Indications
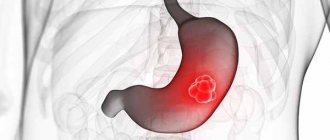
development of stomach cancer
Absolute readings:
- Malignant tumors.
- Chronic ulcers with suspected malignancy.
- Decompensated pyloric stenosis.
Relative readings:
- Chronic gastric ulcers with poor response to conservative treatment (within 2-3 months).
- Benign tumors (most often multiple polyposis).
- Compensated or subcompensated pyloric stenosis.
- Severe obesity.
Preparing for surgery
If the operation is carried out as planned, a thorough examination of the patient is first prescribed.
- General blood and urine tests.
- Study of the coagulation system.
- Biochemical parameters.
- Blood type.
- Fibrogastrodudodenoscopy (FGDS).
- Electrocardiogram (ECG).
- X-ray of the lungs.
- Ultrasound examination of the abdominal organs.
- Examination by a therapist.
Emergency resection is possible in case of severe bleeding or perforation of the ulcer.
Before the operation, a cleansing enema is applied and the stomach is washed. The operation itself usually lasts no more than three hours using general anesthesia.
How is the operation performed?
An upper midline laparotomy is performed.
Gastric resection consists of several mandatory steps:
- Stage I – revision of the abdominal cavity, determination of operability.
- II – mobilization of the stomach, that is, giving it mobility by cutting off the ligaments.
- Stage III – direct cutting off of the necessary part of the stomach.
- Stage IV – creation of an anastomosis between the stump of the stomach and intestines.
After all stages are completed, the surgical wound is sutured and drained.
Types of gastric resection
The type of resection in a particular patient depends on the indications and location of the pathological process.
Based on how much of the stomach is planned to be removed, the patient can undergo:
- Economical resection, i.e. removal of one third to half of the stomach.
- Extensive or typical resection: removal of about two-thirds of the stomach.
- Subtotal resection: removal of 4/5 of the stomach.
- Total resection: removal of more than 90% of the stomach.
According to the location of the excised section:
- Distal resections (removal of the final portion of the stomach).
- Proximal resections (removal of the inlet of the stomach, its cardiac part).
- Median (the body of the stomach is removed, leaving its inlet and outlet sections).
- Partial (removal of only the affected part).
Based on the type of anastomosis formed, there are 2 main methods: Billroth I and Billroth II resections, as well as their various modifications.
Operation according to Billroth I: after removing the outlet section, the gastric stump is connected by a direct connection “output end of the stump - inlet end of the duodenum.” Such a connection is the most physiological, but technically such an operation is quite difficult, mainly due to poor mobility of the duodenum and the discrepancy in the diameters of these organs. Rarely used nowadays.
Billroth II resection: involves suturing the stump of the stomach and duodenum, forming a side-to-side or end-to-side anastomosis with the jejunum.
Gastric ulcer resection
In case of peptic ulcer, in order to avoid relapses, they strive to resect from 2/3 to 3/4 of the body of the stomach along with the antrum and pylorus. The antrum produces the hormone gastrin, which increases the production of hydrochloric acid in the stomach. Thus, we perform anatomical removal of the area that contributes to increased acid secretion.
However, surgery for gastric ulcers was popular only until recently. Resection began to be replaced by organ-preserving surgical interventions, such as excision of the vagus nerve (vagotomy), which regulates the production of hydrochloric acid. This type of treatment is used in those patients who have increased acidity.
Gastric resection for cancer
If a malignant tumor is confirmed, a volumetric resection is performed (usually subtotal or total) with the removal of part of the greater and lesser omentum to prevent relapse of the disease. It is also necessary to remove all lymph nodes adjacent to the stomach, as they may contain cancer cells. These cells can metastasize to other organs.
Removing lymph nodes significantly lengthens and complicates the operation, but ultimately reduces the risk of cancer recurrence and prevents metastasis.
In addition, when cancer spreads to neighboring organs, there is often a need for a combined resection - removal of the stomach with part of the pancreas, esophagus, liver or intestines. In these cases, it is advisable to perform resection as a single block in compliance with the principles of ablastics.
Longitudinal gastrectomy
longitudinal resection of the stomach
Longitudinal resection of the stomach (LG, other names - “drain”, sleeve, vertical resection) is a surgical operation to remove the lateral part of the stomach, accompanied by a decrease in its volume.
Longitudinal gastrectomy is a relatively new method of resection. This operation was first performed in the USA about 15 years ago. The operation is rapidly gaining popularity around the world as the most effective treatment for obesity.
