Resection called an operation during which part of an organ is removed. The most common indication for such interventions on the pancreas is malignant neoplasms. Such operations are complex, carry relatively high risks and may not be performed in all clinics.
In this article we will talk about what types of pancreatic resection there are, what complications they can be accompanied by, and what the risks are.
Our expert in this field:
Ryabov Konstantin Yurievich
Chief surgeon, oncologist, endoscopist
Call the doctor
Blitz survey of oncologist-surgeon Konstantin Yurievich Ryabov
How much experience does a surgeon need to have for extended pancreaticoduodenectomy (EPR)? And why?
At least 20 years. How to become a good karateka - 3 years to hit, 3 years to block, 3 years to stand. ... We will add another 3 years for the decline... and almost double it!
Why should you be treated?
The main thing in predicting survival after PDR is the actual standard internationally accepted implementation of the intervention itself with detailed adherence to technique and technology. Exactly the kind that would have been carried out if the patient were in the USA or Germany. The only objectively measurable indicator will be early postoperative mortality, equal to 1%.
Are there any proprietary PDR techniques?
Currently, the author's method of performing PDR for pancreatic cancer is a pointless exercise. Surgical options have been described many times, along with survival prognoses for various types of cancer. You just need to know the algorithms. A bicycle inventor is someone who knows little and does not want to learn.
Why not to the oncology center, not to the EMC, not to JSC Medicine?
I will slightly violate collegial deontology. With all due respect to our colleagues, some due to the scientific nature of the institution, others due to the desire to distinguish themselves among their colleagues, We have a standard international school, based on the total experience of tens of thousands of operations. Such a number of GPDR and PDR have not been completed anywhere.
Why can't surgery for pancreatic cancer be postponed?
The pancreas is located in an area of extremely loose tissue, and at the same time it is abundantly supplied with blood, and there is abundant lymphatic drainage from it. Therefore, pancreatic cancer extremely quickly metastasizes to surrounding tissues, along the blood and lymphatic vessels. Why should it be done first? Without removing the primary lesion, it is almost impossible to suppress tumor growth. Preservation of the primary lesion will reduce patient survival to “0”.
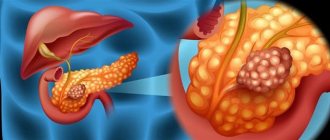
A little about the anatomy of the pancreas
The pancreas is an organ approximately 15 cm long; in appearance it resembles a pear. It has three parts: head, body and tail. The pancreas is located in the upper abdomen behind the stomach. It is located retroperitoneally , that is, it is covered with peritoneum on only one side. The head of the organ is covered by the duodenum.
The pancreas consists of two types of tissue, each of which performs its own functions:
- Exocrine tissue produces juice with enzymes, which flows through the duct into the duodenum and is involved in digestion.
- Endocrine tissue is located in the thickness of the organ in the form of small islands; it produces insulin and some other hormones.
In 95% of cases, malignant pancreatic tumors develop from exocrine cells. The most common are ductal adenocarcinomas .
They are very aggressive, quickly grow into neighboring tissues, and give metastases. It is very difficult to treat them; the only chance of getting rid of cancer is surgical removal of the tumor, if possible.
Pancreatic cancer grades
There are 4 degrees of pancreatic cancer, each of which has its own characteristics and life prognosis:
First degree - the neoplasm has clear boundaries, reaches no more than 2 cm in diameter. It is localized exclusively in the tissues of the pancreas, there are no metastases to other organs of the gastrointestinal tract. Palpation of the left hypochondrium of the abdominal cavity does not cause acute pain. It does not have clearly defined symptoms, so it is diagnosed extremely rarely.
There can be three types:
zero - a small tumor, located strictly within the membranes of those cells from which degeneration began; 1A – the tumor grows through the membrane, forming clearly defined symmetrical contours; 1B – does not spread to other organs, does not have metastases, but there is rapid growth of the tumor.
Second degree - the tumor does not exceed 3 cm in diameter, the circulatory system is affected, and natural blood flow is disrupted. In stage 2A, damage to nearby organs is possible: the duodenum, ducts, but there are no metastases. Stage 2B is characterized by a more aggressive course, as well as damage to the lymphatic system with the formation of metastases.
Third degree - the tumor is actively developing, constantly increasing in size. Its cells and tissues are able to grow into tissues near the underlying gastrointestinal organs, disrupting their functioning. Metastases spread not only to nearby lymph nodes, but can also penetrate the bone marrow. Typically, the third degree is typical for men suffering from alcoholism. Often accompanied by liver cirrhosis and ascites (increased intra-abdominal fluid).
