Gastrectomy is an operation during which the surgeon removes the stomach and connects the remaining ends of the esophagus and duodenum. This is a fairly complex surgical procedure, and serious complications can develop after it. But in some cases, such as cancer, gastrectomy is the only way to cure a person and save his life.
Our expert in this field:
Ryabov Konstantin Yurievich
Chief surgeon, oncologist, endoscopist
Call the doctor
The stomach performs many important functions. It produces digestive enzymes and hydrochloric acid, and absorbs water and salt. In the area of the fundus and body of the stomach there are special glands that produce Castle factor - this enzyme promotes the absorption of vitamin B12 and prevents anemia. Hydrochloric acid kills pathogenic bacteria and prevents them from entering the intestines. Therefore, gastrectomy is resorted to only in cases where there is no other option and the benefits of the operation outweigh the risk of possible complications.
Indications for gastrectomy
The main indication for gastrectomy is stomach cancer. But not every malignant tumor requires complete removal of the organ. Gastrectomy is used if the cancer has spread throughout the entire stomach or is located in its upper part. Together with the stomach, nearby (regional) lymph nodes are removed, the omentum is a double layer of peritoneum (a thin film of connective tissue that lines the walls of the abdominal cavity and covers the abdominal organs), stretched between the liver, duodenum and stomach.
Sometimes, if the tumor has grown significantly, it is necessary to remove part of the intestine, esophagus, pancreas, spleen or other organs affected by cancer. This type of gastrectomy is called combined . It is effective only in cases where the cancer has spread to neighboring organs to a limited extent. For multiple metastases, surgical treatment is ineffective.
Often, the surgeon makes the final decision about whether he will remove the entire stomach or only part of it already during the operation, when it is possible to assess the nature of tumor growth and the degree of spread to neighboring structures. Surgeons have this rule: if any surgical intervention is performed for stomach cancer, you should always prepare for the fact that it may end in gastrectomy.
Some people have mutations in the CDH1 gene. They lead to hereditary diffuse gastric cancer , a dangerous disease in which tumor cells are scattered throughout the organ, making the tumor very difficult to detect at an early stage. Often, mutation carriers are recommended to undergo prophylactic gastrectomy.
Very rarely, gastrectomy is used for other diseases:
- Gastric polyposis.
- An ulcer that is located in the upper part of the organ.
- Zollinger-Ellison syndrome is a tumor in the pancreas that produces the hormone gastrin . It causes the stomach lining to produce a lot of hydrochloric acid. Because of this, ulcers occur in the stomach and duodenum that cannot be treated.
Material and methods
The study included 145 patients with stages I-IV gastric cancer who underwent surgical treatment at the Russian Research Center for Cancer Research from 2002 to 2013. All patients underwent a comprehensive examination at the preoperative stage aimed at verifying and clarifying the extent of gastric cancer. Concomitant diseases were present in 93 (64%) patients. Excess body weight (body mass index more than 25 kg/m2) was noted in 23 (15.7%) patients. The patients were divided into two groups: in group 1 ( n
=71) at the reconstructive stage, an esophageal-intestinal anastomosis was formed manually, in the 2nd group (
n
=74) - an esophageal-intestinal hardware circular anastomosis. In most cases, the anastomosis was formed on an end-to-side loop of jejunum disconnected according to Roux; in two cases, esophagojejunostomy was formed on a loop of jejunum (in one of them, with the creation of a reservoir according to Rodino) and in another observation, esophagojejunostomy was performed. The anastomosis was formed manually using separate interrupted double-row sutures with non-absorbable threads on an atraumatic needle. Among the surgical approaches, median laparotomy predominated - in 54 observations, combined thoradiaphragmolaparotomy access was used in 17 observations. Gastrectomy was performed in 47 cases, gastrectomy with resection of the lower third of the esophagus - in 17 cases. In 7 patients, combined operations with splenectomy, resection of the pancreas or transverse colon were performed. Gastric tumors of stages IIIa-IIIc according to the TNM system prevailed in terms of prevalence - 63 observations. The average duration of the reconstructive stage of the operation in this group was 72±21.9 minutes.
