Pancreatic surgery includes many subcategories that are designed to improve the quality of life of patients in the gastroenterology department.
The uniqueness of the presented gland lies in the fact that it is simultaneously an organ that produces external and internal secretions. It is responsible for the production of enzymes that guarantee stable digestion. The secretion enters the intestines through the excretory ducts. The organ is also a generator of hormones that enter directly into the blood. If treatment is not provided in time, the affected gland quickly fails, affecting neighboring tissues due to its destabilization.
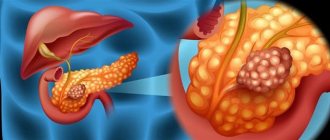
The option is especially dangerous when the victim is diagnosed with an oncological tumor, be it benign or malignant. Almost always, such a scenario requires intervention to remove the problem area.
Medical indications
Anatomically, the pancreas belongs to the upper abdominal cavity, located behind the stomach. The localization site is quite deep, which presents some difficulty during surgery.
Content:
- Medical indications
- Surgery to help patients with acute pancreatitis
- What surgery is indicated for abscesses?
- Is surgery necessary for pseudocyst?
- Features of resection
- What operations are performed for chronic pancreatitis?
- Organ transplant success
- Postoperative period
Schematically, the organ can be divided into three parts: body, tail, head. All of them are closely adjacent to adjacent organs. Thus, the duodenum goes around the head, and the posterior surface is adjacent to the right kidney with the adrenal gland. The part is in contact with the aorta, vena cava, spleen and important vascular pathways.
Due to such dense anatomical fullness, people often wonder whether partial or complete excision of an organ is performed at all. But if an experienced surgeon is responsible for the procedure, then he will cope even with such complex tasks.
The unique organ amazes not only with its extensive functionality and location. It has a rather unusual structure, which includes not only connective tissue, but also a glandular analogue. Additionally, the parenchymal component of the body has an abundant vascular network and ducts.
Doctors admit that this gland is poorly understood in terms of etiology and pathogenesis. Because of this, its cure often involves a long-term, comprehensive approach. Sometimes even with positive dynamics, negative consequences appear.
Among the most common possible complications are:
- bleeding;
- suppuration;
- relapses;
- melting of surrounding tissue;
- exit of an aggressive enzyme beyond acceptable limits.
Because of this, surgical technology is used only in exceptional cases, when it is clear that no other alternative methods will help cope with the current situation. Removing the problematic part of the abdominal cavity, or partially, will allow you to get rid of constant pain, improve your well-being and even prevent death.
Among the main medical indications, experts note:
- acute inflammatory process;
- pancreatic necrosis;
- peritonitis;
- necrotizing pancreatitis with suppuration, which is an indication for emergency excision;
- abscess;
- trauma followed by bleeding;
- neoplasms;
- cyst;
- pseudocyst.
The last variation involves pain and outflow disturbances.
Depending on the primary source of the disease, the type of operation will be determined. The modern classification includes the following varieties:
- necrectomy, which is triggered by necrosis;
- total pancreatectomy;
- abscess drainage;
- drainage of the cyst.
Separately, decisions are considered regarding the need to excise only part of the organ, which is called resection. When it is necessary to remove the head, one of the most popular types of resection is used - pancreaticoduodenal. And if lesions are detected in the area of the tail or body, distal resection cannot be avoided.
Some types of surgical treatment
If there is a pancreatic cyst, surgery involves removing the first part of the organ. As a rule, in this situation, surgical intervention is not considered one of the complex ones.
For stones in the pancreas, surgery begins with dissection of the organ tissue. The walls of the duct are also exposed to this effect. After this, the stones are removed. If there are a large number of the latter, then a longitudinal dissection of the organ is performed, followed by removal of the stones.
It also happens that pancreatic cancer is diagnosed. The operation is the most difficult. In case of tumor of the tail and body, the gland and spleen are removed. In case of a malignant neoplasm in the tail and head, the organ is removed along with the duodenum and spleen.
Surgery to help patients with acute pancreatitis
After acute pancreatitis is confirmed in the victim, doctors first try to restore their former health without surgery. But when alternative approaches do not give the desired result, then radical measures cannot be avoided.
Experts note that, despite the seriousness of the disease, there are no strict criteria for indications for the procedure for acute pancreatitis.
