Biliary-dependent pancreatitis after removal of the gallbladder filled with stone-like sediments begins to develop in 70-80% of cases. Many people attribute this phenomenon to the fact that the gallbladder is closely connected to the pancreas and cholecystectomy contributes to an increase in the load on the pancreas and the development of a chronic form of pancreatitis. But this statement is fundamentally incorrect, since these two organs of the digestive system are complementary, but not interchangeable, and the development of pancreatitis is often a consequence of the progressive stage of cholecystitis, accompanied by an acute inflammatory process against the background of the loss of stone-like, insoluble formations in the cavity of the gallbladder. Chronic pancreatitis with the gallbladder removed, in most cases, acquires longer periods of remission, and the patient after the intervention notes a noticeable improvement in overall health. But, sometimes another postoperative clinic can be observed, when the bile ducts begin to take over all the work of the gallbladder, which leads to a gradual level of entry of bile into the intestinal cavity, disruption of digestive processes, the development of diarrhea or constipation, which in turn can cause acute biliary pancreatitis.
In this review, we will take a closer look at why, after removal of the gallbladder, the pancreas hurts and pancreatic pathology develops, and how pancreatitis is treated after surgery to remove the gallbladder.
Gallbladder removal
Despite the fact that currently there is an active development of various methods of treating cholelithiasis without surgery, most specialists trust the cholecystectomy method. It is a radical solution to the problem when a huge number of insoluble stones or one huge stone accumulates in the bladder cavity, and removal of this organ can not only improve the patient’s health, but also save his life.
The accumulation of a large number of stones in the cavity of the gallbladder contributes to disruption of the functioning of this organ and bile ducts, and also provokes the development of organic dysfunctions near the located organs. This problem must be solved only in radical ways, therefore, in most cases, cholecystectomy is the only correct solution. The affected organ is removed through a 12-mm laparoscopic incision, into which the laparoscope itself is inserted and the gallbladder is removed.
This method of surgery will allow the patient to recover as quickly as possible after the operation and spend a minimum amount of time in the hospital.
Also, do not forget about possible complications that appear after removal of the gallbladder, the main of which will be discussed below.
Postcholecystectomy syndrome and adhesions
The development of postcholecystectomy syndrome is a dependent pathology that occurs against the background of disruption of bile circulation processes due to poor diet and consumption of alcoholic beverages.
This disease manifests itself with the following symptoms:
- the appearance of pain in the right side, abdomen and gastric cavity,
- development of flatulence,
- the appearance of a feeling of heartburn,
- rise in body temperature to subfebrile limits,
- development of diarrhea,
- the appearance of constipation, which contributes to the formation of hemorrhoids,
- feeling of nausea and vomiting,
- the appearance of belching with a bitter aftertaste,
- yellowness of the skin and sclera.
Symptomatic signs may not appear in every case, but the main characteristic of postcholecystectomy syndrome is the development of flatulence and painful symptoms. What to do in such situations?
To eliminate this pathology, immediately after the first painful sensations, it is necessary to seek qualified medical care and prescribe appropriate treatment, which consists of the use of enzymatic agents, as well as antispasmodic drugs with a choleretic effect. In some cases, repeated surgery may be prescribed to correct the changes that have occurred.
In order to prevent the development of such a complication, after cholecystectomy it is necessary to follow the diet prescribed by the doctor, completely eliminate the consumption of fatty foods and alcohol, and also adhere to other methods of maintaining the body prescribed by the specialist.
Another type of complication is the formation of adhesions, which occur in 30-35% of cases after surgery to remove the gallbladder. Adhesions are formations of connective tissue, with the help of which the patient’s body provides itself with protection in the place where the surgical intervention was localized. These formations begin to appear even after minimally invasive surgical treatment.
After the gallbladder is removed, a void appears in its place, which the patient’s body begins to fill with connective tissues. Symptoms of adhesions:
- tingling in the abdominal area,
- as well as the appearance of painful sensations radiating to the abdomen or right side.