To apply mechanical sutures, circular staplers from four different manufacturers were used. All anastomoses were performed on a Roux-enhanced loop of jejunum. The technique for forming the anastomosis is described in detail above. Among surgical approaches in this group of patients, median laparotomy also predominated - 59 observations. The remaining operations were performed using a combined thoracodiaphragmolaparotomy access in the sixth intercostal space on the left. Isolated gastrectomy was performed in 49 patients, combined operations with resection of the esophagus and/or adjacent organs - in 26 cases. The prevalence of gastric cancer and general characteristics of patients are presented in Table. 1.
Table 1. General characteristics of observations
A number of complications arose in the immediate postoperative period (Table 2).
Table 2. Complications in the immediate postoperative period Complications directly related to the method of anastomosis formation (its failure) were noted in one patient of the 1st group and in two patients of the 2nd group. However, if relaparotomy was required in case of failure of manual anastomosis, then when using a mechanical suture, patients were treated conservatively with implantation of an esophageal stent and in both cases there was no death.
69 (47.6%) patients were followed up for a period of 1 to 10 years. Complications potentially associated with the technique of formation of esophagojejunostomy were studied (Table 3).
Table 3. Long-term complications
Preparing for surgery
Before the operation, the doctor prescribes urine blood tests, x-rays, CT, MRI and other diagnostic methods. They are needed in order to assess the patient’s health, the extent of cancer spread, and determine the extent of surgical intervention.
Some patients have disorders in the body that require correction before surgery. In such cases, the doctor may prescribe IVs with water-salt solutions, blood transfusions and blood substitutes, red blood cells, drugs to improve the functioning of the cardiovascular system, antibiotics to prevent infections.
Reviews from our patients
- Feedback on the treatment of stomach cancer
Feedback on stomach cancer treatment January 13, 2021The patient was admitted to the clinic for diagnosis and treatment of stomach cancer. The tumor was verified as soon as possible. A central venous port system was installed. The first of four courses of chemotherapy was completed. After completing this stage of treatment and reducing the size of the tumor, a surgical operation for gastric resection is planned.
read more
- Feedback on the treatment of stomach disease
Feedback on the treatment of stomach disease December 8, 2021
The patient was admitted in serious condition with symptoms such as repeated vomiting, severe weakness, and increased abdominal volume. The cause is a stomach disease. Other clinics refused to treat the patient due to the complexity of the diagnosis. During hospitalization at the Medicine 24/7 clinic, fluid from the abdominal cavity was evacuated, which led to an improvement in the general condition. At the second stage of treatment, stenting of the gastric outlet was performed. Thanks to this, the patient...
read more
- Feedback on the treatment of stomach cancer 10/20/2020
Review of treatment for stomach cancer October 20, 2020 October 20, 2021
The patient was admitted to the Medicine 24/7 clinic with a stomach disease aggravated by somatic diseases. To date, treatment tactics have been selected, including courses of chemotherapy.
read more
- Feedback on the treatment of stomach cancer 09.23.2020
Feedback on the treatment of stomach cancer September 23, 2020 September 23, 2021
A patient's wife talks about her husband's treatment. Diagnosis: stomach cancer. At his place of residence, he was denied treatment. The Medicine 24/7 clinic was able to help. The patient’s wife notes the efficiency of the entire staff, their mobility, and professionalism. In particular, she thanks the attending physician Milana Khanlarovna Mustafaeva.
read more
- Feedback on photodynamic therapy
Feedback on photodynamic therapy July 21, 2020
Mikhail Lvovich is 92 years old. He went to the Medicine 24/7 clinic for treatment of stomach cancer. Surgery and chemotherapy courses are not indicated at his age, as they can lead to significant complications. An individual treatment plan has been developed for the patient, including sessions of endoscopic photodynamic therapy. A positive effect has been achieved. In addition, molecular genetic diagnosis of the tumor was carried out, which in the future will make it possible to select…
read more
- Successful treatment of stage IV gastric cancer with metastases at the Medicine 24/7 clinic
Successful treatment of stage IV gastric cancer with metastases at the Medicine 24/7 clinic November 21, 2021
Here is an example of the effectiveness of properly selected treatment. Even when there seems to be no chance and no one can help. Elena was diagnosed with stage IV gastric cancer with metastases. Treatment included gastrectomy and targeted selective therapy. It gave results. According to the latest examination, the patient has no signs of the disease. Despite this, treatment continues until complete victory. "Thanks a lot! You gave...
