowering the lever of the sewing mechanism, one staple is pushed out of the staple grooves, thus applying stitches.
To insert the first row of sutures and apply a seromuscular suture, both halves of the apparatus are slightly separated. The nurse hands over the immersion machine, which the surgeon uses to immerse the first row of sutures. The second row of sutures is placed using a sewing mechanism located on the machine closer to the remaining part of the stomach. After this, the fixing needles are removed, the central screw is unscrewed, the halves of the apparatus are separated and the plunger is removed. The surgeon removes the device and hands it to the nurse.
Anastomosis of the remaining gastric stump with the small intestine or duodenum is performed in the usual way.
Stages 9 and 10
- as with conventional resection.
Gastrectomy
- Upper-median laparotomy
. - Revision of the abdominal organs.
- Mobilization of the stomach is carried out within a wider range
than resection, but the principle is the same. After crossing the portions of the omentum and ligaments that fix the stomach, on which clamps are applied, reliable ligatures are used (catgut for the remaining part in the body, silk for the part that is removed). - Crossing the duodenum
and suturing its stump can be done manually or using devices (see “Resection of the stomach”). - Mobilization of the left lobe of the liver
, intersection of the branches of the vagus nerve. The area of the cardia and the abdominal segment of the esophagus can be well examined and mobilized only after crossing the triangular hepatophrenic ligament and mobilizing the left lobe of the liver and retracting it to the right (Fig. 90). To do this, you need to submit the longest abdominal mirrors, long clamps and long scissors.Rice. 90. Dissection of the triangular ligament of the left lobe of the liver
The right trunk of the vagus nerve, passing along the posterior right edge of the esophagus, and the left trunk, passing along the anterior left edge, are divided with scissors at the edge of the diaphragmatic opening. The branches of the nerve are always accompanied by blood vessels, for ligation of which it is necessary to apply long catgut threads No. 2-3. In this case, it is convenient for the surgeon to use a special vascular fork to apply ligatures (see page 172).
- Preparation of a loop of small intestine for anastomosis
. The surgeon dissects the avascular zone in the mesentery of the transverse colon and passes the loop of small intestine selected for anastomosis high to the intersection of the esophagus. - Transection of the esophagus
. The surgeon places a soft, curved clamp on the esophagus. For this purpose, a clamp is used to hold the stump of the bronchus or cardiac auricle (Fig. 91). The use of this clamp not only prevents the leakage of esophageal contents, but also fixes the esophagus in a retracted position and assists in suturing. A Fedorov renal clamp is applied to the removed part (see page 21) and the esophagus is cut between the clamps. - Imposition of esophageal-intestinal anastomosis
. The top of the small intestinal loop is brought under the esophageal stump and the first row of interrupted silk sutures is placed on the posterior wall of the anastomosis. At the same time, the sister feeds silk No. 2 threads 40-50 cm long on a round intestinal needle. The ends of the threads are not tied until all the stitches have been placed. The second row of interrupted sutures is applied on the same needle with the same long catgut threads No. 2 (Fig. 92). The anterior wall of the anastomosis is formed in the same way as the posterior one. - Application of intercervical anastomosis
. A side-to-side anastomosis is performed between the afferent and efferent loops (see page 139). - Fixation of loops in the window of the mesentery of the transverse colon.
- Suturing a wound of the anterior abdominal wall.
Rice. 91. Soft crank clamp for esophageal stump
Rice. 92. Applying an internal row of sutures to the posterior wall of the esophageal-intestinal anastomosis
Gastrectomy using staplers
Stages 1, 2, 3 are the same.
4. Transection of the duodenum
. For this purpose, UKL-40, UKL-60 devices can be used.
Stages 5, 6 and 7 are the same.
8. Establishment of esophageal-intestinal anastomosis using the PKS apparatus.
Having removed the mushroom with the rod from the apparatus, the tubular body is inserted through the intestine by cutting it at a distance of 12-15 cm from the site of the anastomosis. In the intestinal wall at the site of the anastomosis, the surgeon makes a puncture with a scalpel through which a rod with a mushroom is inserted into the body of the apparatus. Then the fungus is introduced into the stump of the esophagus, onto which a purse-string suture is first applied. After tightening the purse-string suture around the rod, the fungus is brought closer to the apparatus body by rotating the nut so that the sutured tissues of the esophagus and intestines are located between the apparatus body and the mushroom. After removing the fuse, stapling occurs by squeezing the handles of the device until it stops. By turning the nut 1-2 turns counterclockwise, the tissues compressed between the body and the mushroom are released and the apparatus is removed from the intestine. After this, additional seromuscular interrupted silk sutures are manually applied around the entire circumference of the anastomosis. The defect in the intestinal loop, located 12-15 cm from the anastomosis, is either sutured with a double-row suture, or used to apply a side-to-side interintestinal anastomosis.