The main indicators of the need to involve surgery are:
- infected pancreatic necrosis, which is characterized by purulent melting of tissue;
- ineffectiveness of conservative therapy for more than two days;
- abscesses;
- purulent accumulations in peritonitis.
The necrotic course of the disease, when suppuration haunts about 70% of all victims, is considered particularly difficult even for real professionals.
Without radical solutions, the mortality rate is 100%.
When infected pancreatic necrosis is confirmed in a patient, he is urgently prescribed an open laparotomy with cleansing of dead cells and drainage of the postoperative bed.
According to statistics, about 40% of clinical cases require repeat laparotomy in the future. Even an experienced gastroenterologist is unlikely to announce the exact time period. The reason for repetition is the need to completely get rid of harmful tissues affected by necrosis.
In particularly difficult scenarios, doctors do not even suture the abdominal cavity, leaving it open so that if there is a risk of bleeding, they can quickly pack the problem area.
Many people registered in the gastroenterology department of the hospital are interested in the fact of how much such care costs. But there is no specific figure here, since it takes into account the peculiarities of each operation along with the medications involved, anesthesia and subsequent recovery. Doctors warn that if a patient has undergone surgery, this is not the end of the expenses.
There is always a risk of needing re-intervention. The price will also increase due to the need to undergo quite a long rehabilitation. Separately, the cost is affected by the need to resort to cholecystectomy. This measure is necessary if, along with the main disease, the victim is also found to have gallstone disease. Then, in one go, the surgeon will get rid of the gallbladder.
What is the essence of postoperative treatment?
Appropriate therapy is prescribed by a specialist after studying the patient’s medical history.
As a rule, after surgery, doctors advise adhering to a dietary diet, following a special gentle regimen, and eating special enzyme supplements that promote the digestion of food.
It is also mandatory to engage in physical therapy and undergo physiotherapeutic procedures.
Since after removal of the pancreas, most begin to suffer from diabetes, they are prescribed insulin.
What surgery is indicated for abscesses?
If a person has been confirmed to have an abscess, then sending him to the operating room cannot be delayed. Especially when the abscess was a direct consequence of limited necrosis after exposure to an infectious pathogen. Sometimes the provocateur of the deviation is a long-term period of suppuration of the pseudocyst.
People usually ask what can be done in such a serious situation, other than surgery, but without an autopsy with drainage, a person’s life is unlikely to be saved. Depending on the affected area, it will depend on which technology the gastroenterologist will prefer:
- open;
- laparoscopic;
- internal.
The first combination is based on laparotomy, which involves opening the abscess with drainage of its cavity until the area is completely cleared.
When a verdict is made in favor of laparoscopic drainage, a laparoscope is required, with the help of which the problem point is opened carefully. Next, the expert removes non-viable tissue and installs channels for proper drainage to function.
A difficult and at the same time productive technique is internal drainage, the difficulty of which lies in opening the abscess through intervention through the posterior wall of the stomach. For a successful outcome, laparotomy or laparoscopic access is used.
The result is presented in the form of the release of malicious content through an artificially created fistula. Over time, the cyst becomes obliterated, and the fistula opening closes.
Diet after surgery
Medical nutrition is one of the main components of the patient’s rehabilitation period.
The diet begins after two days of fasting. On the third day, the patient is allowed to eat pureed soups, teas without sugar, crackers, rice and buckwheat milk porridges, cottage cheese, a little butter and steamed protein omelet.
Before going to bed, the patient can drink a glass of water with honey or yogurt.
For the first seven days, all food for the patient should be steamed. After this period, you can eat boiled foods.
Is surgery necessary for pseudocyst?
Pseudocyst is a consequence of an acute inflammatory process in the pancreas. From a physiological point of view, a pseudocyst is a cavity that has not received a formed membrane, and inside it there is pancreatic juice.
Some people mistakenly believe that such a diagnosis is cancer, but in fact, getting rid of it is much easier than when diagnosing oncology. This even applies to situations where impressive accumulations of up to 5 centimeters in diameter are discovered.
If you do not help the patient at this stage, he will soon face numerous complications, which are expressed in:
- compression of surrounding tissues or ducts;
- chronic pain;
- suppuration up to the formation of an abscess;
- vascular erosions with bleeding due to exposure to aggressive digestive enzymes;
- breakthrough of accumulations into the abdominal cavity.