read more
- Anna Sergeevna about the treatment of stomach cancer
Anna Sergeevna about the treatment of stomach cancer June 29, 2021
Anna Sergeevna was admitted to the Medicine 24/7 clinic in serious condition. Due to stomach cancer, the patency of her esophagus was impaired. At the clinic, her condition worsened, any food intake was impossible, and continuous vomiting began. During the examination, an inoperable stenosis was discovered. A decision was made to perform stenting. During the procedure, a unique stent was installed, 70 centimeters long. Thus, the clearance...
read more
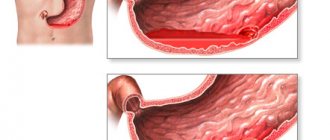
Anastomositis after gastrectomy treatment
Anastomositis is an inflammatory process that develops at the site of the connection (anastomosis) formed as a result of surgery between different parts of the digestive tract, in order to restore its integrity.
After total removal of the stomach, surgeons form an anastomosis between the cardiac part of the esophagus and the small intestine. During partial resection of the stomach, the remaining part of the stomach and duodenum are sutured.
The exact causes of the disease are unknown. It is assumed that risk factors for the occurrence of pathology:
- Incorrect technique for applying a connecting suture. Thus, a continuous seam and through punctures with a needle increase the likelihood of developing an inflammatory process.
- Individual characteristics of the patient's body. In some chronic diseases (for example, diabetes), as well as in elderly patients, the ability of tissues to recover from damage is significantly reduced, which leads to failure of the formed connections.
- Type of suture material. It is possible to develop an allergy to foreign proteins included in its composition. For example, catgut, which is made from the intestines of cattle.
- Compression of the anastomosis by other abdominal organs. The pressure of the swollen intestinal loops makes it difficult for the sutures to heal.
- Removal of 2/3 of the stomach due to peptic ulcer increases the risk of anastomositis.
- Infection of the junction.
- Disturbances of protein and acid-base homeostasis in the postoperative period. A drop in the concentration of proteins in the blood plasma and the development of acidosis reduce the intensity of tissue regeneration.
Development of the process in the esophagus
- The surgeon made erroneous actions during the operation: stitches were placed incorrectly, part of the organ was removed more than necessary.
- The circulatory and nervous system damaged during surgery.
- Improper patient care during the postoperative period.
- Damage to the structure of the pancreas with dysfunction.
- Low immune response of the body due to chronic stress and colds.
- Violation of doctor's orders. Refusal to take medications.
- Failure to comply with bed rest and prescribed strict diet.
In addition to the imbalance between the secretion of pepsin, hydrochloric acid and a decrease in the protective function of the digestive organs, the following causes of the development of peptic ulcer are identified:
- Helicobacter pylori infection;
- taking certain medications;
- genetic predisposition;
- bad habits;
- malignant and benign neoplasms;
- chronic inflammatory processes;
- HIV, syphilis, tuberculosis;
- cancer;
- diabetes.
Stress peptic ulcers of the stomach are often diagnosed with prolonged chronic stress, depression, anxiety due to inflammation of the vagus nerve, which provokes excessive secretion of pepsin and hydrogen chloride and a decrease in the production of protective mucus.
The most rare type of peptic ulcer disease is damage to the distal segment of the esophagus. In 20% of cases it is combined with peptic ulcer of the stomach and duodenum. They are divided into chronic (when the cause exists for a long time) and acute (arising after surgery, accompanied by vomiting of acidic stomach contents).
The ratio of ulcers on the esophagus to damage to the stomach and duodenum is 1:50. Peptic ulcers on the esophagus occur in the lower part of the organ, in a place where gastric contents are often thrown back, corroding the tissue. At the initial stage, when exposed to gastric secretions, hyperemia of the epithelium appears, followed by the formation of ulcers, which heal with the appearance of scars.