Fourth degree - intoxication of the whole body increases, and a malignant neoplasm can spread to distant organs: kidneys, bladder, genitals. Metastases in the bone marrow literally leave a person no chance of life, and the prognosis in this case is the most unpredictable and unfavorable.
But not only the degree of cancer affects life expectancy. When diagnosing, a histological examination of the tumor itself is also taken into account, which makes it possible to predict its further development. Based on the type of tumor and its structure, the following types of pancreatic cancer are distinguished:
mucinous cystadenocarcinomas; ductal adenocarcinoma; mucinous adenocarcinoma; glandular squamous cell carcinoma.
Gastropancreatoduodenal resection for pancreatic cancer: to do or not to do?
Is it worth having surgery? Will it lead to prolongation of life? Or the diagnosis of pancreatic cancer is a death sentence, and nothing needs to be done. What complications develop after surgery? How much will life expectancy increase after pancreatic surgery?
To do or not to do PDR/GPDR? Why does such a question exist in the minds of patients with pancreatic cancer? Unfortunately, in our country the quality of surgical care for this particular category of patients is low. The degradation of surgical schools in most academic educational institutions in our country leads to high intra- and postoperative mortality, as well as unsatisfactory long-term results of surgery. This very often serves as a basis for treating oncologists to refuse radical interventions for pancreatic cancer. Similar views are held by related doctors - endocrinologists, endoscopists, and simply surgeons. This is compounded by discrepancies in the foreign and domestic scientific press regarding the prognosis of survival of patients with pancreatic cancer after radical surgery.
Why? Diagnosis criteria, classification of pancreatic tumors, and staging differ in Japan, the USA and Western Europe.
The objective reality is this: in the best hospitals in the world, standard pancreaticoduodenectomy gives a 1% mortality rate, that is, out of 100 operated patients, one dies during the operation. In ordinary city hospitals, where surgeons do not have a flow of operations, and actually “train” in large oncology surgery, intraoperative mortality in HDPR can reach 12.5%.
The most difficult data for patients and their relatives to understand are the survival results of patients with pancreatic cancer after radical surgery. On average, from 30 to 70% of patients survive a year after surgery, according to various sources; the average life expectancy after GPDR is, according to domestic data, 12 - 15.5 months; The five-year survival rate even after operations in the world's best centers and combination therapy does not exceed 3.5–15.7%. Therefore, whether to have surgery or not is your choice!
Necessity and contraindications for surgical treatment
The pancreas is closely related to the duodenum and gallbladder, so diseases of these organs of the digestive system can produce similar symptoms. To clarify the source of the problems, differential diagnosis is necessary.
Not all pancreatic diseases require surgery. Some are successfully treated with conservative treatment methods. There are a number of absolute and relative indications for pancreatic surgery.
Surgical treatment requires tumors and cysts that obstruct the outflow of glandular secretions and, in some cases, acute pancreatitis. The following diseases require urgent surgical intervention:
- acute pancreatitis, which is accompanied by necrotization (death) of tissues,
- purulent abscesses,
- injuries complicated by internal bleeding.
Surgery for pancreatitis can also be performed in cases of severe chronic disease, which is accompanied by severe pain.
First of all, they try to eliminate stones in the pancreas using conservative methods, but if the formations are large, then most often the only way to get rid of them is surgery.
In type 2 and type 1 diabetes, surgical intervention may be required in case of serious complications: problems with blood vessels, nephropathy, including progressive ones.
What is the key to successful operations?
So, since you need to undergo pancreaticoduodenectomy for pancreatic cancer, how and where to do it?
Firstly. The NCCN standards determine that gastropancreatoduodenal resection must be performed immediately after the diagnosis of pancreatic cancer, even without histological or cytological verification, but on the basis of PET-CT and magnetic resonance imaging. This requirement is due to the fact that even during laparoscopic intraoperative pancreatic biopsy, the false negative rate exceeds 10%. Unfortunately, this becomes clear only too late, after the disease has reached an inoperable stage. Therefore, we consider it justified to perform PDR surgery after PET-CT and MRI.
Secondly. Pancreatic cancer, due to the specificity of the affected organ, almost immediately affects with micrometastases the entire connective tissue surrounding the pancreas; tumor cells form micrometastases along the neurovascular bundles along the lymphatic vessels, in the nearest lymph nodes, in the para-aortic lymph nodes, in the stacks of the portal and splenic veins. Micrometastases are formed even with small - from 0.4 to 3.5 cm single primary tumor foci of PCa.
That is, in fact, even in the 1st stage of prostate cancer, micrometastases affect the majority of lymph nodes that are not removed using the standard GPDR technique, namely regional and parapancreatic lymph nodes, as well as lymph nodes of the juxtaregional collector.