Such sad scenarios are confirmed by numerous reviews from those who have already gone through such a difficult test. To alleviate their condition, they were prescribed:
- percutaneous external drainage;
- excision of pseudocyst;
- internal drainage, which is based on creating an anastomosis of the cyst with the stomach or a loop of the cyst.
One of the options presented above is selected solely on the basis of analysis results.
Rehabilitation period
Is it possible to leave the hospital immediately after surgery? No. The patient is continuously monitored for several days. The blood composition is monitored, sugar tests are taken, blood pressure is regularly measured, and a chest x-ray is performed.
Many complications that arise after surgery may take some time to appear. Depending on the patient’s condition on the first day after surgery, a prognosis for the future is made.
On the forum you can find information that discharge from the hospital occurs 1-1.5 months after the operation. In the first week after surgery, the patient must remain in bed.
Rehabilitation includes mandatory adherence to a diet. Nutrition after pancreatic surgery begins with the first 2 days of fasting, after which food is allowed on the 3rd day. In the first week, food is cooked exclusively by steaming. The menu for the first days consists of the following products: unsweetened tea, crackers, cottage cheese, porridge with milk, steamed egg white omelet.
The diet after pancreatic surgery gradually expands. In the evening you can eat yogurt. Boiled products are allowed 10 days after the operation. Nutrition during the rehabilitation period excludes fried and fatty foods, smoked foods, flour products, sweets and baked goods.
In the future, the patient will only occasionally be able to indulge in prohibited foods.
A mandatory item in the recovery program is physical therapy. You need to return to active life gradually. Exercise therapy after pancreatic surgery consists of breathing exercises and cardio exercises. Gymnastics must be performed strictly under the supervision of a doctor.
Important information: Which doctor should I consult for pain in the pancreas?
According to medical statistics, neglecting the need to perform physical therapy exercises significantly delays the patient’s rehabilitation process and increases the risk of relapse after surgery for an oncological tumor.
Reviews about the operation
Patients after surgery say:
- Igor, Moscow: I was diagnosed with pancreatitis, I was treated with pills for a long time, but it didn’t really help. It’s my own fault: I didn’t really follow a diet. As a result, I had to undergo surgery. Everything went well. It was difficult to follow a strict diet. But after the intervention I began to feel much better.
- Elena, Ivanovo: They found a tumor on the pancreas, they had surgery to remove it, it’s good that the organ was not removed. After the operation there was severe pain, they said that this was a common complication, and they treated it with medications. Now it’s all gone, I’m on a diet, and I’m regularly checked by a doctor.
- Vadim, 60 years old: After pancreatic surgery, I didn’t do any exercises, I was lazy. In the end, I regretted it - it took a very long time to recover. Thanks to the doctors for improving my condition with pills. I can tell everyone who will undergo such an operation: diet and breathing exercises are mandatory, otherwise there may be a relapse.
Feedback from patients who have undergone pancreatic surgery boils down to one thing: recovery and future well-being depend on how accurately a person follows the doctor’s instructions, performs exercises and adheres to a diet.
The operation to remove the pancreas is a very complex surgical procedure that requires strict adherence to the recommendations of specialists during the rehabilitation period.
Features of resection
Removal of a part of an organ is prescribed only when health cannot be saved in any other way. This usually occurs due to damage by a neoplasm, or after a recent injury, when the overall prognosis remains consistently positive. Very rarely, radical excision is resorted to if a person has become a victim of chronic pancreatitis.
Due to some anatomical distinctive features of the blood supply to the gland, only one of two parts can be removed:
- head;
- body with tail.
But the first solution involves mandatory excision of the duodenum, since the system has a single blood supply.
To reduce the percentage of risks of surgery on the pancreas, doctors have developed several versions of resection. The most popular is the pancreaticoduodenal variation, which is also called the Whipple method. The technology relies on extracting not only the affected head of the gland along with the circumflex organ of the duodenum, but also part of the stomach, gallbladder and neighboring lymph nodes.
Such extensive intervention is indicated for cancer of the papilla of Vater or a tumor located in the specified area. But the matter does not end with the excision, because the surgeon is obliged to build a drain for the bile. The remaining gland tissue is used for reconstruction. Outwardly, it will look as if the specialist has re-formed the damaged parts of the digestive tract from what remains in the abdominal cavity.