Refusal of stomach contents occurs, among other things, due to dysfunction of the sphincter of the lower esophagus. Therefore, the precursor of peptic ulcer of the esophagus is reflux esophagitis. Etiologically, this disease is divided into symptomatic and peptic. Symptomatic ones are characterized by the absence of a hiatal hernia or gastroesophageal reflux.
A peptic ulcer of the esophagus develops when:
- the entry of hydrochloric acid and enzymes from the stomach into the esophagus;
- axial hiatal hernia;
- after surgery on the lower esophageal sphincter;
- violation of peristalsis;
- diseases of the biliary system.
Symptoms and clinical picture:
- frequent heartburn;
- vomit;
- pain when swallowing;
- melena (dark-colored stool due to blood present in it);
- dysphagia (swallowing disorder).
Methods for treating acute, chronic stages and complications of peptic ulcers
Acute anastomositis after gastrectomy develops in all patients in the first 4–5 days after surgery and has the character of acute inflammation. The reason for its occurrence is injury to the tissues of the digestive tract with surgical instruments. The inflammatory process is accompanied by severe swelling of the mucous membrane in the area of the sutures.
The incidence of chronic anastomositis is highest in the first 5 years after gastrectomy. More often this complication occurs in men. The constant inflammatory process occurring in the area of surgical sutures leads to disruption of the functioning of organs. The occurrence of cicatricial changes in the mucous membrane leads to the appearance of an area of narrowing of the digestive tube and stagnation of the contents.
The prognosis of the disease depends on the activity of the inflammatory process and accompanying complications such as the formation of scars and ulcerative lesions. In the most severe form of the disease, necrotic ulcerative lesions of the junction area are formed with possible perforation into the abdominal cavity.
In the acute course of the disease (newly diagnosed ulcer), conservative methods of drug therapy in combination with a strict therapeutic diet are acceptable.
The chronic form occurs with non-healing ulcers and is prone to relapses (exacerbation stages) and remissions (attenuation of symptoms).
If both forms are not treated, the peptic ulcer may become more complicated, in such cases hospitalization followed by surgery is recommended.
In uncomplicated cases, it is recommended:
- drug therapy;
- diet;
- being in a hospital (during an exacerbation and in the acute stage with pronounced symptoms);
- physiotherapy;
- Spa treatment.
The drug treatment package includes:
- antibiotics (in cases of Helicobacter pylori infection);
- antisecretory drugs;
- healing medications;
- antacids;
- healing mineral waters;
- cytoprotectors (protecting the mucous membrane).
The choice of diet depends on the stage of the disease, the presence of complications and concomitant diseases.
Strict adherence to the doctor’s dietary instructions helps speed up healing and reduce relapses.
In addition to following a diet, patients are recommended to get rid of bad habits (drinking alcohol-containing drinks, smoking), not to take aspirin and other non-steroidal anti-inflammatory drugs.
During treatment, doctors recommend minimizing physical activity and eliminating emotional stress.
Classification
After organ resection, post-gastroresection disorders may occur.
The nature of the operation performed divides postoperative disorders into post-gastroresection and post-vagotomy. Clinical manifestations depend on the type of surgery performed. Gastric resection is carried out in three ways: Billroth I, Billroth II, Roux. Vagotomy can be performed at all levels; a distinction is made between trunk and selectively proximal.
Prevention
A peptic ulcer (peptic ulcer) is an open ulcer that forms on the mucous membrane of the lower esophagus, stomach and duodenum. The most common manifestation of a peptic ulcer is abdominal pain. A peptic ulcer that occurs on the lining of the stomach is called a gastric ulcer (peptic ulcer).
Ulcers can occur in the lower part of the esophagus and in the duodenum (duodenal ulcer). Modern science believes that peptic ulcers are not caused by spicy foods, or even stress at work. Today we can say with confidence that bacterial infection and the use of certain medications play a leading role in the development of peptic ulcers.