Although during prostate cancer a significant part of the stomach is removed, all its natural valves (cardiac sphincter, pylorus) are left, which allows the physiology of digestion to be preserved. The stomach is transformed from a voluminous bag into a fairly narrow tube. Satisfaction occurs fairly quickly with relatively small portions; as a result, the patient consumes much less food than before surgery, which contributes to sustainable and productive weight loss.
Another important feature of PRG is that the area in which the hormone ghrelin is produced is removed. This hormone is responsible for the feeling of hunger. When the concentration of this hormone decreases, the patient stops experiencing constant cravings for food, which again leads to weight loss.
The functioning of the digestive tract after surgery quickly returns to its physiological norm.
The patient can expect a weight loss equal to about 60% of the excess weight they had before surgery. PGR is becoming one of the most popular surgeries to combat obesity and diseases of the digestive tract.
According to reviews from patients who have undergone prostate cancer, they literally have a new life. Many who gave up on themselves and tried unsuccessfully to lose weight for a long time gained self-confidence, began to actively engage in sports, and improved their personal lives. The operation is usually performed laparoscopically. Only a few small scars remain on the body.
Laparoscopic gastrectomy
This type of surgery is also called “minimal intervention surgery.” This means that surgery is performed without large incisions. The doctor uses a special instrument called a laparoscope. Through several punctures, surgical instruments are inserted into the abdominal cavity, with which the operation itself is performed under the control of a laparoscope.
A specialist with extensive experience using laparoscopy can remove some part of the stomach or the entire organ. The stomach is removed through a small incision no more than 3 cm.
There is evidence of transvaginal laparoscopic resections in women (the stomach is removed through an incision in the vagina). In this case, no scars remain on the anterior abdominal wall.
Gastric resection performed using laparoscopy undoubtedly has great advantages over open one. It is characterized by less severe pain, a milder course of the postoperative period, fewer postoperative complications, as well as a cosmetic effect. However, this operation requires the use of modern suturing equipment and the surgeon's experience and good laparoscopic skills. Typically, laparoscopic gastrectomy is performed when the course of a peptic ulcer is complicated and the use of antiulcer drugs is ineffective. Also, laparoscopic resection is the main method of performing longitudinal resection.
For malignant tumors, laparoscopic surgery is not recommended.
Indications for surgery
Absolute indicators for resection are malignant tumors of the stomach, when surgery gives the patient a chance to prolong life. Doctors prescribe surgical intervention when ulcers do not heal for a long time, the acidity of gastric juice is reduced, or severe scar changes occur that give a pronounced clinical picture.
Stomach cancer
All organs of the human body are made up of cells that grow and divide when new cells are needed. But sometimes this process is disrupted and begins to proceed differently: cells begin to divide when the body does not need it, and old cells do not die. Additional cells accumulate, forming tissue that doctors call a tumor or neoplasm. They can be benign or malignant (cancerous).
Stomach cancer begins in the inner cells, but over time invades the deeper layers. In this case, the tumor can grow into neighboring organs: the esophagus, intestines, pancreas, liver. The causes of malignant neoplasms of the stomach are divided into several types:
- poor nutrition, especially associated with the abuse of fried, canned, fatty and spicy foods;
- smoking and alcohol;
- chronic diseases of the gastrointestinal tract: ulcers, gastritis;
- hereditary predisposition;
- hormonal activity.
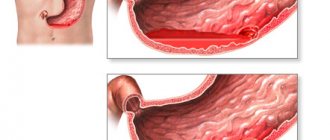
Severe stomach ulcer
An ulcer is a defect in the gastric mucosa. Peptic ulcer disease is characterized by periodic exacerbations, especially in the spring and autumn. The main reason for the development of the disease is frequent stress, which strains the nervous system, which causes muscle spasms in the gastrointestinal tract. As a result of this process, a malfunction in the nutrition of the stomach occurs, and gastric juice has a detrimental effect on the mucous membrane. Other factors leading to the development of peptic ulcers:
- disrupted diet;
- chronic gastritis;
- genetic predisposition;
- long-term medication use.
With a chronic gastric ulcer, the formation of ulcerative defects occurs on the mucous membrane of the organ. Resection of these pathologies is performed when complications of the disease develop, when there is no effect from conservative therapy, bleeding occurs, and stenosis develops. This is the most traumatic type of surgery for stomach ulcers, but also the most effective.
- Ringworm in dogs - types of disease, routes of infection, symptoms, home treatment and prevention
- Russians plan to abolish transport tax
- Moscow pensioners will increase the minimum pension amount
Laparoscopic resection for obesity
Laparoscopic surgery is an endoscopic method of gastric surgery, which is performed through punctures in the abdominal cavity with a special instrument without a wide incision. This resection is carried out with the least trauma for the patient, and the cosmetic postoperative result is much better. The indication for laparoscopic gastrectomy is the extreme stage of obesity, when neither medication nor a strict diet helps the patient.