The recovery program includes several anastomoses at once:
- gastric outlet with jejunum;
- pancreatic stump duct with intestinal loop;
- common bile duct with the intestine.
Occasionally, based on the prevailing situation at the time of the operation, surgeons give preference to pancreatogastroanastomosis. It is based on the release of the pancreatic duct into the stomach, and not, as usual, into the intestines.
Distal variation is necessary to free the tumor, which is located in the body or tail. It is believed that this is a more severe case when it comes to malignant oncological formations. They are almost always inoperable because they grow into the intestinal vascular system too quickly. Because of this, surgeons are more likely to make such a radical decision if the benign nature of the tumor has been confirmed.
Adding to the difficulty is the fact that the distal analog necessarily covers the need to remove the spleen. Such a complex system is explained by the fact that the technique is associated with the spread of diabetes mellitus at the postoperative stage.
Sometimes plans have to be changed on the spot. When the abdominal cavity is opened, the doctor may notice a more extensive spread of the pathology, which will prompt him to use a last resort - a total pancreatectomy. This means that complete excision of the organ is planned to preserve health.
In what cases is pancreatic resection prescribed?
Pancreas
Before prescribing surgical treatment for various diseases of the pancreas, all possible methods that do not require surgical intervention are used. If a cancerous tumor is suspected, the presence of which can be confirmed after a thorough diagnosis of the pancreas (after a biopsy of the pancreas is done and appropriate tests are taken from the patient), pancreatectomy is prescribed. Partial resection of this organ may be prescribed in the following cases:
- phases of exacerbation of chronic pancreatitis
- mechanical damage to the organ and destruction of its integrity (ruptures, crushing)
- the presence of neoplasms of a malignant nature (carcinoma)
- cyst formation
- presence of fistulas
- necrotic changes in tissues
What operations are performed for chronic pancreatitis?
Some patients believe that with diabetes mellitus, along with the concomitant destabilization of the gland due to chronic pancreatitis, only surgery will help. But experts warn that with such a pancreatic condition, one can only hope for relief, and not for a complete recovery without the risk of relapse.
To help victims of the chronic form of such a dangerous disease, doctors have developed several surgical practices:
- drainage of ducts, which is necessary in case of pronounced problematic patency;
- resection with drainage of the cyst;
- resection of the head, which is characteristic of obstructive jaundice, duodenal stenosis;
- pancreatectomy for large-scale lesions.
The stones that are deposited in the ducts deserve special attention. They partially or completely block the passage of secretions, which provokes acute pain. In case of severe pain and the impossibility of reducing its manifestations with the help of pharmacological substances, there is no other option other than classical surgery.
This technique is called virsungotomy. This means cutting the duct to remove the stone, or draining above the level of obstruction.
Indications for surgery
Surgeries on the pancreas are performed according to strict indications, which are determined individually for each patient:
- pancreatitis, turning into pancreatic necrosis;
- abscess or phlegmon of an organ;
- the formation of stones blocking the lumen of the ducts;
- purulent pancreatitis with the development of peritonitis;
- massive injury with unstoppable bleeding;
- malignant tumor;
- multiple cysts causing persistent pain.
These conditions are considered absolute indications for surgical intervention - planned or emergency. Whether surgery is performed for other diseases of the pancreas depends on the characteristics of the pathology and the patient’s health status.
pancreatic cancer
Organ transplant success
A relatively new word in surgery for pancreatic health is transplantation. It was first produced in 1967. But even then, scientists knew that it would be possible to change organs only together with the accompanying duodenum.
Despite the fact that after a kind of exchange it is possible to live with other internal organs for quite a long time, how long they live after such a transplant is not particularly encouraging. In official medicine, the longest life expectancy after a successful outcome was just over three years.
Due to the too high risks for the patient, as well as the high threshold of complexity, this transplant is not in significant demand, even if the victim has been diagnosed with a malignant tumor.
The difficulty ends with the fact that the gland is a hypersensitive component of the abdominal cavity. Even with a gentle touch with a finger, she receives significant injuries. If we add to this the need to suture a huge number of accompanying large and small vessels, then the manipulation turns into a many-hour ordeal for all medical personnel and the patient.
The search for a donor is also not particularly smooth, since this organ is classified as unpaired, which means it can only be taken from a deceased person. He must not only meet all the criteria, but also give prior permission for the use of his organs for those in need.