Diseases of the operated stomach arise as complications after surgery. To prevent their occurrence, the probabilities of the outcome of surgical intervention should be calculated. If possible, avoid using a scalpel. Surgery has contributed to the emergence of a remote method of dealing with complications.
How is a gastrectomy performed?
The operation lasts 4–5 hours. It is performed under general anesthesia. The stomach can be removed in two different ways:
- Through the cut. This approach is used in most cases.
- Laparoscopically - through punctures in the abdominal wall. Such operations are considered very promising, they are better tolerated and can reduce the recovery period. But some doctors and researchers believe more research is needed before laparoscopic surgery can be considered the standard approach to gastrectomy for gastric cancer.
During surgery, the doctor removes the stomach and other affected organs. The esophagus is then connected to the small intestine.
Rehabilitation after surgery
A patient who has undergone a gastrectomy is usually discharged from the hospital after 7–14 days. Eating by mouth is prohibited for the first 3–5 days. You can only moisten your lips with water to prevent them from drying out. All this time, the person receives nutrient solutions intravenously.
Painkillers and medications are prescribed to correct disorders in the body and improve the functioning of internal organs. The sutures are tied daily, and X-rays are periodically taken to check the integrity of the sutures on the esophagus and intestines.
Diet and nutrition after surgery
During the first time after surgery, the patient is given intravenous parenteral nutrition solutions containing amino acids, carbohydrates and small amounts of fats. Two days after resection, the patient can drink liquids (decoctions, tea, compote) in small portions and often. Baby formulas begin to be administered through a tube. Gradually, the diet expands, and after two weeks the patient can independently adhere to a gentle diet, the purpose of which is to prevent inflammatory processes and complications (for example, dumping syndrome).
In the late postoperative period, it is better to give preference to purees and soups based on vegetables or cereals (but without cabbage or millet). The method of preparing other dishes can be steamed, oven-baked or boiled; fried foods should be avoided. You need to refrain from eating baked goods during the first month, and after that, control your consumption within reasonable limits. It is also better to limit plant foods containing a coarse fibrous structure. You can only eat lean meat; give preference to poultry (turkey, chicken). The fish consumed should also not contain large quantities of fat (bream, hake, cod, pike perch). Dairy products, milk and eggs can be eaten in limited quantities and not earlier than 2 months after surgery.
After removing part of the stomach, the patient will have to eat small portions and quite often (up to 5 times a day). Small portions will not cause discomfort, since the feeling of hunger does not form if the stomach is full. You should not try to increase single servings; this can lead to stretching of the gastric wall and the formation of an overly large stomach, which is undesirable for patients with existing obesity, which was the reason for seeing a doctor.
That is why, when forming a diet, they pay attention to the primary reason for visiting a doctor.
If the patient has suffered from a peptic ulcer for a long time, then the diet after gastrectomy in the postoperative period should limit the consumption of acidic foods, include the intake of mineral water and antacid and antibacterial (targeted Helicobacter Pylori) drugs.
Possible complications
The risk of complications after gastrectomy is quite high, because patients with stomach cancer are most often elderly people who have concomitant diseases. Possible complications:
- Infection of a postoperative wound. Antibiotics are used to prevent and treat this condition.
- Failure of sutures on the esophagus and intestines. Because of this, the contents of the intestine enter the abdominal cavity, which can cause the death of the patient. In order to eliminate this complication, it is necessary to resort to repeated surgery.
- Internal bleeding is also a dangerous complication that must be corrected surgically.
- Small intestinal obstruction.
After a gastrectomy, digestion is disrupted; the body needs some time to adapt to the absence of a stomach and a change in diet. Because of this, some patients lose a lot of weight. This is especially dangerous for cancer patients.
A common complication of gastrectomy is dumping syndrome . For normal digestion in the small intestine, it is important that the food that enters it is well processed in the stomach. If this does not happen, irritation of the mucous membrane with a food bolus provokes a strong flow of blood to the intestine, while the brain does not receive enough blood. Because of this, after eating a person becomes pale, his skin becomes covered with sweat, his heartbeat quickens, and he wants to lie down quickly. After an attack, rumbling in the stomach and diarrhea often occur.