It is very important to promptly prevent the development of such formations. After a minimally invasive operation, the patient can take a sitting position, and then get up after a couple of hours and move; lying down for a long time is not recommended. Performing movements helps to activate the intensive performance of the body and the processes of its restoration, therefore, the formation of adhesions in this case will not occur.
You will not be able to remove adhesions on your own; here, even the medicinal recipes of traditional healers using various medicinal herbs, which can only lead to the development of individual intolerance to the medications taken, will be powerless. To prevent the development of disability, treatment of diseased adhesive formations should be carried out only under the clear guidance of the attending physician.
Purpose of cholecystectomy and methods of its implementation
When choosing a diet for patients who have undergone removal of the gallbladder, it is necessary to take into account that after this operation the liver, bile ducts, pancreas and intestines are most often involved in the pathological process.
For hepatitis, diet No. 5 is prescribed, enriched with foods containing lipotropic substances. These include cottage cheese, cod, pike perch, buckwheat and oatmeal, egg white, and yeast drink.
When pancreatitis occurs, the protein content in the diet of patients is increased to 120-140 g, the amount of fat is reduced to 40-50 g, foods that increase bloating (potatoes, bread, legumes, cabbage), fatty, spicy and canned foods are excluded.
For biliary dyskinesia and constipation, a diet is prescribed that stimulates bile secretion and bowel movements. Products containing magnesium salts and plant fiber (fruits, vegetables, wheat and bran bread, bran decoction, buckwheat, etc.) are introduced into the diet.
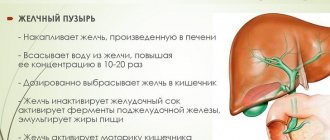
The functions performed by the organ include the accumulation and removal of bile, which is intended for processing fats contained in food.
Among the tasks performed by the pancreas are:
- production of enzymes that ensure food digestion;
- production of glucagon and insulin, which maintain normal blood glucose levels.
The presence of insoluble stones in the diseased organ:
- provokes inflammation of the pancreas;
- causes the reflux of bile into the pancreatic ducts, leading to various forms of pancreatitis and necrotization of its tissues due to self-digestion under the action of enzymes.
Experts identify such pathologies that cause biliary pancreatitis as:
- Cholangitis. Occurs when the bile ducts become inflamed due to obstruction of the ducts due to infection.
- Gallstone disease. Stagnation of bile, which occurs when the channels are blocked by stones, provokes an increase in pressure inside the organ. The consequence of this is the reflux of fluid into the pancreas.
- Cholecystitis. It manifests itself in the form of edema, which disrupts the circulation of bile and occurs with the development of inflammatory processes in the bladder area.
Symptoms of this form of inflammation are:
- Systematic severe aching pain that occurs in the back, lower abdomen and under the ribs. It usually appears within a few hours after eating smoked, canned, fried or high-fat foods.
- Painful sensations of varying degrees of intensity, manifested in the upper part of the abdominal cavity.
- General weakness of the body.
- Frequent gastrointestinal disorders with stool disorders in the form of constipation or diarrhea with a slight increase in body temperature.
- Respiratory system dysfunction.
- The appearance of nausea and vomiting, which is accompanied by a feeling of bitterness in the mouth.
- Fever.
The development of pathology leads to:
- release of enzymes into the blood and surrounding tissues;
- slowing down the digestion process with the simultaneous appearance of painful sensations;
- dysfunction of the pancreas;
- increased frequency of attacks;
- increasing the risk of developing insulin-dependent diabetes mellitus.
Before performing a cholecystectomy, the doctor must make sure that there is no other way to solve the problem. Before this, when symptoms of chronic biliary pancreatitis appear, depending on the severity of the pathology, the gastroenterologist may prescribe one of the following treatment methods:
- A strict diet as an element of symptomatic therapy involves not only fasting for several days, but also a significant reduction in fluid intake, since its entry into the body causes the production of enzymes and deterioration of the condition.
Important! In order to normalize the digestion process and reduce the activity of the pancreas, drugs from the group of enzymes, for example, Pancreatin, can be used. - Intravenous or intramuscular administration of painkillers, for example, Baralgin.