But even if you manage to get such a donor, the required part of the peritoneum must be delivered extremely quickly. The gland is sensitive to a lack of oxygen, and also begins irreversible processes half an hour after the cessation of stable blood flow.
This means that even after careful removal from the previous owner in freezing mode, it will survive no more than five hours. This is unlikely to be enough to organize transportation even between neighboring transplant centers, and if you add time for the procedure itself, it becomes completely difficult.
If the victim was lucky and the organ was delivered as soon as possible, then the algorithm for identifying it includes:
- placement in the peritoneum;
- connection with hepatic vessels;
- comparison with the splenic and iliac vessels.
This is difficult to implement from the technical side of the issue, and is also accompanied by a high chance of death due to extensive bleeding and subsequent shock.
Introduction
Chronic pancreatitis (CP) is a disease whose treatment is challenging. The inflammatory-degenerative process in the pancreas (P) usually occurs with alternating exacerbations accompanied by destruction of gland tissue and periods of replacement of damaged parenchyma of the organ with connective tissue [1]. Chronic recurrent inflammation of the pancreas leads to a number of complications requiring surgical treatment. Resection of the head of the pancreas with the formation of a longitudinal pancreatojejunostomy (Frey's operation) is one of the most common surgical options. In this report, we described the technique of performing the operation, which is accepted at the Institute of Surgery named after. A.V. Vishnevsky.
Material and methods
Description of the original method
In 1987, C. Frey and G. Smith proposed a new method of surgical treatment of CP [7]. This surgical intervention, which is commonly called the Frey operation, consists of resection of the head of the pancreas with preservation of the duodenum (duodenum) and longitudinal pancreaticojejunostomy along the body and tail of the gland with the jejunal loop turned off by Roux (Fig. 1).
Figure 1. Scheme of surgical treatment of chronic pancreatitis proposed by C. Frey and G. Smith in 1987 [7]. a — volume of resection of the head of the pancreas.
Figure 1. Scheme of surgical treatment of chronic pancreatitis proposed by C. Frey and G. Smith in 1987 [7]. b — reconstructive stage of the operation. Unlike Beger's operation, complete transection of the pancreas in the isthmus region is not performed.
Laparotomy is performed using a bisubcostal approach. After mobilization of the duodenum according to Kocher, the gastrocolic ligament is dissected, and the anterior surface of the pancreas becomes accessible for inspection. The main pancreatic duct (MPD) is opened longitudinally along its entire length, and stones are removed and strictures are dissected. The portal and superior mesenteric veins are distinguished above and below the isthmus of the gland. According to the authors, this technique avoids complete transection of the gland and prevents damage to these vessels. Preventive hemostatic sutures are applied to the tissue of the head of the pancreas using an absorbable thread, parallel and at a distance of 3-4 mm from the edge of the duodenum. Using an electrocoagulator, the tissue of the head of the pancreas is resected, leaving a layer of parenchyma along the inner edge of the duodenum, which contains branches of the upper and lower pancreaticoduodenal arteries, providing blood supply to the intestine. The authors recommended preserving the anterior pancreaticoduodenal arcade and avoiding injury to the intrapancreatic portion of the common bile duct. To better identify the common bile duct, it is proposed to mark it with a metal bougie, after which the anterior surface of the duct is freed from fibrous tissue. Medially, to the right of the portal vein, a 4-5 mm wide section of the parenchyma of the gland is preserved to avoid injury to the confluence of the portal vein and the intersection of the isthmus. The authors proposed to create a longitudinal pancreatoenteroanastomosis with a dissected gastrointestinal tract and a resected head of the pancreas using a double-row suture. The inner row of individual sutures is applied with PDS 3/0 thread (Polydioxanone, PDS - trade name), the outer row with 3/0 silk. A similar option for creating a longitudinal pancreatojejunostomy was proposed by P. Partington and R. Rochelle back in the 60s of the last century [13].
In 2003, C. Frey and K. Mayer [6] reported modifications to the surgical technique. The authors refused to isolate the portal vein above the pancreas. At the same time, mobilization of the superior mesenteric vein along the lower edge of the gland was still recommended “... to provide an idea of the location of the vessels behind the isthmus of the pancreas.” To achieve hemostasis, the gastroepiploic artery is ligated at its origin. Particular attention is paid to the adequacy of drainage of the ducts of the uncinate process of the head of the pancreas. The authors do not describe changes in the technique of forming pancreaticoenteroanastomosis, but note that it is possible that the duodenal wall is also involved in the sutures of the anastomosis when there is a thin layer of parenchyma of the head of the pancreas.