Some tips will help you cope with the unpleasant manifestations of dumping syndrome:
- Avoid sweets. Dumping syndrome is caused by foods that contain a lot of sugar and starch.
- Eat slowly.
- Lie down and rest for 25 minutes after eating.
- Increase the amount of fiber in your diet slowly.
- Avoid soups and other liquid dishes.
- Eat more often and in small portions.
In most cases, symptoms improve over time. If they persist and cause severe discomfort, you should consult a doctor. There are three degrees of severity of dumping syndrome:
- Easy . Symptoms occur 1-2 times a month and go away on their own within 20-30 minutes.
- Medium-heavy . Symptoms occur 3–4 times a week and last 1–1.5 hours.
- Heavy . Attacks occur every time while eating, symptoms persist for 2.5–3 hours, the person cannot eat normally.
The stomach is necessary for the absorption of vitamins B12, D, C. After a gastrectomy, a deficiency of these substances may occur in the body, which can lead to anemia (signs: pale skin, weakness, dizziness, headaches), a decrease in the body’s resistance to infections, and weakening of bones and muscles.
Get a consultation with a doctor
Anastomositis after gastrectomy: what is it, how does it manifest and is treated
Anastomositis is a pathology that develops after complete or partial removal of the stomach.
The disease belongs to a group of syndromes that have a common name - disease of the operated stomach. The incidence of postoperative anastomositis reaches 25%. Read further about the causes, main symptoms of the disease, its diagnosis, as well as how anastomositis is treated after gastric resection.
Causes of anastomositis
Anastomositis is an inflammatory process that develops at the site of the connection (anastomosis) formed as a result of surgery between different parts of the digestive tract, in order to restore its integrity.
After total removal of the stomach, surgeons form an anastomosis between the cardiac part of the esophagus and the small intestine. During partial resection of the stomach, the remaining part of the stomach and duodenum are sutured.
The exact causes of the disease are unknown. It is assumed that risk factors for the occurrence of pathology:
- Incorrect technique for applying a connecting suture. Thus, a continuous seam and through punctures with a needle increase the likelihood of developing an inflammatory process.
- Individual characteristics of the patient's body. In some chronic diseases (for example, diabetes), as well as in elderly patients, the ability of tissues to recover from damage is significantly reduced, which leads to failure of the formed connections.
- Type of suture material. It is possible to develop an allergy to foreign proteins included in its composition. For example, catgut, which is made from the intestines of cattle.
- Compression of the anastomosis by other abdominal organs. The pressure of the swollen intestinal loops makes it difficult for the sutures to heal.
- Removal of 2/3 of the stomach due to peptic ulcer increases the risk of anastomositis.
- Infection of the junction.
- Disturbances of protein and acid-base homeostasis in the postoperative period. A drop in the concentration of proteins in the blood plasma and the development of acidosis reduce the intensity of tissue regeneration.
Acute and chronic anastomositis
Acute anastomositis after gastrectomy develops in all patients in the first 4–5 days after surgery and has the character of acute inflammation. The reason for its occurrence is injury to the tissues of the digestive tract with surgical instruments.
The inflammatory process is accompanied by severe swelling of the mucous membrane in the area of the sutures. As a result, complete or partial obstruction of the operated area of the gastrointestinal tract develops. Within a week, acute inflammation subsides and the anastomosis is restored.
In 10–15% of cases, acute anastomositis becomes chronic.
The incidence of chronic anastomositis is highest in the first 5 years after gastrectomy. More often this complication occurs in men.
The constant inflammatory process occurring in the area of surgical sutures leads to disruption of the functioning of organs.
The occurrence of cicatricial changes in the mucous membrane leads to the appearance of an area of narrowing of the digestive tube and stagnation of the contents.
Symptoms of anastomositis
Patients present a whole range of complaints related to disruption of the gastrointestinal tract. Among them:
- nausea;
- belching;
- heartburn;
- bitter taste in the mouth;
- increased salivation;
- vomiting of food contents mixed with bile;
- heaviness in the epigastric region after eating;
- decreased appetite;
- pain in the epigastric region, as well as throughout the abdomen;
- flatulence.