With obesity, a metabolic disorder occurs, and when the process of losing weight can no longer be controlled, doctors have to remove part of the stomach, after which the patient gets rid of the problem, loses weight and gradually returns to everyday life. But the biggest advantage of laparoscopy is the restoration of normal metabolism, reducing the risk of atherosclerosis and coronary heart disease. Watch the video to see how laparoscopic gastrectomy is performed:
Complications
Among the complications that arise during the operation itself and in the early postoperative period, it is necessary to highlight the following:
- Bleeding.
- Infection in the wound.
- Shock.
- Peritonitis.
- Thrombophlebitis.
In the later postoperative period, the following may occur:
- Anastomotic failure.
- The appearance of fistulas at the site of the formed anastomosis.
- Dumping syndrome (discharge syndrome) is the most common complication after gastrectomy. The mechanism is associated with the rapid entry of insufficiently digested food into the jejunum (the so-called “food failure”) and causes irritation of its initial section, a reflex vascular reaction (decreased cardiac output and dilation of peripheral vessels). It manifests itself immediately after eating with epigastric discomfort, severe weakness, sweating, increased heart rate, dizziness and even fainting. Soon (after about 15 minutes) these phenomena gradually disappear.
- If gastric resection was performed for peptic ulcer disease, then it may recur. Almost always, recurrent ulcers are localized on the intestinal mucosa, which is adjacent to the anastomosis. The appearance of anastomotic ulcers is usually a consequence of a poorly performed operation. Most often, peptic ulcers form after Billroth-1 surgery.
- Recurrence of a malignant tumor.
- Weight loss may occur. Firstly, this is caused by a decrease in the volume of the stomach, which reduces the amount of food taken. And secondly, the patient himself strives to reduce the amount of food eaten in order to avoid the appearance of unwanted sensations associated with dumping syndrome.
- When performing Billroth II resection, the so-called afferent loop syndrome may occur, the occurrence of which is based on violations of the normal anatomical and functional relationships of the digestive tract. It manifests itself as bursting pain in the right hypochondrium and bilious vomiting, which brings relief.
- Iron deficiency anemia may be a common complication after surgery.
- Much less common is B12 deficiency anemia due to insufficient production of Castle factor in the stomach, through which this vitamin is absorbed.
Basic methods of performing the operation
There are many different options for gastric resection and reconstruction. Theodor Billroth first performed such an operation back in 1881, and in 1885 he also proposed another way to restore the functioning of the gastrointestinal tract. These gastric surgeries are still used today, but today they have been modernized and simplified, so they are available to a wide range of practicing surgeons. The doctor selects the type of operation individually in each case, but more often they use:
- Subtotal distal resection, when the lesion is located in the pyloroantral part of the lower third of the stomach (the entire lesser curvature).
- Subtotal proximal resection, performed for stage 1 and 2 gastric cancer, when the lesser omentum, lymph nodes, lesser curvature and a section of the greater omentum are removed.
- Gastrectomy, which is performed in the presence of a primary multiple tumor or infiltrative cancer located in the middle part of the stomach. The entire organ is removed, and an anastomosis is performed between the esophagus and the small intestine.
By Billroth 1
Gastric resection according to Billroth 1 is the excision of 2/3 of the organ, when the physiological path of food movement with the participation of pancreatic excretion and bile is preserved. During surgery, the anastomosis of the duodenum and stomach is connected end to end. This method is used for polyps, malignant ulcers, and small cancerous tumors of the gastric antrum.
- Salad with chicken and prunes - simple step-by-step recipes for cooking at home with photos
- Pain under the right shoulder blade
- Why does it hurt when you pee
By Billroth 2
During Billroth 2 resection, a large part of the blind stump of the duodenum and stomach, anterior and posterior anastomosis (connection of two organs) are removed. After this operation, the physiological path of food movement is disrupted - it enters directly into the jejunum, and bile reflux is possible and the anastomosis is disrupted. Resection according to Billroth 2 has more indications, since it is performed on gastric ulcers of any location and for cancer, since it gives the doctor the opportunity to perform extensive removal of the organ up to 70%.
According to Hoffmeister-Finsterer
The Hofmeister-Finsterer technique is a modified version of Billroth 2, which provides for resection of at least 2/3 of the organ for peptic ulcer disease. During the operation, the entire secretory zone is removed, after which the motor function of the stomach undergoes significant changes: peristalsis weakens, the function of the pylorus, which ensures the gradual evacuation of food, disappears altogether.
By Ru
The Roux method is the removal of part of an organ with a Y-shaped gastroenteroanastomosis. In this case, the jejunum is divided, and its distal end is sutured and connected to the lower third of the gastric stump. This is also a modification of Billroth 2, which is indicated for duodenogastric reflux esophagitis, which is characterized by the reflux of the contents of the duodenum into the stomach.