Indications and contraindications for Frey's operation
Frey's operation is indicated for patients with CP with persistent pain syndrome against the background of pancreatic hypertension caused by stones, strictures of the gastrointestinal tract and/or postnecrotic cysts of the gland (Fig. 2)
Figure 2. Results of instrumental examination of patients with chronic calculous pancreatitis for whom Frey's operation is indicated. a — SCT of the abdominal organs. Delayed phase. Enlarged fibrous-changed head of the pancreas (arrow).
Figure 2. Results of instrumental examination of patients with chronic calculous pancreatitis for whom Frey's operation is indicated. b — SCT of the abdominal organs. Delayed phase. Enlarged fibrous-changed head of the pancreas, cyst of the head of the pancreas (arrow).
Figure 2. Results of instrumental examination of patients with chronic calculous pancreatitis for whom Frey's operation is indicated. c — SCT of the abdominal organs. Native research. Pancreatic hypertension, virsungolithiasis (arrow).
Figure 2. Results of instrumental examination of patients with chronic calculous pancreatitis for whom Frey's operation is indicated. d-ultrasound of the abdominal organs. B-mode. Cyst of the head of the pancreas, pancreatic hypertension (arrows). [4, 5, 7]. Contraindications to this operation are compression of the superior mesenteric vein with the development of regional portal hypertension, duodenal dystrophy and the inability to exclude the tumor nature of the disease [6, 10-12]. For the listed complications of CP, it is necessary to perform a subtotal resection of the head of the pancreas (Beger's operation) or pancreaticoduodenal resection with preservation of the pylorus. A relative contraindication, in our opinion, is the presence of biliary hypertension. The release of the intrapancreatic part of the common bile duct from scar tissue significantly complicates and increases the duration of the operation, requiring marking of the duct with a probe. In such observations, it is more expedient to form a single cavity, including the opened intrapancreatic part of the common bile duct and the main bile duct, anastomosed with the lumen of the jejunum - the “Bernese version” of resection of the head of the pancreas [8].
Description of the technique for performing the Frey operation used at the Institute of Surgery named after. A.V. Vishnevsky
A transverse or bisubcostal laparotomy is performed. To achieve maximum quality of surgery and ensure optimal exposure, a universal retractor with attachment to the operating table and a circular open contour (Germany) is installed. By modeling the positions of the arches for specific anatomical conditions and surgical access, it is possible to have a wide and, most importantly, absolutely stable view of the surgical field (Fig. 3, see color insert).
Figure 3. Intraoperative photographs. Stages of performing Frey's operation. a — surgical access. A universal retractor is installed. View of the wound from the operating surgeon's side.
Figure 3. Intraoperative photographs. Stages of performing Frey's operation. b — view of the wound from the assistants’ side.
Figure 3. Intraoperative photographs. Stages of performing Frey's operation. c — resection of the head of the pancreas was performed, the main pancreatic duct along its entire length was opened (arrow).
Figure 3. Intraoperative photographs. Stages of performing Frey's operation. d — stage of formation of pancreatojejunal anastomosis on a loop of the small intestine switched off according to Roux. Bottom row of stitches (arrow).
Figure 3. Intraoperative photographs. Stages of performing Frey's operation. d — stage of formation of pancreatojejunostomy on a loop of the small intestine switched off according to Roux. Top row of seams (arrow). The number of blades used is determined by the constitutional characteristics of the patient and the specific situation. Using this wound retractor allows you to eliminate the need for a second assistant.
After installing the retractor, the omental bursa is opened. To determine the location of the superior mesenteric vein, the reference point is the median vein of the transverse colon; the superior mesenteric vein is not distinguished.
