Hereditary diffuse gastric cancer is a type of cancer that is sometimes caused by a mutation in the CDH1 gene. Cancer cells are widespread or scattered throughout the stomach, making it difficult to detect at an early stage. To prevent the development of an aggressive form of stomach cancer, a gastrectomy (complete removal of the organ) is performed. If it is necessary to remove the stomach due to cancer, life expectancy largely depends on the qualifications of the surgeon, the absence of complications and adherence to diet after surgery.
The recommended treatment to prevent the development of an aggressive form of stomach cancer is gastrectomy (complete removal of the organ). It is also performed to treat some non-cancerous conditions. People with other types of stomach cancer may also have a gastrectomy.
Methods of surgical treatment
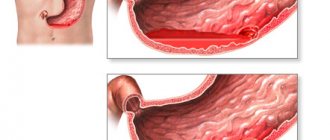
The choice of tactics and extent of surgical intervention depends on the location of the tumor and the extent of the oncological process. During surgery, the organ may be completely or partially removed.
In some situations, it is necessary to remove adjacent structures affected by the tumor (spleen, part of the pancreas, esophagus and liver, intestinal loop).
The goal of surgical treatment is complete excision of the tumor in healthy tissues with the entire ligamentous apparatus and nearby lymph nodes, which are primarily affected by metastases.
The success of the operation and the prognosis of survival largely depend on how many lymph nodes are removed. According to modern international recommendations, at least 15 regional lymph nodes are subject to dissection (removal).
Main methods of surgical treatment:
- total gastrectomy;
- subtotal (partial) resection, which is divided into distal and proximal.
Total gastrectomy – complete removal of the organ, both omentums, tissue and regional lymph nodes. The operation is indicated for a tumor located in the middle third of the stomach, cancer of a macroscopic growth form, hereditary diffuse cancer syndrome and undifferentiated forms of pathology.
As a result of the intervention, an esophageal-intestinal anastomosis is formed: the esophagus is directly connected to the small intestine.
Proximal subtotal resection is performed for exophytic tumor of the fundus and upper third of the stomach, which does not extend to the cardia rosette. At the end of the operation, an anastomosis is performed between the stomach and esophagus.
Distal resection is indicated for exophytic tumor process in the antrum (cancer of the lower third) or a small tumor in the middle third of the stomach.
The operation can be performed in two ways:
- according to Billroth 1─ 1/3 of the stomach is removed, an end-to-end gastroduodenal anastomosis is formed;
- according to Billroth 2 - 2/3 of the stomach is removed, a side-to-side anastomosis is applied between the stump of the stomach and the jejunum, with partial exclusion of the duodenum from the digestive process.
The surgical approach is selected taking into account the location of the tumor and the general condition of the patient. An incision is made along the chest in the area of the ribs (transpleural approach) or along the anterior abdominal wall (transperitoneal approach). A postoperative scar can be located both on the chest and in the middle parts of the abdominal cavity.
Indications and contraindications
As for any operation, as well as for subtotal resection, certain indications are required, which can be absolute or relative. The absolute indications for surgical treatment of the gastrointestinal tract are:
- extensive process of malignant nature;
- stomach ulcers that have a chronic course with the risk of developing into a cancerous process;
- pyloric stenosis in the decompensation phase.
Relative indications include the following body conditions:
- significant increase in body weight, that is, stage 3 obesity;
- pyloric stenosis in the subcompensation or compensation phase;
- some multiple benign formations of the stomach (polyposis);
- chronic ulcers with no effect from therapeutic treatment for 2-3 months.
Despite the fact that this type of treatment is difficult for the body, in case of malignant tumors it saves the patient’s life.
But not all patients undergo this type of surgical treatment. Contraindications for gastric resection are:
- metastasis to the lymph nodes and neighboring organs due to stomach cancer;
- severe general somatic condition of the patient;
- open pulmonary tuberculosis;
- chronic renal and liver failure, in the decompensation phase;
- the presence of ascites, that is, fluid in the abdominal cavity;
- severe course of insulin-dependent diabetes mellitus.
In any case, indications and contraindications for surgical intervention for organ resection are determined by a specialist on an individual basis.