According to Balfour
The Balfour method involves placing a gastrointestinal connection on a long loop of jejunum. This method prevents pathological changes in the organs of the gastrointestinal tract, and is also used for very high resection due to peptic ulcer or the impossibility of suturing in another way due to the anatomical features of the gastric stump. Balfour resection eliminates the gap between the knees of the jejunum, which eliminates the future occurrence of intestinal obstruction.
Nutrition, diet after gastrectomy
The patient's nutrition immediately after surgery is carried out parenterally: saline solutions, glucose solutions and amino acids are administered intravenously.
After surgery, a nasogastric tube is inserted into the stomach to suction out the stomach contents, and nutritional solutions can also be administered through it. The tube is left in the stomach for 1-2 days. Starting from the third day, if there is no congestion in the stomach, you can give the patient a not too sweet compote in small portions (20-30 ml), rosehip decoction about 4-6 times a day.
Next, they switch to semi-liquid pureed food (mashed potatoes, vegetable broths, liquid porridges, slimy soups). Food for feeding the patient in the postoperative period should be prepared only by steaming.
In the future, the diet will gradually expand, but an important condition must be taken into account - patients will have to follow a special diet, balanced in nutrients and excluding coarse, indigestible foods. The food that the patient takes must be thermally processed, consumed in small portions and should not be hot. Complete exclusion of salt from the diet is another condition of the diet.
The volume of a serving of food is no more than 150 ml, and the frequency of intake is at least 4-6 times a day.
This list contains foods that are strictly prohibited after surgery:
- Any canned food.
- Fatty dishes.
- Marinades and pickles.
- Smoked and fried foods.
- Baking.
- Carbonated drinks.
The hospital stay is usually two weeks. Complete rehabilitation takes several months. In addition to following the diet, it is recommended:
- Limiting physical activity for 2 months.
- Wearing a postoperative bandage for the same time.
- Taking vitamin and mineral supplements.
- If necessary, take hydrochloric acid and enzyme preparations to improve digestion.
- Regular monitoring for early detection of complications.
Patients who have undergone gastrectomy must remember that the body’s adaptation to new digestive conditions can take 6-8 months. According to reviews from patients who have undergone this operation, weight loss and dumping syndrome are most pronounced at first. But gradually the body adapts, the patient gains experience and a clear understanding of what diet and what foods he tolerates best.
After six months to a year, the weight gradually returns to normal, and the person returns to normal life. It is not at all necessary to consider yourself disabled after such an operation. Many years of experience with gastric resection proves that it is possible to live without part of the stomach or even completely without the stomach.
If indicated, gastric resection surgery is performed free of charge in any abdominal surgery department. However, it is necessary to take a serious approach to the issue of choosing a clinic, because the outcome of the operation and the absence of postoperative complications depend to a very large extent on the qualifications of the operating surgeon.
Prices for gastric resection, depending on the type and volume of the operation, range from 18 to 200 thousand rubles. Endoscopic resection will cost slightly more.
Sleeve resection for the treatment of obesity is, in principle, not included in the list of free medical care. The cost of such an operation is from 100 to 150 thousand rubles (laparoscopic method).
Billroth-1: disadvantages
Operations according to Billroth 1 and 2 also have certain disadvantages. They must be taken into account when choosing a surgical procedure. During the Billroth-1 operation, duodenal ulcers may be observed.
With this method of surgical intervention, it is not possible to qualitatively mobilize the intestine in all cases. This is necessary to create an anastomosis without tension on the suture. This problem occurs especially often in the presence of duodenal ulcers that penetrate into the pancreas. Also, severe scarring and narrowing of the intestinal lumen can lead to the inability to properly mobilize the duodenum. The same problem occurs when ulcers develop in the proximal stomach.
Some surgeons enthusiastically insist on performing Billroth-1 resection, even if there are a number of unfavorable conditions for its implementation. This significantly increases the likelihood of suture failure. Therefore, in some cases it is necessary to abandon the Billroth-1 operation. If there are significant difficulties, it is better to give preference to surgical intervention using the second method.
It is extremely important that the technique of the surgeon who will perform the operation be carefully honed and practiced as much as possible. Although Billroth-1 is considered an easier, faster technique, it is performed exclusively according to strict indications. The decision to conduct it is made only if certain factors are present and certain obstacles are absent.
In some cases, this operation requires mobilizing not only the duodenum, but also the spleen and intestinal stump. In this case, it is possible to create a seam without tension. Extensive mobilization greatly complicates the operation. This unnecessarily increases the risk during its implementation.
It is also worth noting that resection using the Billroth-1 technique is not performed during the treatment of gastric cancer.