The duodenum is mobilized according to Kocher. The last technique should ensure free insertion of the left hand behind the head of the pancreas. The opening of the lumen of the gland is performed in the area where it is better visualized or determined by palpation - as a rule, in the area of the body of the gland. In rare cases, when identification of the duct is difficult, we perform intraoperative ultrasound, which allows us to accurately detect and open the duct. After opening the latter for a short distance, it is dissected with an electric knife along its entire length to the tail and head of the pancreas. Next, with the left hand, inserted under the head of the pancreas and duodenum, the latter are fixed and, focusing on the fingers of the left hand, resection of the tissue of the head and uncinate process is performed. This technique allows you to confidently resect tissue without fear of “extending” beyond the resected organ. The parenchyma is excised with thin plates in a spiral from the previously opened lumen of the gastrointestinal tract to the periphery using an electric knife. The superior pancreaticoduodenal artery is often located in the resection zone, which requires its intersection and ligation. The artery stump should not subsequently enter the anastomotic suture line. Upon completion of the resection, a layer of gland tissue no more than 5 mm wide remains along the perimeter of the head and uncinate process. The bottom of the formed cavity is a thin layer of tissue, through which the fingers of the left hand, located behind the head, are clearly visible. All stones from the remaining tissue of the head and uncinate process should be removed. Since stones are often coral-shaped and tightly fixed, they are removed with excision of adjacent tissue, which reduces trauma to the pancreatic parenchyma. After resection is completed, the tip of the probe or dissector should freely pass through the major papilla of the duodenum into its lumen. In the absence of biliary hypertension, exposure of the wall of the common bile duct is not required. Final hemostasis must be extremely careful and is achieved by suturing. Urgent histological examination of the removed gland tissue is strictly necessary to exclude the tumor nature of the disease.
The jejunum is divided 20-30 cm from the ligament of Treitz at the level of the first arterial arcade. A “Ru-loop” of at least 50 cm in length is formed with the formation of an end-to-side interintestinal anastomosis using single-row continuous sutures. An isolated loop is passed behind the colon through a window into the mesocolon. The intestine is dissected along the antimesenteric edge to the mucous layer, 1 cm away from its stump. The length of the intestinal wall incision should be 5-10 mm shorter than the length of the opened gastrointestinal tract and the cavity of the resected head. The formation of pancreatojejunostomy begins from the distal angle. In the extreme distal part of the opened GPP, the gland tissue is sutured with two 3/0 polypropylene ligatures 70 cm long. The ligatures should be located 2-3 mm above each other. The lower lip of the pancreatojejunostomy is formed with a lower ligature using a wraparound suture in one row. The distance between stitches is 5-7 mm, the depth of capture of the intestinal wall and pancreatic tissue is at least 5-6 mm. Next, the intestinal lumen is finally opened. The upper lip of the anastomosis is similarly formed by a previously applied upper ligature to two-thirds of its length. The remaining part of the anastomosis is sutured with a new ligature. This method of forming the upper lip of the anastomosis allows for revision of the latter in the event of bleeding in the immediate postoperative period with minimal trauma to the pancreas tissue. At the end of the operation, the Roux-loop is sutured in the window of the mesentery of the transverse colon. A drainage tube is brought to the area of the formed anastomosis.
Results and discussion
According to the described method, from 2007 to 2010 at the Institute of Surgery named after. A.V. Vishnevsky performed 60 operations. There were 56 men (93.3%), 4 women (6.7%). The age of the patients ranged from 21 to 71 years (average 48.1±1.2 years). In all cases, the disease occurred due to alcohol abuse. The average duration of the operation was 4 hours 32 minutes ± 1 hour 39 minutes. Postoperative complications of varying severity developed in 21 (35%) patients. Only in 4 (6.7%) patients the severity of postoperative complications was assessed as “grade III - grade V” and higher according to the P. Clavien classification [3]. Bleeding into the lumen of the pancreatojejunostomy on the 3rd day after surgery occurred in 2 patients; in one observation, it was possible to limit ourselves to conservative treatment; in the other, relaparotomy was performed, disconnection of the anterior lip of the anastomosis, suturing of the bleeding vessel of the pancreas, and restoration of the anastomosis.
Postoperative pancreatitis developed in 17 (28.3%) patients; the complication corresponded to the edematous form of pancreatitis in 16 patients, and pancreatic necrosis in 1 patient. Pancreatic necrosis led to arrosive bleeding into the lumen of the anastomosis, which required relaparotomy, separation of the pancreatojejunostomy, and suturing of the bleeding vessel. Failure of anastomotic sutures with subsequent formation of pancreatic fistulas occurred in 2 cases. The fistulas closed spontaneously 2 and 3 months after surgery. The average length of hospital stay after surgery was 12±4 bed days. 1 (1.7%) patient died from multiple organ failure due to pancreatic necrosis.