Preparing for surgery
Before surgery, in order to clarify the stage of the disease and develop a treatment plan, a number of diagnostic measures are carried out:
- History taking and physical examination
- Detailed blood test (general and biochemical)
- Clinical urine analysis
- Fecal occult blood test
- ECG
- X-ray examination of the chest in two projections
- Ultrasound of the abdominal organs
- CT, MRI of the affected area
- Gastroscopy with biopsy histology
- Analysis for tumor markers CA 72-4, CEA, Ca 19.9
- Colonoscopy
- Preoperative diagnostic laparoscopy is indicated for patients with total and subtotal lesions of the stomach. This study is carried out to exclude peritoneal carcinomatosis and determine metastases in the abdominal organs that were not detected by non-invasive methods.
- If indicated, additional clinical examinations and consultations with medical specialists are prescribed.
- If there is an increased risk of infectious complications, taking antibacterial drugs is indicated.
- A few weeks before surgery, the patient must begin to adhere to a special diet and avoid aggressive foods. Products are consumed mainly in crushed form, in small portions.
- 7-10 days before the operation, anticoagulants and non-steroidal anti-inflammatory drugs are discontinued.
- Of no small importance is the patient’s psychological attitude and belief in a speedy victory over the disease. The support of relatives and friends helps set the stage for a positive treatment outcome.
Organ-preserving operations
Organ-preserving methods are gaining increasing recognition in the world practice of treating patients with cancer. The indication for such an operation is the detection of early forms of malignant neoplasm.
Early gastric cancer is considered a neoplasm that affects the submucosal layer of the stomach wall and its mucous membrane, regardless of the absence or presence of metastases in the lymph nodes.
If early gastric cancer is detected, it may be possible to perform an organ-preserving intervention - endoscopic resection of the affected area of the mucous membrane within healthy tissue.
The procedure for performing the operation is as follows. After the clear dimensions of the affected area are determined using special dyes, the planned boundaries of the intervention are marked - this is done through electrocoagulation. Next, the surgeon performs hydropreparation of the tissue (this is necessary to ensure better visual control of the layers and prevent possible perforation of the stomach wall). A special electric knife is passed through the instrumental channel of the endoscope, after which, under visual control, resection of the affected area of the mucous membrane and submucosal layer is carried out - down to the muscle layer.
During the rehabilitation period, the patient is under the dynamic supervision of a doctor, receiving the necessary drug therapy. Compared to standard surgical treatment, this method is more economical and less invasive, and also allows to shorten the patient’s hospital stay and speed up rehabilitation.
Contraindications
Stomach surgery for cancer is not always advisable:
- Distant metastases in organs and lymph nodes. In such a situation, surgical intervention is carried out only in the presence of vital indications, with the development of serious complications: bleeding, perforation, tumor stenosis. Lymph dissection is not performed in these cases.
- Serious decompensated pathology of organs and systems.
- Disturbance of the blood coagulation system.
- Extreme exhaustion.
- Peritonitis.
Age is not an obstacle to surgical treatment.
Ways to prolong survival
Palliative techniques are used in relation to inoperable patients with stage 4 cancer. The following methods are used for this:
- Chemotherapy involving systemic administration of powerful cytostatics. The action of such chemotherapy drugs is aimed at suppressing cancer cells that are in the active division phase. Therefore, chemotherapy stabilizes the abnormal growth of the malignancy.
- Irradiation, which is based on the use of ionizing radiation for local effects on the tumor. However, the technique is ineffective against glandular tumors in the stomach, which are resistant to radiation. But some patients may experience slight improvements after a course of radiation therapy.
- A surgical intervention aimed at maintaining the patency of the gastrointestinal tract. It is used as a primary treatment, in particular to eliminate incurable types of carcinoma in the stomach. Surgery can be performed in several ways:
- stenting, when a special mesh is inserted into the gastric lumen to hold the walls of the affected organ and tumor;
- gastrostomy, when in case of inoperable cancer, during radical resection, a thin tube is implanted through the anterior wall of the peritoneum;
- resection, when all or part of the tumor is removed along with surrounding healthy stomach tissue. Less commonly, subtotal excision of the affected organ is performed.
Consequences of surgery to remove the stomach for cancer
Removing the stomach is a technically complex and risky operation that can lead to a number of complications:
- bleeding;
- divergence of internal and external seams;
- postoperative pneumonia;
- thromboembolism.