At the same time, the final decision on the volume of PDR is made intraoperatively, during a visual examination of the abdominal organs, with the exception of distant metastases and local extension of the process. In other cases, the situation is regarded as inoperable (unresectable), since it is believed that tumor infiltration of the retroperitoneal tissue, including the nerve plexus and metastasis of regional lymph nodes, makes the operation technically impossible. Therefore, during the operation, under any circumstances, we try to perform the largest possible volume of resection with resection of regional lymph nodes, as well as in some cases with vascular resection, which actually increases the survival rate of our patients.
In our experience, the best 5-year survival after extended GPDR is observed for small tumors of the head of the pancreas (ductal adenocarcinoma), without visually detectable invasion of mesenteric vessels, lymph nodes of the juxtaregional collector and distant metastases.
Call your doctor now!
Third. In the majority of patients with cancer of the head of the pancreas, metastases were not detected in the lymph nodes around the tail of the pancreas, as well as metastases in the hilum of the spleen and mediastinal tissue. Interestingly, as a rule, no tumor lesion is detected in the distal direction along the pancreatic duct.
Therefore, it is important to take into account the nature of the lesion in the scope of the operation. Ideally, the histological variant of the tumor is also included, since it is this that determines the survival of patients. Thus, standard PDR for ductal adenocarcinoma of the head of the pancreas gives ideal short-term results (intra- and postoperative mortality 0-5%), unsatisfactory long-term results (median life expectancy after surgery 10-18 months, no 5-year survival). At the same time, surgery for cystadenocarcinoma of the head of the pancreas gives a 5-year survival rate of up to 60-78%. Therefore, we do not use the classic Whipple operation, proposed at the beginning of the 20th century, but its various variations with partial preservation of some organs, if possible.
Fourthly. Since the “Medicine 24/7” clinic performs an extended GPDR, we most often resect the head and body of the pancreas, the pyloric part of the stomach together with the lesser omentum and the right half of the greater omentum, the duodenum, the gallbladder, the distal part of the common hepatic duct and the entire common bile duct. The tissues removed as a single complex include adjacent connective tissue, lymphatic vessels and nodes, nerve plexuses, fascial-cellular sheaths of all large vessels in the area of surgery. In addition, if there is suspicion of tumor invasion of the superior mesenteric vein or portal vein, the latter are resected. In addition, skeletonization of all large arteries and veins is carried out.
Fifthly. Our own data and the data of Japanese and American colleagues indicate that a real 5-year survival rate of more than 15%, and in the limit, for neuroendocrine tumors, 85% is achieved with the most extended GPDR, followed by a thorough histological examination of the entire surgical complex, in which no , or single metastases were detected in the lymph nodes of the juxtaregional collector. However, the large volume of surgery faces another problem - the tolerability of the extended GPDR. The wider the scope of the GPDR, the higher the incidence of complications - postoperative diarrhea, failure of pancreaticojejunostomy. Surprisingly, diarrhea that lasts several months after surgery indirectly indicates the extent of the operation and predicts a positive long-term outcome of extended GPDR.
At sixth. In Russia, since standard GPDR is most often performed for exocrine prostate cancer, most patients die in the first year after surgery, regardless of the extent of the tumor process; only a few patients survive 3 years. It is important to know that the data given in most even scientific works are based on so-called life tables, which overestimate the five-year survival rate compared to direct data by almost four times; We, having experience in monitoring hundreds of patients since 1996, use only direct observational data. The vast majority of patients die from progression of pancreatic cancer due to the development of local relapses without liver metastases after standard GPDR.
That is why in 2008, for the first time in Russia, my research group performed extirpation of the pancreatic stump in case of relapse of pancreatic cancer after a previously performed pancreatoduodenal resection (included in the register of operations in Germany). This intervention allows patients to live for another 12-24 months, even with recurrent prostate cancer.
Patient age
The older a person is, the greater the chance that he has problems with the pancreas. This is directly related to an unhealthy lifestyle, as well as the following unfavorable factors:
alcoholism; obesity due to poor nutrition; low quality of consumed water; abuse of sweet carbonated drinks.
The risk group most often includes men aged 25 to 55 years. The insidiousness of the disease is that it does not make itself felt in the early stages. Typically, oncology is diagnosed when the patient experiences acute abdominal pain, deterioration in general condition, and indigestion, which is typical for stages 2-3. Pancreatic cancer in the early stages is detected in only 5-7% of all patients during a routine examination.
In most cases, cancer is detected at stages 3-4, when the patient has obvious symptoms of gastrointestinal diseases:
indigestion and abdominal pain after eating; yellowness of the skin; increase in abdominal volume; sudden weight loss; complete lack of appetite; toxicosis.