In addition, patients complain of a deterioration in their general condition:
- weight loss;
- poor sleep;
- headache;
- increased fatigue;
- heartache;
- dizziness.
Diagnostics
The diagnosis is made using endoscopic examination methods, as well as x-rays of the stomach using a radiopaque agent.
X-ray of the stomach is performed using a barium suspension as contrast. The examination allows you to identify areas of narrowing in the anastomosis zone and assess the rate of evacuation of barium suspension.
What are the features of the operation and what patients may encounter can be found in this video.
Treatment
Therapy for acute postoperative form of anastomositis after gastrectomy includes:
- systemic administration of antibiotics;
- removal of gastric contents using a probe to avoid stagnation;
- delivery of anti-inflammatory drugs directly to the site of application of the connection using a probe.
Treatment of chronic anastomositis is complex and is carried out in a hospital setting for at least 7-10 days. Treatment options include:
- Systemic anti-inflammatory therapy. The patient is given intravenous or intramuscular injections of glucocorticoid hormones (prednisolone or hydrocortisone). The duration of hormonal therapy is 4–7 days, depending on the severity of the process. Glucocorticoids suppress the immune system, which leads to the subsidence of inflammatory manifestations.
- To relieve spasmodic symptoms and normalize peristalsis, antispasmodics are prescribed: no-shpu, papaverine, buscopan.
- In some cases, low-level laser therapy is performed at the anastomotic area using an endoscope.
- As symptoms progress, the patient is transferred to intravenous nutrition.
Ulcerative defects in the mucous membrane of the gastric anastomosis are treated according to the same principles as peptic ulcers of the stomach and duodenum, carrying out antibacterial therapy and using proton pump blockers ( Rabeprazole , Omeprazole ).
Diet therapy plays an important role in treatment. After removal of the stomach, for the first 3–4 months, patients should eat mechanically gentle foods (mashed, steamed). Then the diet is gradually expanded, trying to make it as nutritious and easily digestible by the body as possible. Fractional nutrition plays an important role - eating 6-8 times a day.
When stenosis forms at the junction of the digestive tract, conservative methods are ineffective and surgery is necessary to restore the patency of the gastrointestinal tract.
Source: https://GastrituNet.online/bolezni-zheludka/terapiya/operativnoe/rez/anastomozit-posle-rezektsii-zheludka-lechenie.html
Life after gastrectomy
It may take from several months to two years for the body to completely “get used” to the absence of a stomach. After surgery you will have to make some changes to your diet:
- From now on, you should forget about three meals a day. You need to eat 6 times a day in small portions.
- You should not drink while eating. There should be at least an hour between meals and liquids.
- Immediately after a gastrectomy, you should not eat foods high in fiber: whole grain bread, pasta, rice, peas, beans, lentils, oats. Their presence in the diet should be increased gradually.
- Some people stop digesting milk sugar, lactose, . After drinking milk, they experience bloating and diarrhea.
- Due to dumping syndrome, you will have to give up sweets.
- Your doctor may recommend taking vitamins D, C, and B12.
The material was prepared by oncologist, endoscopist, chief surgeon of the Medicine 24/7 clinic, Konstantin Yuryevich Ryabov.
If you are looking for a good surgeon in Moscow, contact the specialists of the Medicine 24/7 clinic for help. We employ experienced doctors, and the operating rooms are equipped with modern high-tech equipment. This allows us to successfully perform many complex surgical procedures. Contact us.
Main stages of gastric resection
For any removal option, the intervention goes through three standard stages:
- Mobilization involves cutting the ligaments that secure the organ inside the abdominal cavity and ligating the vessels before cutting them to prepare the gastric section for removal;
- Cutting off the part of the organ planned for removal from the remaining intact area of the gastrointestinal tract;
- Connection of the remaining “healthy” sections with the intestines.
The intervention takes more than one hour, especially with carcinoma, when the greater and lesser omental bursa, tissue and lymph nodes must be removed.
Laparoscopic surgery is longer than in the open abdominal cavity, and technically much more complicated; in fact, this operation is the pinnacle of the professional art of an abdominal oncologist surgeon.