- Antibiotics can be used to stop inflammatory processes and degenerative changes in the pancreas. However, this measure is used in rare cases, when drugs from the group of antispasmodics and analgesics are insufficiently effective.
- Intramuscular administration of antispasmodic drugs, for example, Papaverine, is aimed at reducing the production of gastric juice, which stimulates the activity of the pancreas.
Important! If, despite following a strict diet, the exacerbation episode lasts more than 1 week, intravenous nutrition is a possible solution. - When treating chronic pancreatitis in a hospital setting, one of the mandatory elements of treatment is replenishing the water balance in the body. Its violation occurs due to limiting the amount of fluid consumed. This measure is usually performed by intravenous administration of saline solution.
When an acute form of pancreatitis is determined and symptoms of an “acute abdomen” are detected based on the diagnostic results, the attending physician decides to remove the organ. Another indication is the presence of a large number of stones causing dysfunction of the pancreas and neighboring organs.
Cholecystectomy can be performed using one of two methods, involving removal of stones or removal of the pancreas itself, performed through a small incision:
- laparoscopic;
- laparotopically.
Methods of performing cholecystectomy a) minimally invasive closed type; b) open type
Treatment of pancreatitis after removal of the gallbladder, depending on the patient’s condition, includes a set of measures, the main of which is following a diet during the period of exacerbation of the disease and after its completion.
A comprehensive approach to relief may include the use of one or more drug treatments, including:
- Following a diet that includes pureed soups and pureed vegetables.
As a drink, it is permissible to use weak green tea, fresh juice diluted with water in a 50/50 ratio, and weak rosehip-based decoctions. The patient's menu should include the consumption of fats of vegetable origin and dairy, as they promote the excretion of bile. Over time, you can include low-fat sea fish, chicken and beef dishes in your menu. The main purpose of such a diet is to eliminate the collection of bile in the area of the ducts. One of the principles of such a diet is to eat in small portions, increasing the number of meals to 5-6 per day. Note! It is not recommended to eat freshly baked bread; adding bran and other high-fiber foods to the diet has a good effect on the course of the disease. - In accordance with the testimony of the attending physician, in some cases, after the operation, a 3-day course of therapy using antibiotics is prescribed.
- To relieve pain, it is practiced to prescribe drugs from the group of antispasmodics and analgesics, for example, Buscopan and Drotaverine.
- In some cases, in order to alleviate the patient’s condition and improve digestive processes, drugs of the enzymatic group are prescribed.
- In order to prevent the formation of stones in the bile ducts, drugs containing substances that interfere with this process are used, for example, Ursofalk.
- As a preventive measure to prevent the occurrence of pancreatitis and other pathologies, after cholecystectomy, medications that help normalize the intestinal microflora and choleretic medications are prescribed.
The key to successful treatment after surgery is following the recommended diet and contacting a gastroenterologist at the first signs of deterioration in health.
- How gallbladder dyskinesia affects the pancreas: the hidden danger of pathology
If you liked the material: rate it and share with friends
| (1 votes, average: 5.00 out of 5) Loading… |
This operation is also prescribed for polyps larger than 10 millimeters and other pathologies that are fraught with serious complications. Despite the fact that conservative methods of treating this pathology are currently being actively developed, unfortunately, cholecystectomy is often the only effective method of treating this disease. In many cases, such surgery helps save the patient's life.
Cholecystectomy for cholelithiasis is indicated if there are a large number of calculi (in common parlance - stones) in the bladder cavity or if their size threatens to block the bile duct. In addition, the development of this disease can negatively affect the functioning of other organs of the digestive system, and this is also an indication for bladder resection.
If gallstone disease occurs against the background of concomitant pathology (for example, pancreatitis - a disease of the pancreas), then in order to avoid complications and exacerbations, the gallbladder is almost always removed.
In case of pancreatitis, the need for such surgical intervention is due to the fact that disruption of the normal bile outflow and outflow of pancreatic juice leads to the fact that bile enters the ducts of this organ, and the secretion of the gland stagnates in them.