In addition to age, life expectancy can also be influenced by factors such as:
The location of the tumor determines the possibility or impossibility of surgery. Pancreatic cancer can have three levels of location: head, tail, and degeneration of the whole body. The provoking factor determines the cause of the formation of the tumor. There can be three types: gastrinoma, insulinoma, glucagonoma. Tumor histology - helps to evaluate its structure, composition and shape, as well as the rate of degeneration.
Main types of operations for pancreatic cancer
In clinical practice, the main radical operations for prostate cancer are distinguished, including standard PDR (Whipple operation), gastropancreaticoduodenectomy, extended GPDR, pancreatectomy, distal combined resection of the pancreas, extended total pancreaticoduodenectomy. All these operations are extremely complex technically, since the requirements for the surgeon’s qualifications include the ability not only to determine the volume of resection during the operation and perform it, but also to carry out a series of restorative manipulations in a certain sequence - pancreaticojejunostomy, biliodigestive anastomosis, gastrojejunostomy and interintestinal anastomosis. That is why the team usually consists of 4-5 surgeons, and the average duration of the operation is about 6-8 hours.
Whipple operation (pancreaticoduodenectomy)
Pancreaticoduodenectomy is the most common operation for pancreatic cancer that develops from exocrine cells. The surgeon removes the head of the pancreas (sometimes along with the body), part of the small intestine, bile duct, gallbladder, regional lymph nodes, and sometimes part of the stomach. Such a large volume of intervention helps with the maximum probability of removing all tumor tissue and reducing the risk of relapse.
The remaining parts of the intestines and stomach are connected, the pancreas and the remaining part of the bile duct are sutured to the small intestine. Thus, after the operation, bile and digestive juice continue to flow into the intestine.
Classically, the Whipple procedure is performed through a large incision that runs down the middle of the abdomen. But in some clinics, the equipment and skills of doctors allow the intervention to be performed laparoscopically.
Get a consultation with a doctor
Pancreaticoduodenectomy is a complex operation. Success and risks are highly dependent on the experience of the doctor. If few such interventions are performed in the clinic, and doctors do not have sufficient experience, complications kill about 15% of patients. But even if the operation is performed by experienced doctors, the mortality rate reaches 5%.
Main complications after Whipple surgery:
- Bleeding,
- Failure of intestinal sutures,
- Infections.
- Indigestion. Many patients have to follow a diet and take pancreatic enzyme medications,
- Stool disorders
- Weight loss,
- Diabetes mellitus - if a lot of endocrine tissue has been removed.
The Whipple operation gradually fell out of use in most European countries after publications, first by Japanese and then by American and European authors, on the analysis of the life expectancy of patients whose life expectancy after the operation did not exceed the life expectancy after chemoradiation treatment.
The reason for this turned out to be the presence of micrometastases and small metastases in regional lymph nodes along the upper edge of the body of the pancreas, in the lymph nodes around the mesenteric vessels, in the lymph nodes around the hepatic ducts, which are not removed using the standard Whipple surgery technique. The only indication currently, according to international protocols, for Whipple surgery for pancreatic cancer is cancer of the major duodenal papilla, which metastasizes mainly to 1-2 groups of lymph nodes directly adjacent to the head of the pancreas.
It is for this reason that scientific groups in the USA and Japan, in parallel, to replace the standard PDR in patients with cancer of the head of the pancreas, developed methods of extended GPDR. At the same time, it was possible to reduce postoperative mortality from 32 to 8%, and then to 5%. Then they achieved an increase in life expectancy after surgery, on average up to 3 years, and a reduction in the number of local and regional relapses to 15%, with a total long-term three-year survival rate of about 35-45%, and a five-year survival rate of 25-30%.
Extended gastropancreaticoduodenectomy
Extended gastropancreatoduodenal resection (extended GPDR) is an operation, the essence of which is the simultaneous removal of a complex of organs, including the head of the pancreas, lower stomach, duodenum, incoming part of the small intestine, gallbladder, partially bile ducts and adjacent lymph nodes. In addition, extended pancreatoduodenal resection involves the removal of a segment of the portal vein and arteries involved in the tumor process with reconstruction of the vessels. The retroperitoneal lymph nodes are also removed from the celiac artery to the bifurcation of the iliac arteries.
In case of unresectable prostate cancer, including the presence or threat of obstructive jaundice, gastrointestinal obstruction, and with the patient's life expectancy exceeding 6–7 months, palliative interventions are performed, including the application of biliodigestive and gastrojejunal anastomoses.
In case of expected life expectancy of more than 1-2 months. We prefer to place stents in the bile ducts either by percutaneous transhepatic drainage and stenting, or during the RCCP procedure - retrograde cholangiopancreaticoduodenography. The stenting procedure improves the quality of life of patients and increases life expectancy.