After almost every operation on the stomach, various types of functional and organic disorders develop associated with the restructuring of the digestive process:
- dumping syndrome;
- anastomositis;
- adductor loop syndrome;
- bile reflux;
- hypoglycemic syndrome;
- anemia;
- small stomach syndrome, early satiety;
- dyspeptic disorders: nausea, belching, vomiting;
- food allergy.
As for mortality, with gastrectomy it is about 10%.
Postoperative period
Adequate management of the postoperative period helps to avoid complications and promotes rapid rehabilitation.
Immediately after surgery, the patient should receive optimal care in the intensive care unit, 24-hour monitoring of vital signs, and adequate pain relief. Typically the patient remains in intensive care for 1 to 3 days.
In the first days, strict bed rest is prescribed.
To prevent congestive pneumonia, starting from the early postoperative period, breathing exercises are performed.
After total removal of the stomach, parenteral nutrition (intravenous drips) is provided for the first days, then the patient is transferred to enteral nutrition through a tube or jejuno- or gastrostomy tube.
Enteral nutrition ensures maximum sparing of the affected organs and rapid healing of the surgical wound. At least 2-3 liters of nutrient solutions should be administered per day.
It is necessary to constantly monitor the level of electrolytes and acid-base balance and, if necessary, immediately correct them.
Cardiovascular and antibacterial drugs are prescribed according to indications.
Adaptation of patients after gastrectomy
Rehabilitation and adaptation to new nutritional conditions lasts about a year. During this period, complications are possible:
- Reflux esophagitis. Inflammation of the esophageal mucosa caused by the reflux of intestinal contents and bile from the small intestine.
- Dumping syndrome. It occurs as a result of the entry of unprocessed food into the intestines and is accompanied by vegetative crises - dizziness, sweating, weakness, palpitations, sometimes after eating a single vomiting occurs.
- Anemic syndrome.
- Fast weight loss.
- Hypovitaminosis - most vitamins are absorbed in the stomach. In its absence, the necessary compounds are not absorbed. Correction: parenteral administration of multivitamin complexes.
These accompanying symptoms are noted by all patients, communicating on the forum and sharing their experiences of how they live after removal of the stomach.
Features of nutrition and diet
Diet therapy in the postoperative period is the main component of rehabilitation.
The main task of the diet:
- create peace for wound healing at the junction of the esophagus and duodenum;
- provide the body with basic nutritional ingredients;
- prevent intestinal bloating.
Immediately after surgery in a hospital setting, the patient is prescribed fasting on the first day. For nutrition, the parenteral method is used, that is, intravenous administration:
- saline solutions (Trisol, Disol);
- amino acids (Aminoplasmal);
- glucose;
- specialized mixtures (Kabiven).
If the postoperative period passes without complications, from the third day you can give a not very sweet compote or rosehip decoction in the amount of 250 ml per day. Drinks are often given by the teaspoon.
Chemotherapy after stomach removal for cancer
Due to the high probability of hidden tumor processes, adjuvant chemotherapy is used to remove micrometastases that remain after radical tumor removal. It is optimal to start cytostatic therapy in the coming days after surgery.
There are various chemotherapy treatment regimens. As a standard for advanced cancer, combinations of chemotherapy drugs are used, which, unlike monotherapy, significantly increase the survival rate.
Drugs are selected individually depending on the stage of the disease, histological picture, patient’s condition and concomitant pathology.
The main drugs for chemotherapy of stomach cancer:
- Ftorafur
- Adriamycin
- 5-fluorouracil
- Mimomycin C
- UFT, S1
- Polychemotherapy: FAM, EAP, FAP, etc.
It is recommended to carry out 6-8 courses of chemotherapy, followed by monitoring the dynamics. The duration of chemotherapy treatment is determined by cyclic cell division, as a result of which not all cancer cells can be simultaneously exposed to cytostatic drugs, which will lead to relapse of the disease.
Gastric resection and survival
Gastric resection - before and after surgery.
Life expectancy after removal of the tumor along with the stomach depends on three factors:
- stage of the disease;
- quality of therapy applied;
- the body's response to treatment.
In world-famous clinics that use advanced technologies, the number of deaths after radical interventions does not exceed 5%. The remaining 95% of patients do not complain of symptoms of relapse of the disease for at least a decade. If the surgery was performed on a subtotal principle, that is, complete excision of the affected organ occurred, survival rate for more than 5 years is 60-70%. But if such a resection was carried out in the last stages of the oncological process, the rate drops to 30-35% of survivors during the first five years.