This leads to “self-digestion” of this secretion, which is fraught not only with the occurrence of an inflammatory process in the tissues of the gland, but also (which is much more dangerous) in advanced cases can cause necrosis - the death of organic cells of pancreatic tissue with a complete loss of their functionality (without the possibility of recovery) .
How does gallbladder removal affect the pancreas?
After surgery to remove the gallbladder, most people experience a noticeable improvement in their general condition. Pancreatitis ceases to manifest itself over a long period of time, moving into a stage of prolonged remission. The so-called “cholelithiasis pancreatitis” can only worsen when drinking alcohol-containing drinks or if the diet is violated.
Many people lead normal lives after undergoing surgery to eliminate the bladder, and the key to their success is a diet that completely excludes alcoholic beverages and foods with a high percentage of fat.
Consequences of the operation
If pancreatitis is a consequence of cholelithiasis, then cholecystectomy can improve the general condition, remission will last longer, and the intervals between periods of remission will decrease. This usually happens when the operation was successful and was performed in the initial stage, when the disease has not yet advanced.
Then the elimination of bile duct obstruction caused by the presence of stones helps to improve the health of the pancreas. The function of pancreatic juice secretion returns to normal in 62.55% of patients.
Timely surgery leads to recovery in more than half of cases
But in many cases, after surgery to remove the gallbladder, a syndrome called postcholecystectomy may appear.
Typically this condition develops for the following reasons:
- incorrectly chosen tactics of the operation or errors during its implementation;
- disorders in the functions of individual organs after removal of the gallbladder;
- existing liver diseases;
- adaptive restructuring of the digestive system with the possible formation of pathologies after cholecystectomy.
With the development of postcholecystectomy syndrome, chronic pancreatitis is often associated. Although no exact figure can be given, the detection rate varies widely from 5% to 90%.
Postcholecystectomy syndrome can occur both after abdominal and after laparoscopic surgery, if errors were made during the intervention
The occurrence of pancreatitis after cholecystectomy
The development of pancreatic pathology in the pancreatic cavity after cholecystectomy can only be observed in the event of a violation of dietary nutrition, consumption of foods on the exclusion list, and drinking of alcoholic beverages.
The cause of an acute attack of pancreatic pathology may be the bile ducts taking over the functionality of the removed bladder. During this process, bile enters the intestinal cavity in small portions, and not as before - when bile entered in large quantities. Such changes provoke a decrease in the bactericidal properties of bile and changes in the microflora in the intestinal cavity, which leads to the formation of diarrhea, heartburn and constipation. Such changes begin to have a negative impact on the functionality of all internal organs included in the digestive tract system, including the pancreas.
A disrupted diet with chaotic consumption of prohibited foods and drinking alcohol-containing products will soon after cholecystectomy lead to the development of inflammation in the cavity of the parenchymal organ, called pancreatitis.
Treatment of pancreatitis with removed gallbladder
By ensuring proper diet, treatment methods for pancreatitis after gallbladder removal involve minimal use of medications. In hospital settings, for three days after surgery, antibacterial therapy is carried out using drugs with an antibiotic spectrum of action.
Taking analgesic and antispasmodic drugs will help eliminate painful symptoms; Drotaverine or Buscopan is prescribed. And also to prevent the formation of stones in the pancreatic cavity, the drug Ursolfac is prescribed for half a year to 2 years.
What happens after surgery?
There is a misconception that the pancreas takes on too much of the load from the gallbladder after it is removed. However, it is not. If inflammation is a consequence of the growth of stones, then after removal of the organ, stable remission and complete cure of pancreatitis may occur. Most patients have normal secretion of enzymes and pancreatic juice after surgery.
If the operation was performed with some deviations, a complication in the form of postcholecystectomy is possible. As a rule, its causes can be:
- liver dysfunction;
- disruption of the functioning of internal organs (in particular, the gastrointestinal tract);
- mistakes made during the surgical intervention itself;
- global changes in the functioning of internal organs as a result of abnormal behavior of the gallbladder;
- the development of new organ lesions as the disease progresses.