Distal pancreatectomy
During this operation, the tail and part of the body of the pancreas, and often the spleen, are removed. Distal resection is usually used for neuroendocrine tumors that originate from endocrine cells. At the time of detection, exocrine cancer of the body and tail most often has time to spread widely in the body, grows into neighboring organs, and gives metastases.
In addition to other possible complications, removal of the spleen during distal pancreatectomy leads to a decrease in the body's defenses. A person becomes more vulnerable to infections.
Pancreatectomy is a method of removing the pancreas
Pancreatectomy is the removal of the pancreas. It is carried out in case of severe life-threatening pathology, when all possible methods of conservative therapy have failed. In such cases, the following types of resection are performed:
- total - the gland is completely removed along with the organs adjacent to it (spleen, part of the stomach and small intestine, gall bladder),
- partial - as a result of surgical treatment, only the head or tail has to be removed.
The operation is schematically carried out according to the following algorithm: an incision is made in the projection of the pancreas, part or all of which, together with the damaged adjacent neighboring digestive organs, is removed, the incision is sutured and secured with knots or staples. Surgical treatment is dangerous due to the increased complexity of manipulations, trauma and frequent deaths.
After a successful operation, complications may arise. Their development is influenced by:
- obesity,
- age,
- concomitant diseases,
- unhealthy diet
- smoking.
The recovery period is long: it takes many months, sometimes a year. From the first days, an unpleasant sensation may appear, and there will be constant pain in the left hypochondrium throughout the entire rehabilitation. Any asthenic symptom (decreased appetite, severe weakness) also occurs, and food allergies develop.
Reviews from our patients
- Mammary cancer. Full recovery
Mammary cancer. Full recovery February 19, 2021Here is a case of complete recovery from breast cancer. Two weeks ago, a patient came to us with a complaint of a tumor in the right mammary gland. A biopsy was performed. Based on its results, cancer was diagnosed. The tumor is highly differentiated, susceptible to the influence of hormones. A surgical operation for resection of the mammary gland was performed. The breast is preserved. According to the results of histological examination, the surgical intervention was carried out radically, the resection margins were clean. To prevent…
read more
- Treatment at the Medicine clinic 24/7. Patient review
Treatment at the Medicine clinic 24/7. Patient review February 16, 2021
The patient underwent examination and chemotherapy treatment. He notes: “I would like, first of all, to express my gratitude. Secondly, the impression of the clinic and the attending physician as the highest professionals. Extreme level of competence, efficiency, organization and interconnectedness of decision making. All this leads to a positive result. Therefore, I want to express my gratitude to all of you for all this. I didn’t even expect that such a level of service in medicine was possible......
read more
- Preparing for chemotherapy: Increasing hemoglobin levels
Preparing for chemotherapy: Increasing hemoglobin levels February 11, 2021
The patient was admitted to the clinic with a low hemoglobin level. This factor interferes with chemotherapy. In other medical institutions it may be a reason for refusal of treatment. In such situations, specialists at the Medicine 24/7 clinic carry out a set of measures aimed at increasing hemoglobin levels. We have a similar case before us. During hospitalization, blood counts returned to normal. The patient was discharged with improved health.
read more
- Treatment of pleurisy: patient review
Treatment of pleurisy: patient review February 11, 2021
The patient came to the Medicine 24/7 clinic due to pleurisy, which acutely arose against the background of the underlying disease. Treatment was carried out promptly. Fluid from the pleural cavity was evacuated. Specific treatment of the underlying disease was started. The patient thanks her attending physician for the assistance provided. She notes his attentiveness and kindness.
read more
- Photodynamic therapy: patient review
Carrying out photodynamic therapy: patient review February 10, 2021
The patient applied to the Medicine 24/7 clinic for treatment of skin basal cell carcinoma. Treatment was prescribed in the amount of photodynamic therapy. A positive result has been achieved. During a comprehensive examination, kidney disease was revealed. Treatment tactics have been developed. Patient o.
read more
- Chemotherapy: patient review
Chemotherapy: patient review February 10, 2021
The patient was hospitalized for a second course of chemotherapy. Her condition remained serious. During hospitalization, the patient was prepared for treatment. A course of antibacterial therapy was carried out. Bilateral pneumonia was stopped, as well as bleeding. The patient successfully completed the second course of chemotherapy. The treatment prognosis is favorable.
read more
- Treatment of stage 3 ovarian cancer with peritoneal carcinomatosis
Treatment of stage 3 ovarian cancer with peritoneal carcinomatosis February 5, 2021
The patient came to the clinic due to stage 3 ovarian disease. A comprehensive examination was carried out. The diagnosis is confirmed. The situation was discussed at a medical council, the decision of which proposed cytoreductive surgery and the HIPEC procedure. The surgery was successful. On the seventh day after surgery, the patient was discharged home in satisfactory condition. In the future, it is planned to conduct six courses of chemotherapy, the goal of which is to avoid relapse.
read more
Is pancreas surgery life-threatening?