Stages 9, 10 and 11 are the same.
Lifestyle after surgery and prevention of complications
In the postoperative period, the patient may require care and assistance, consisting of the administration of painkillers, nutritional mixtures through a tube, and intravenous fluids. Until it becomes possible to eat food by mouth, special solutions are prescribed intravenously or through a tube inserted into the small intestine. Infusion therapy is performed to replenish the missing fluid.
Approximately 2-3 days after the operation, the patient is asked to drink liquid and try liquid food. If everything is fine, the intestines have begun to function, then the diet gradually expands from liquids to cereals, pureed dishes and then to eating regular food.
Nutrition after gastrectomy is of particular importance. Patients who have undergone surgery are advised to eat small meals up to 6-8 times a day to prevent the possibility of dumping syndrome and digestive disorders. Large amounts of food should be avoided.
The diet after removal of the stomach should be gentle, it is better to steam or boil dishes, preferably a sufficient amount of protein, reducing the proportion of fats and avoiding easily digestible carbohydrates (sugar, sweets, honey). After removing the stomach from the diet, you will have to eliminate spices, alcohol, spicy and fried foods, smoked foods, pickles, and reduce salt intake. Food should be well chewed, not cold, but not hot.
If intestinal function is impaired in the form of diarrhea, dishes with rice, buckwheat are recommended, and for constipation - prunes, fermented milk products, boiled beets. It is allowed to drink tea and compotes, but the amount should not exceed 200 ml at one time, and it is better to divide it into 2-3 parts.
The deficiency of vitamins and microelements that inevitably occurs after removal of the stomach is compensated for by taking them in the form of medications. Vitamin B12 must be prescribed, since in the absence of the stomach its absorption does not occur, which is fraught with the development of pernicious anemia.
You can switch to the described diet a month to a month and a half after removal of the stomach, but rehabilitation usually takes about a year. Of particular importance is the psychological status and mood of the patient. Thus, excessive anxiety and suspiciousness can lead to long-term unjustified restrictions in the diet, resulting in weight loss, anemia, and vitamin deficiency. There is another extreme: the patient cannot maintain the regime, reduces meals to three or four times a day, begins to eat prohibited types of foods, which leads to digestive disorders and the development of complications.
Good physical activity is necessary for early activation and stimulation of intestinal function. The sooner the patient gets up after surgery (within reason, of course), the lower the risk of thromboembolic complications and the faster the recovery.
With a correct and timely operation, adequate rehabilitation and compliance with all doctor’s recommendations, patients after gastrectomy live as long as everyone else. Many adapt to new digestive conditions and lead a very active lifestyle. The situation is worse in patients who have undergone surgery for cancer. If the tumor is detected in a timely manner at an early stage, then the survival rate reaches 80-90%, in other cases this percentage is much lower.
The prognosis after removal of the stomach, as well as life expectancy, depend on the reason for which the operation was performed, the general condition of the patient, and the presence or absence of complications. If the organ removal technique was not violated, complications were avoided, and there was no recurrence of the malignant tumor, then the prognosis is good, but the patient will have to make every effort so that the body receives the substances it needs in full, and the digestive system, devoid of a stomach, does not suffer from an unbalanced nutrition.
Results of the operation
As with Roux-en-Y gastric bypass, most weight loss is achieved in the first 2 years (>70% weight loss for BMI less than 50). After this, in some cases, weight restoration occurs and the residual gastric pouch expands.
Within 5 years, there was a steady weight loss of around 50% of excess weight. The best results are achieved with good adherence to dietary and behavioral recommendations.
With a proper diet, regular exercise, and good eating habits, sleeve gastrectomy patients will feel well and maintain good weight loss.
A 2021 meta-analysis compared mid- and long-term outcomes between sleeve gastrectomy and gastric bypass surgery. It was concluded that in the medium term (2-3 years after surgery), the two surgeries had similar results in terms of excess weight loss and resolution or improvement of comorbidities.
In the long term (5 years after surgery), patients after sleeve gastrectomy can partially restore their body weight after stretching the sleeve stomach.
You can get more information on the possibilities of performing a sleeve gastrectomy in Belgium by writing to us or requesting a call back. We will provide you with complete information on obesity treatment in Belgium. Just click on the call back icon and we will call you back within the day.