Dispensary observation
Removal of the stomach is not a 100% guarantee of cure, therefore, in order to prevent recurrence, patients are registered with a dispensary and periodically monitored.
In the first 2 years after the operation, a preventive examination is carried out every 3-6 months, after 3 years - once every six months, 5 years after the operation, annual examinations or unscheduled examinations are indicated if there are complaints.
If the risk of relapse is increased, the interval between preventive examinations is reduced. The scope of preventive examination is determined individually according to clinical indications.
What postoperative complications may occur?
Unfortunately, a 100% cure for cancer is not always possible, especially if the disease was diagnosed at stage 2 or later. Yes, the tumor is removed - the main problem, but other pathological processes may develop that disrupt the patient’s normal lifestyle. Common complications after gastrectomy of any complexity include:
Partial or complete removal of the stomach is often accompanied by complications, one of which is bloating.
- anemia;
- metastasis;
- bloating and abdominal pain;
- dumping syndrome;
- esophagitis;
- stump gastritis;
- anacid and hypoacid state;
- colitis;
- diarrhea;
- peritonitis.
Cancer recurrence
Recurrence of stomach cancer after radical treatment is observed in 20-50% of cases. A second oncological process may develop several months or several years after the operation.
If the relapse is early, then the secondary tumor is most often identified in the area of the anastomosis, if it is late, in the area of the lesser curvature, cardia or stump wall.
Residual cancer occurs within three years from the date of surgery - early relapse. Recurrent cancer develops three years after removal of the primary tumor.
The main cause of relapse is cancer cells that were not removed during surgery. The probability of resumption of the tumor process depends on the stage of the disease and is 20% at stages I and II, 45% at stage III. Low-grade forms of cancer are most susceptible to recurrence.
The prognosis for relapse is serious. Average survival rates do not exceed 25%.
A case of locally advanced gastric cancer
Statistics show that approximately 75% of patients suffer from stage III-IV gastric cancer at the time of hospitalization. This leads to the fact that quite often there is a need for combined operations - they are performed in 30-50% of cases.
Despite the fairly high degree of risk, today combined operations occupy a very important place in the treatment of gastric cancer - this is due to the peculiarities of local spread of the tumor and regional metastasis of the tumor. Even if we are talking about palliative surgery, the intervention in any case reduces the symptomatic manifestations of the disease and increases the life of patients.
The most common combination is surgery accompanied by splenectomy. Resection of the colon and its mesentery, diaphragm, adrenal gland, distal resection of the pancreas, left upper evisceration of the abdominal cavity, and gastropancreatoduodenal resection are performed somewhat less frequently.
Rehabilitation after surgery
The duration of recovery differs in each specific case. The minimum rehabilitation period is at least 3 months. If you follow the recommendations, you can live a completely full life, without serious restrictions.
During the period of scar formation, it is recommended to wear an abdominal bandage. This will significantly speed up the healing of the postoperative wound, reduce the risk of hernias, fix the organs in the correct position and reduce pain.
In the first 6 months after surgery, heavy physical activity and heavy lifting are prohibited in order to prevent the formation of hernias.
For the same reason:
Constipation, severe coughing, and sneezing should be avoided. Physical exercises are performed without involving the abdominal muscles.
After the operation, a vitamin deficiency develops, which is replenished with the help of medications. During total gastrectomy, vitamin B12 injections are prescribed.
It is extremely important to maintain physical activity: light gymnastics, walking in the fresh air, feasible housework - all this contributes to speedy rehabilitation.
Strict adherence to the prescribed diet and nutrition regimen is the main component of successful recovery. It is necessary to completely exclude prohibited foods from the diet.
The psychological aspect is of great importance. A person should not be excluded from public life. Doing what you love, communicating with friends and positive emotions have a beneficial effect on the rehabilitation process.
Survival forecast - how long do they live after surgery?
The prognosis of life expectancy depends on the stage at which the disease was detected, the form of tumor growth, the presence of hidden metastases, the general condition and age of the patient. On average, the five-year survival rate after surgery is about 40%.
Stomach cancer is a serious, often recurrent pathology with an aggressive course, but with an integrated approach to treatment and a positive psychological attitude of the patient, it is quite possible to achieve long-term remission, and in the initial stages even completely cure the disease.