Diseases of the pancreas occur with progression. In many cases, the prognosis is unfavorable for life: if the diagnosis, treatment is delayed, or the condition is severe, death can occur. It is necessary to carry out surgical intervention as early as possible for existing indications.
Surgery is a complex and lengthy procedure and, according to statistics, is accompanied by a high mortality rate. But this does not mean that surgery is dangerous. The pathology of the pancreas is so severe that if there are indications for surgery to preserve life and health, it is impossible to refuse radical treatment. Already in the process of surgical manipulations, it is possible to predict the patient’s further condition and the occurrence of complications.
Typical history of patients with pancreatic cancer.
The patient first applied to a regional clinical hospital in one of the regions of Russia at the end of 2021 with complaints of yellowness of the eyes and skin. Obstructive jaundice was diagnosed, caused by a volumetric process in the area of the gallbladder.
An operation aimed at correcting obstructive jaundice was performed - cholecystoenteroanastomosis was formed; In addition, during the examination of the abdominal organs, the condition was assessed as a tumor of the head of the pancreas. Due to the large volume of tissue involved, the tumor was considered inoperable.
The patient went to the Blokhin Russian Cancer Research Center on his own, where computed tomography and endoscopic ultrasound with puncture of the head of the pancreas were performed. Based on histology results, a diagnosis of adenocarcinoma of the head of the pancreas was made. The detailed clinical diagnosis is formulated as “Cancer of the head of the pancreas T3N1M0”. Due to tumor involvement of the superior mesenteric vein, surgery was refused and 3 cycles of chemotherapy according to the GEMOX regimen were recommended. The patient independently contacted us after completing 3 cycles of chemotherapy.
A control examination was performed, including PET-CT, CT with contrast: changes in the primary lesion within the measurement error, regression of regional metastases. It is recommended to perform an extended GPDR. The operation was performed before the New Year 2021. Using intraoperative histological examination, the diagnosis of ductal adenocarcinoma was confirmed.
Postoperative histological and immunohistochemical studies confirmed the diagnosis. The duration of the operation was 6.5 hours. The scope of resection is maximum, with “skeletonization” of the main veins, as well as resection of the affected area of the superior mesenteric vein with the imposition of a vascular anastomosis. The volume of blood loss is 900 ml.
The early postoperative period was uneventful - on the 7th day the patient was transferred to the ward. Discharge from the hospital was made on the 21st day. As of mid-2021, the patient is under our dynamic observation.
Get your treatment protocol today
Possible complications
An operation aimed at removing the pancreas is a threat to the health and life of the patient. The occurrence of complications is facilitated by: poor general condition, cachexia, progressive cancer, unsanitary conditions, obesity, diabetes mellitus, additional diseases (heart, liver, lungs).
The anatomy of the abdominal organs is different for each person. Therefore, despite the efforts of doctors during surgical treatment, sometimes technical difficulties arise that can lead to complications.
These include: damage to neighboring organs (for example, the spleen and liver), as well as nerves and blood vessels (the risk of their damage increases with significant obesity, with various anatomical abnormalities in patients who have undergone other operations).
On this topic
- Oncogastroenterology
What kind of pain occurs with rectal cancer?
- Olga Vladimirovna Khazova
- December 3, 2021
Complications of pancreatic resection directly related to the procedure in the early and late period include:
- impaired emptying , leading to nausea and vomiting;
- infection of a postoperative wound due to infection;
- suture rupture as a result of healing complications, impaired blood supply or mechanical stress;
- inflammation of the pancreatic stump;
- inflammation of the bile ducts;
- disruption of blood supply as a result of closure or damage to blood vessels;
- bleeding in the gastrointestinal tract;
- adhesions in the abdominal cavity, which even after many years can lead to intestinal obstruction.
Non-insulin-dependent diabetes mellitus develops when the remnant pancreas is unable to provide enough insulin. This complication is associated with the need to use insulin for the rest of life.
Most of these complications may require subsequent operations, changes in the method of treatment, its prolongation, and can also cause death.
Is it possible to perform liver and pancreas resection at the same time?
Combined liver and pancreatectomy is an even more complex operation, but it can be performed in some patients. The very fact that part of the liver and pancreas needs to be removed at the same time is not a contraindication to surgery. Such interventions are accompanied by high, but not prohibitive, risks, and some patients may well tolerate them.