Chronic pancreatitis is a serious disease that often leads to the development of complications requiring surgical treatment:
- pain in the epigastric region, refractory to drug treatment;
— suspicion of a pancreatic tumor against the background of inflammatory changes in the parenchyma;
- stenosis of the intrapancreatic part of the common bile duct with the development of biliary hypertension, obstructive jaundice;
- pancreatic hypertension caused by strictures of the main duct of the pancreas, virsungolithiasis;
— compression of the superior mesenteric and/or portal vein with the development of regional portal hypertension syndrome;
— compression of the duodenum with the development of duodenal obstruction (must be differentiated from duodenal dystrophy);
- postnecrotic cysts of the pancreas (especially false aneurysms of the arteries of the celiac trunk, superior mesenteric artery).
All operations on the pancreas are associated with a high risk of developing postoperative complications, so their implementation requires strict adherence to the indications for surgical treatment. According to world literature, in the immediate postoperative period, 18–55% of patients developed complications of varying severity [5, 9, 11]. R. McClaine et al. [11] published data showing that in 9% of cases, operations were repeated due to complications that developed, and pancreatic fistulas developed in 14% of patients. According to C. Frey et al. [5, 6], postoperative complications were observed in 19-22% of patients, postoperative mortality was 0.7%. H. Beger et al. when analyzing their own experience in performing resections of the head of the pancreas, they note that postoperative mortality is 0.8%, the rate of relaparotomy is 5.6%, and the overall rate of complications is 20% [2, 14]. The average length of hospital stay after surgery was 14-19 bed days (range 7 to 87 bed days) [2, 5, 14].
When performing the Frey operation, we sought to minimize its morbidity, which is why we completely abandoned the isolation of the portal and superior mesenteric veins. Formation of pancreatojejunostomy with a single-row enveloping suture, in our opinion, reduces damage to the parenchyma of the gland, while providing the necessary tightness. The open-ended design of a continuous suture created by three threads ensures uniform distribution of intracavitary pressure and reduces tissue tension along the suture line.
Despite the fact that we are supporters and promoters of laparoscopic and robot-assisted methods of performing operations on the pancreas, the Frey operation, in our opinion, is advisable to perform from a traditional approach. There are several reasons for this. Frequent bleeding from small arteries of the pancreas, which is easily stopped by suturing after temporary hemostasis due to finger pressure, is difficult to stop with endoscopic access. Coagulation hemostasis, which is fundamental in endoscopic surgery, is unreliable during this operation. The significant length of the continuous suture and the need to ensure uniform tight tension of the thread significantly complicate the endoscopic operation.
A large area of the wound surface of the pancreatic parenchyma, formed during resection of the head of the pancreas, as well as inevitable damage to the parenchyma, are predisposing factors for the development of bleeding in the next 2-3 days after surgery, as well as postoperative pancreatitis. It is for this reason that final hemostasis after resection of the head parenchyma should be achieved by suturing the vessels rather than by coagulation. When bleeding occurs into the lumen of the anastomosis, as a rule, the first leading symptoms are weakness and dizziness, tachycardia and low blood pressure, which occur against the background of complete well-being. Subsequently, melena occurs. During endoscopic examination, as a rule, no blood is found in the stomach and duodenum. If, as a result of conservative treatment, bleeding stops and surgery is not performed, then in the near future there is a high degree of probability that it will recur, since thrombotic masses are quickly lysed under the influence of pancreatic juice. In this regard, patients are subject to careful dynamic monitoring for timely diagnosis of recurrent bleeding. Sewing a bleeding vessel is the only effective and reliable way to stop bleeding into the lumen of the pancreatojejunostomy. During the operation, one of the threads of the upper lip of the anastomosis is removed, blood clots are removed, after which the source of bleeding can be visualized. Final hemostasis is achieved by suturing with a non-absorbable thread using an 8-shaped suture. The integrity of the anastomosis is again restored with a continuous suture.
Thus, the technique we use to perform resection of the head of the pancreas with the formation of a longitudinal pancreatojejunostomy is relatively simple and quite reliable. Only in 6.7% of patients the severity of postoperative complications was assessed as “grade III” and higher. When forming a longitudinal pancreatodigestive anastomosis, we give preference to a continuous single-row suture.