Thus, the success of the operation largely depends on how long the disease has progressed and whether other pathologies have arisen against its background.
Diet for pancreatitis after removal of the gallbladder
Over the next 2 months of the postoperative period, pureed soups, as well as pureed vegetables boiled in water or stewed, can be used as food.
As drinks, it is allowed to use weak rosehip-based decoctions, weakly brewed green tea drink, and freshly squeezed juices must be diluted with boiled water in a 1:1 ratio.
What products are prohibited?
During the rehabilitation period, as well as after it, all types of dishes with a high percentage of fat content, spiciness and salt, as well as those prepared by frying, are prohibited from consumption.
Exceptions should also be:
- all types of fish,
- strong tea and coffee,
- alcohol,
- all confectionery and bakery products,
- all types of chocolate.
Nutrition
The quality and quantity of food plays a dominant role in the recovery process of all functions of the body of the operated person. Therefore, it is so important to strictly follow all nutritional recommendations:
- Cold food and liquids are contraindicated, as this can cause stomach cramps, which is not good in this case.
- Your diet should not include spicy, smoked, fried or fatty foods. They are also contraindicated for you. However, as well as products such as sweets, wine, vinegar, lard, concentrated broths and all kinds of syrups. The use of any of them, even in small quantities, can provoke pain (after removal of the gallbladder, such a symptom must be treated with extreme caution).
- The most suitable diet in this case is table No. 5.
Important! During the day you need to take about five to six meals of the recommended food. Moreover, each of them should be small in volume, since a significant amount of food entering the stomach is poorly digested.
If you continue to eat incorrectly, then do not ask your doctor a question about why your side hurts after removal of your gallbladder.
Is it possible to remove the gallbladder for pancreatitis?
It is important to remember that the development of cholecystitis can often be triggered by the progressive stage of pancreatic pathology in the pancreatic cavity. And then many patients are alarmed by the question of whether it is possible to cut out the gallbladder for pancreatitis?
The fact is that in such cases the issue of eliminating the gallbladder is not even discussed and is put on the priority list. This is due to the fact that accumulated stones prevent the outflow of bile, which leads to its penetration into the pancreatic cavity and activation of pancreatic enzymes, which trigger the process of self-destruction in the gland with the development of pancreatic necrotic lesions, characterized by the death of gland tissue, the restoration of which will no longer be possible.
Bibliography
- Yu.S. Polushin, A.V. Sukhovetsky, M.V. Surkov et al. Acute postoperative pancreatitis. St. Petersburg Folio, 2003, p. 158.
- Lopatkina T.N. Chronic pancreatitis: diagnostic problems, the role of biliary disorders and approaches to treatment. Wedge. Pharmacol. ter. 2004 No. 1, pp. 9–11.
- Plotnikova E.Yu., Gracheva T.Yu. The place of Trimebutine in the conservative treatment of sphincter of Oddi dysfunction. Attending doctor. 2018 No. 2.
- Ilchenko A.A., Bystrovskaya E.V. Experience with the use of Duspatalin for functional disorders of the sphincter of Oddi in patients who underwent cholecystectomy.
Diet after surgery for chronic pancreatitis
With chronic inflammation of the pancreas and cholecystitis, all patients must follow a certain diet in order to keep it at rest as much as possible and relieve the main symptoms. However, this rule is even more important in the case where a cholecystectomy has been performed.
Please pay attention to the following nutritional rules:
- eat fractionally and in small portions;
- increase the number of meals to six to seven per day;
- limit the consumption of unhealthy foods (fatty, too salty and sweet, spicy, sour);
- reduce the amount of canned food in the diet;
- give preference to boiled and baked foods;
- reduce the amount of chemicals;
- Avoid eating too hot or cold foods.
Take your last meal no later than two to three hours before bedtime. Overeating and consumption of foods that cause flatulence and fermentation are unacceptable. It is also important to reduce the amount of confectionery and refined baked goods in the diet. The diet for a removed gallbladder and pancreatitis should be as soft and gentle as possible.