For example, in one 2009 research study, the authors describe follow-up of 40 patients aged 39–69 years who underwent combined liver and pancreatectomy for different types of cancer: cholangiocarcinomas, neuroendocrine tumors, gallbladder carcinoma, gastrointestinal stromal tumors, colorectal cancer, metastatic melanoma eyes. None of the patients died shortly after the operations. Five-year survival rates turned out to be quite good.
Of course, such interventions can be performed successfully and with minimal risks only in specialized clinics, where doctors perform more than one similar operation every year and have extensive experience.
The material was prepared by oncologist, endoscopist, chief surgeon of the Medicine 24/7 clinic, Konstantin Yuryevich Ryabov.
Experienced surgeons of various specialties work at the Medicine 24/7 clinic; our operating rooms are equipped with modern high-tech equipment. This allows us to perform many complex interventions. Contact us to find out more.
Nutrition after surgery
After removal of the pancreas, special attention is paid to nutrition. On the third day you are allowed to drink sweetish weak tea and still mineral water. On days 4-6 add liquid vegetable soups and liquid porridges. Only towards the end of the first week do they begin to gradually add coarser food - bread, omelet, stewed vegetables. Two weeks after the operation, cottage cheese with a reduced percentage of fat content, lean types of meat and fish are allowed.
Dishes must be subjected to heat treatment. The diet does not contain fresh vegetables and fruits, baked goods, coffee, spicy and smoked foods, or canned products. Alcohol and smoking are unquestionably prohibited.
All portions are palm sized. You should eat frequently. Don’t forget about herbal medicine and vitamin-mineral complexes. These principles are followed for life.
To avoid serious complications and any type of surgery, you need to take care of yourself. It is better to prevent a disease than to treat it later.
Postoperative period
After removal of the pancreas, the patient is sent to a separate ward. There he will be observed by a doctor during the rehabilitation period. On average, this time lasts 5-20 days. If unforeseen circumstances suddenly arise, this period is extended at the discretion of the attending physician.
Some patients experience pain after the anesthesia wears off. In this case, painkillers are prescribed.
When a person is discharged from the hospital, the doctor explains in advance what rules will have to be followed for some time. This includes the following recommendations:
- compliance with a certain dietary table;
- taking enzymes;
- insulin administration;
- Physical activity and heavy lifting are prohibited.
Important information: Where is the pancreas located in humans and how does it hurt?
The help of loved ones is especially important for the patient, since for some time he will not be able to cope with all matters on his own.
Rehabilitation of the patient
The recovery time after pancreatic surgery may vary. They depend on the pathology, the volume of radical intervention performed, concomitant diseases and lifestyle. If surgical treatment was caused by extensive pancreatic necrosis or cancer of the pancreas and partial or total resection of the pancreas and neighboring organs was performed, then it will take many months, some – a year, to restore the body. And after this period you will have to live in a gentle regime, adhering to a strict diet, constantly taking prescribed medications.
At home, a person feels constant weakness, fatigue, and lethargy. This is a normal condition after major surgery. It is important to follow a routine and find a balance between activity and rest.
During the first 2 weeks after discharge, complete rest (physical and psycho-emotional), diet and drug treatment are prescribed. A gentle regime implies an afternoon nap, the absence of stress and psychological stress. Reading, household chores, and watching television should not increase the feeling of fatigue.
You can go outside in about 2 weeks. It is recommended to take walks in the fresh air at a calm pace, gradually increasing their duration. Physical activity improves well-being, strengthens the heart and blood vessels, and increases appetite.
It will be possible to close the certificate of incapacity for work and return to professional activity in about 3 months. But this is not an absolute period - it all depends on the state of health and clinical and laboratory parameters. In some patients this happens earlier. After severe operations due to loss of ability to work, many are assigned a disability group for a year. During this time, the patient lives, adheres to a diet, routine, takes prescribed drug therapy, and undergoes physiotherapeutic procedures. A gastroenterologist or therapist observes the patient, monitors laboratory parameters of blood and urine, and adjusts treatment. The patient also visits a specialist in connection with endocrine pathology: after large-scale operations on the pancreas, diabetes mellitus develops. How well he will live this time depends on strict adherence to the advice of doctors.
After a set period of time, the patient again undergoes the MSEC (medical and social expert commission), at which the issue of the possibility of returning to work is decided. Even after restoration of physical condition and social status, many people will need to use medications for life and limit themselves in food.
Postoperative treatment
Therapeutic tactics are developed by the doctor after studying examination data before and after surgery, taking into account the patient’s condition. Despite the fact that a person’s health and general well-being depend on the chosen method of surgical treatment and the quality of rehabilitation measures, mortality after surgery remains high. Choosing the right treatment strategy is important not only for normalizing vital signs, but also for preventing relapses of the disease and achieving stable remission.
While still in the hospital, the patient is prescribed replacement therapy in the form of enzymes and insulin, and the dose and frequency of administration are calculated. Subsequently, the gastroenterologist and endocrinologist adjust the therapy. In most cases, this is lifelong treatment.
At the same time, the patient takes a number of drugs from different groups:
- antispasmodics and analgesics (if pain is present),
- PPIs – proton pump inhibitors,
- hepatoprotectors (for liver dysfunction),
- affecting flatulence,
- normalizing stool,
- multivitamins and microelements,
- sedatives, antidepressants.
All medications are prescribed by a doctor, who also changes the dosage.
A prerequisite for normalizing the condition is lifestyle modification: giving up alcohol and other addictions (smoking).
Diet
Dietary nutrition is one of the important components of complex treatment. The further prognosis depends on strict adherence to the diet: even a slight violation of nutrition can cause a severe relapse. Therefore, food restrictions, refusal to drink alcoholic beverages and smoking are a prerequisite for the onset of remission.
After discharge from the hospital, the diet corresponds to table No. 5P according to Pevzner, the first option, pureed (2 months), upon the onset of remission it changes to No. 5P, second option, unmashed (6-12 months). In the future, it is possible to assign table No. 1 in different modifications.
To recover from surgery, you will have to observe strict dietary restrictions for six months. In the future, the diet expands, changes occur in the diet, and new products are gradually introduced. Proper nutrition:
- frequent and fractional - in small portions 6-8 times a day (later adjusted: the frequency of meals is reduced to 3 times with snacks 2 times a day),
- warm,
- pureed to a puree-like consistency,
- steamed or by boiling and stewing.
At all stages of the disease, including remission, fatty, fried, spicy, smoked foods are prohibited. To compile the menu, special tables are used indicating a list of permitted and prohibited foods and their calorie content.
Any changes in diet should be agreed with your doctor. The diet after pancreatic surgery must be followed throughout life.
Physiotherapy
Therapeutic exercise (physical therapy) is an important stage in the restoration of the body. Prescribed when complete remission is achieved. In the acute period and after surgery, any physical activity is strictly prohibited for 2-3 weeks. Exercise therapy improves the general condition of a person, his physical and mental status, affects the normalization of the functions of not only the pancreas, but also the other digestive organs, improves appetite, normalizes stool, reduces flatulence, and removes stagnation of bile in the ducts.
2 weeks after discharge, walking is allowed, later the doctor prescribes a special set of exercises and self-massage for the pancreas and other digestive organs. In combination with morning exercises and breathing exercises, this stimulates digestion, strengthens the body, and prolongs remission.
Rehabilitation process after pancreatectomy
Living after removal of the pancreas and spleen, especially at first, is difficult. There is constant pain at the site of scarring of the sutures and a feeling of hunger: in the first few days, eating is prohibited, in the subsequent period you have to follow a strict diet. The doctor will determine how long it will last.
To prevent complications, a course of therapy is carried out:
- antibacterial,
- anti-inflammatory,
- insulin therapy.
A long, sometimes lifelong, course of enzyme preparations is prescribed. The name, dosage and duration of administration are prescribed by the doctor, taking into account the scope of the operation and the patient’s condition. If a resection of the head or tail of the gland is performed, the remaining part will eventually take on some of the functions. With total removal, problems arise with replacement therapy and nutrition.
Mode sequence:
- For 2–3 days the patient observes strict bed rest and fasting. Only drinking is allowed.
- After 3 days you are allowed to sit down, then get out of bed and take short walks with support. Walking and movement are necessary at an early stage to prevent the formation of adhesions in the abdominal cavity.
- After 8–10 days, the wound heals, the sutures are removed, and the patient is discharged from the hospital. Depending on the volume of gland tissue removed and the size of the operation performed, the patient may remain on sick leave for another 10–20 days, after which he is discharged to work.
Diet after pancreas removal
After surgery to remove the pancreas, a person lives on a diet for the rest of his life. To exist, you need to make diet a way of life. The essential principles of nutrition are adherence to:
- multiplicity,
- details,
- eating only permitted or permissible food and categorically refusing prohibited foods (you must be able to use a special table indicating calorie content and lists of permitted foods to draw up the correct menu and calculate its calorie value).
After surgery it is important:
- high protein content in food (it is involved in the restoration of cell membranes and tissue healing),
- restriction of carbohydrates (due to impaired endocrine function of the pancreas associated with insulin production),
- prohibition of fats (during the recovery process, minor consumption of butter and vegetable oil is allowed).
Fried, spicy, pickled and salty foods are prohibited.